Geographic Variations and Risk Factors in Lung Cancer Incidence
Authors: Juan Carlos Laguna, Miguel García-Pardo, Joao Alessi, Carlos Barrios, Navneet Singh, Humaid O. Al-Shamsi, Herbert Loong, Miquel Ferriol, Gonzalo Recondo, and Laura Mezquita.
Published in: Therapeutic Advances in Medical Oncology, Sage Journals, March 2024
Introduction
Lung cancer is the second most diagnosed cancer and the leading cause of cancer mortality worldwide, with rates differing significantly by region. While tobacco smoking is the primary cause of lung cancer in many Western countries, other factors like environmental carcinogens and genetic predispositions also contribute, especially in regions with a higher prevalence of non-smoking-related cases. Non-small-cell lung cancer (NSCLC) accounts for the majority of cases, and distinct genetic mutations seen across different geographic areas influence treatment approaches and outcomes.
Design and Methods
This study examines lung cancer incidence and key risk factors across various geographic regions, analyzing data to understand the prevalence of NSCLC and identifying environmental and genetic factors that contribute to these regional disparities. Data collection included epidemiological studies, mutation analyses, and cancer registries from regions across North America, Latin America, Asia, MENA (Middle East and North Africa), Sub-Saharan Africa, Europe, and Oceania.
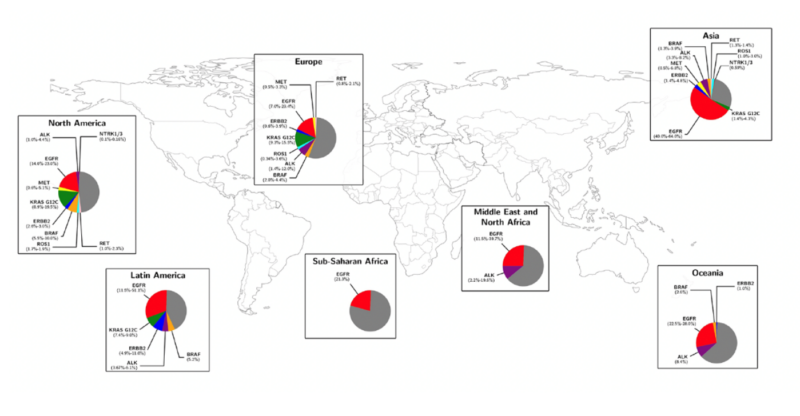
Above is presented the global distribution of main actionable genomic alterations in non-small-cell lung cancer.
What We Learned: Key Highlights
- North America: Lung cancer remains a leading health issue, with significant incidence among women. Tobacco, radon exposure, and air pollution are major risk factors. African Americans demonstrate higher lung cancer rates, potentially due to genetic predispositions.
- Latin America: High lung cancer mortality rates, with tobacco, air pollution, and arsenic exposure as main contributors. Genetic studies reveal a high prevalence of EGFR mutations.
- Asia: Asia has the highest lung cancer rates globally, with particular non-smoking-related cases in women. Unique genetic mutations, such as EGFR mutations, are prevalent.
- Middle East and North Africa (MENA): Diverse lung cancer rates are impacted by high tobacco use, hookah, and environmental radon exposure. Genetic studies highlight regional predispositions, but limited molecular profiling restricts targeted treatments.
- Sub-Saharan Africa: Generally lower rates due to lower smoking prevalence; however, indoor pollution and occupational hazards, like mining dust, elevate risk, and limited healthcare resources contribute to poor survival outcomes.
- Europe: High mortality from lung cancer with rising smoking rates among women. Genetic variability and molecular profile access vary by region, impacting treatment options.
- Oceania: Significant disparities between Indigenous and non-Indigenous populations, with higher incidence in Indigenous groups and contributors like tobacco smoking and asbestos exposure. Molecular profiling access is highest in Australia and New Zealand.
Key Takeaways
- Tobacco Remains a Global Challenge: Smoking remains a dominant risk factor worldwide, though its impact varies by region.
- Non-Smoking-Related Cancers: Rising cases in non-smokers, particularly among women in Asia, underscore the importance of addressing genetic and environmental factors.
- Genetic Mutation Variability: EGFR mutations are more prevalent in Asian populations, influencing treatment approaches and the need for molecular profiling.
- Access to Molecular Profiling: Disparities in access to profiling limit personalized treatment options, especially in regions like MENA and Sub-Saharan Africa.
- Environmental Carcinogens: Radon, air pollution, and occupational exposures contribute significantly to lung cancer risk beyond smoking, with regional variations.
Future Directions
- Increased Access to Molecular Profiling: Expanding molecular profiling capabilities in underserved regions could enable more personalized treatment and improve outcomes.
- Targeted Prevention Campaigns: Region-specific interventions focusing on smoking cessation, radon mitigation, and air pollution reduction are essential.
- Genetic Research Initiatives: Research into genetic predispositions across diverse populations could aid in the development of targeted therapies and preventive strategies.
- Improved Healthcare Infrastructure: Enhancing diagnostic and treatment resources, especially in low-resource settings, is critical for early detection and better lung cancer management globally.
Find More “Paper Alerts” on OncoDaily.


