Saarang Deshpande shared on X:
“As it is a global health issue reflective of health inequities, let’s discuss serum ferritin thresholds for iron deficiency (ID) and iron deficiency anemia (IDA).
Despite it being a well-described global health problem, we’re not as good as we could be at diagnosis of iron deficiency.
Inconsistent ferritin cut-offs for what constitutes iron deficiency vs sufficiency play a big role here.
Here are some examples of different cut-offs for serum ferritin:
15 – WHO
23.9 – Where I trained ‘reference’ LLN
30 – CDC and ACOG
50 – Some experts Inconsistent guidelines beget inconsistent care
A survey of PCPs shows that ~25% misinterpret iron studies showing ID! (and half underuse bidirectional endoscopy)
Wonder if inconsistent ferritin thresholds / reference ranges have anything to do with it??
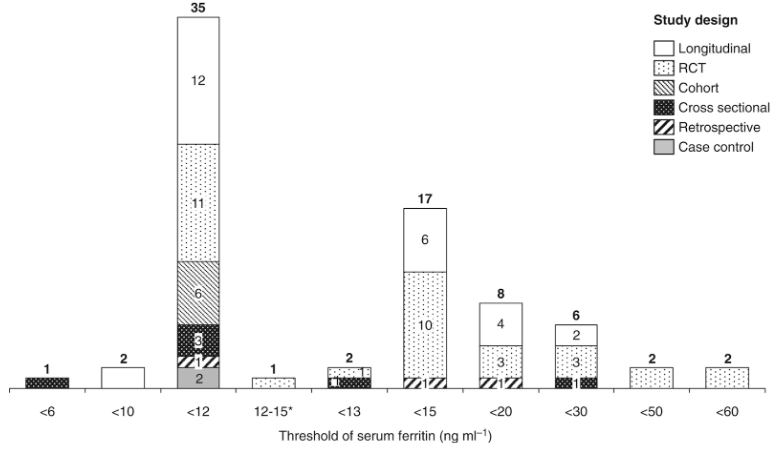
Inconsistent ferritin thresholds make synthesis of research difficult too. Most studies on ID in pregnancy use overly specific/restrictive thresholds (<12 and <15), mostly witho0ut justifying their ferritin cut-off.
Authors: J. Daru, J. Allotey, J. P. Peña-Rosas, K. S. Khan
When USPSTF concluded insufficient evidence to recommend ID screening in pregnancy, part of the reason was inconsistent ferritin thresholds — though there’s association between ID and maternal/neonatal outcomes.
The historical origin of our ferritin ‘reference range’ seems to come from bone marrow biopsies showing absent stainable iron stores correlating with ferritin <15 But BMBx studies also show absent / depleted (1+) iron stores in 30-50% of women!
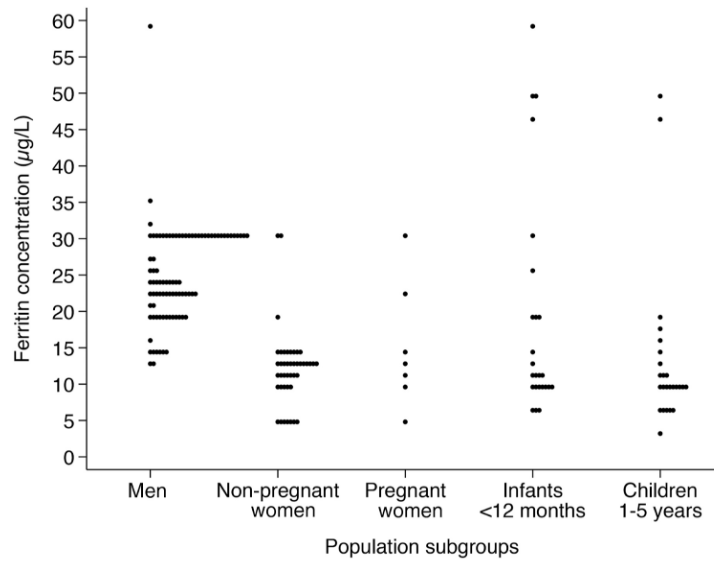
A systematic review of ferritin reference ranges showed a median LLN of 8 for females and 25 for males – a structural sex-based inequity And, the presumed ‘iron-sufficient’ are not excluded from having ID, biasing these ranges.
The origin of ferritin reference intervals: a systematic review | The Lancet Haematology
Authors: Judy Truong, Kanza Naveed, Daniel Beriault, David Lightfoot, Michael Fralick, Michelle Sholzberg

This review lists the many ferritin cut-offs. A salient quote: ‘evidence to support any recommended SF cutoff for diagnosis of ID is limited…15 μg/L is likely specific but can be expected to miss many cases of ID—perhaps as many as half.’
Authors: Jahnavi Daru, Katherine Colman, Simon J Stanworth, Barbara De La Salle, Erica M Wood, Sant-Rayn Pasricha
Current adolescent and young adult screening certainly appears to miss the mark on ID diagnosis: nearly 40% of adolescent and young females are iron deficient – sex-based inequity – as reported by Angela Weyand.
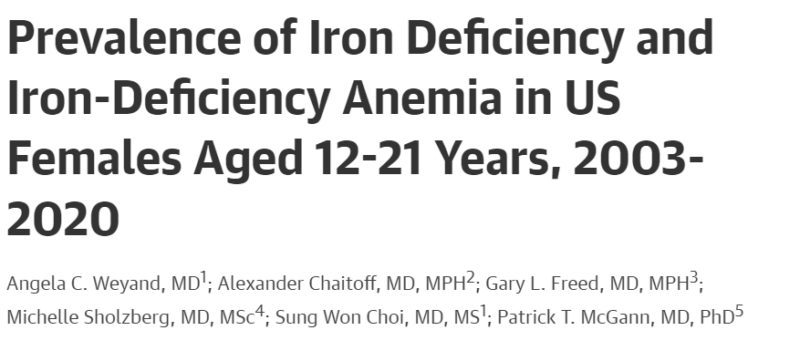
Likewise, females of lower SES have higher risk of being anemic but are the least likely to have ferritin checked when non-anemic – a compounded socioeconomic inequity – as reported by Angela C. Weyand and Michelle Sholzberg.
Authors: Sophia Wen, Rosane Nisenbaum, Angela C. Weyand, Grace H. Tang, Michael Auerbach, Michelle Sholzberg
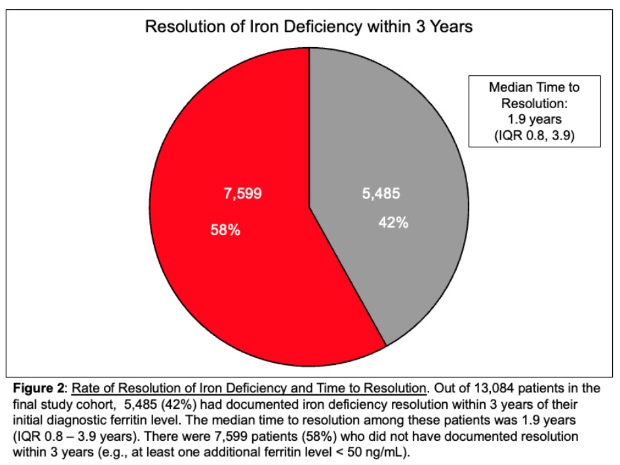
Diagnostic ambiguity may delay adequate treatment Most with documented ID still had it after 3 years, and for those who improved, median time to resolution was almost 2 years.
Authors: Jacob C. Cogan, Julia Meyer, Ziou Jiang, Michelle Sholzberg
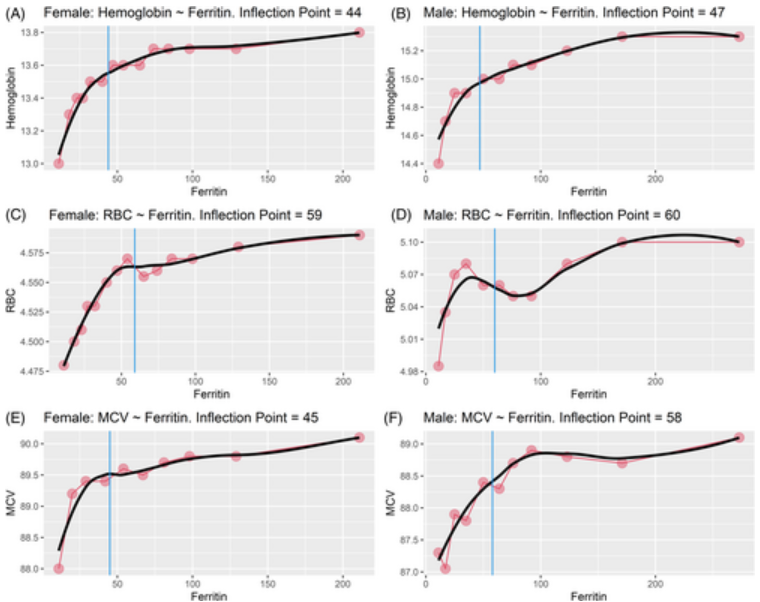
From an anemia perspective: the inflection point at which ferritin correlates with changes in Hgb, RBC count, and MCV is between 44 to 60
…essentially the same between males and females (and anemia is a late finding of ID!)
Authors: Robert T. Means Jr, Caixia Bi, Edward C. C. Wong, Lance A. Bare, Michael J. McPhaul
Big takeaways:
- Our ferritin thresholds lean specific rather than sensitive for case detection. As benefits of treating what we previously called ‘subclinical’ ID seem to outweigh harms of ‘over-treatment’ in borderline cases, I’d venture higher cut-offs are more sensible.
- Inappropriate laboratory reference ranges predicated on Gaussian distribution are not useful when ~40% of women are iron-deficient (and ~6% have IDA as well). Ferritin LLNs should be physiologic.
- Standardization of ferritin thresholds can facilitate dissemination of appropriate guidelines on Iron deficiency and further study and amelioration of its global burden.
I’ve limited my scope to ferritin thresholds, but there’s much more to be discussed re: inadequate care for heavy menstrual bleeding, malnutrition, sex-based Hgb reference ranges, accessibility of IV iron, etc end!
Check out these tweet(orial)s for more!
Angela Weyand on iron dosing.
Tony Breu on ID causing sx without anemia.
William Aird on non-anemic ID:
Source: Saarang Deshpande/X
More posts featuring Iron Deficiency on oncodaily.com
Saarang Deshpande is a Resident Physician at Penn Medicine, University of Pennsylvania Health System. He previously worked as a Research Assistant at Cornell University and completed internships at the American Psychiatric Association, VCU Health, and Johns Hopkins School of Medicine.