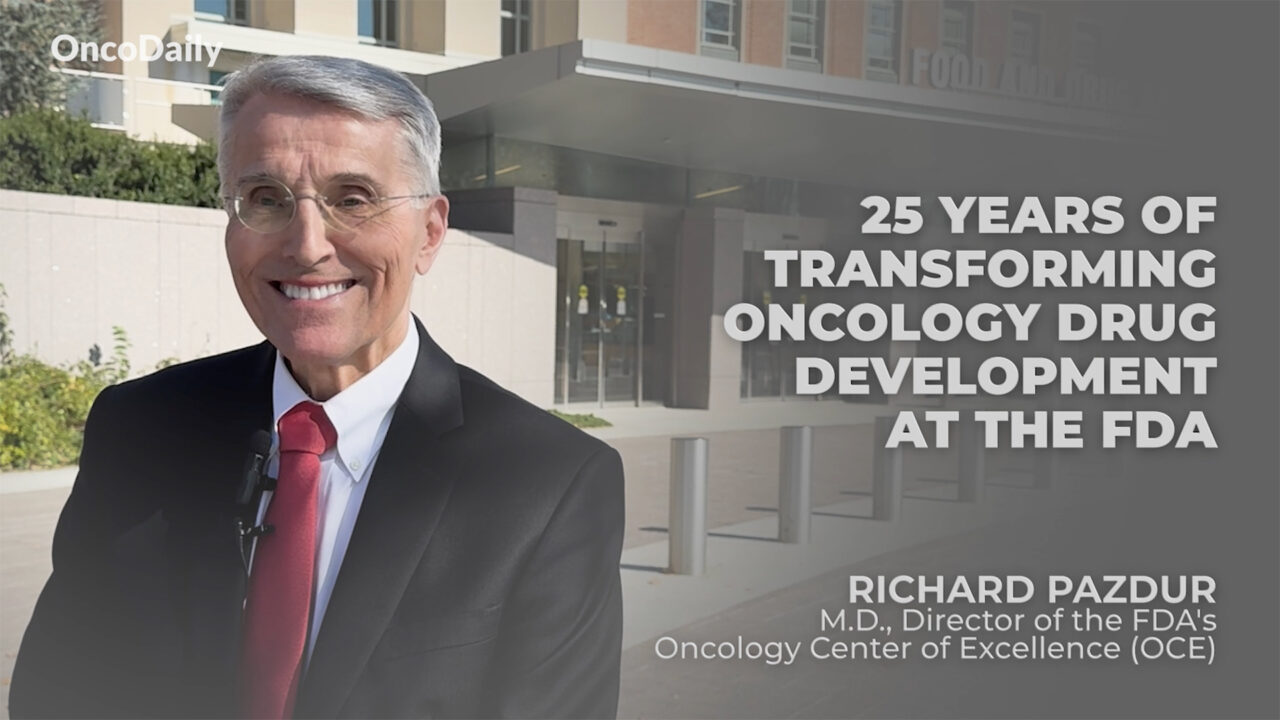
In a career that spans nearly half a century in oncology, including 25 years at the FDA, Dr. Richard Pazdur has redefined the agency’s role in oncology drug development. As the director of the FDA’s Oncology Center of Excellence (OCE), he has overseen revolutionizing changes in the development of oncology drugs, fostering a transformative impact on medical oncology.
This interview captures Dr. Pazdur’s reflections on his legacy, the evolution of oncology, his approach to mentorship, and his insights on future challenges and opportunities in the field. Dr. Richard Pazdur’s 25 Year WAR on Cancer at the FDA!
Richard Pazdur is the Director of the FDA’s Oncology Center of Excellence (OCE), where he oversees the coordination of oncology product reviews. He joined the FDA in 1999 as Director of the Division of Oncology Drug Products and led the 2005 consolidation of cancer and hematologic review divisions into the Office of Hematology and Oncology Products (OHOP). In 2019, OHOP became the Office of Oncologic Diseases (OOD), where he currently serves as acting director.
I practiced medical oncology for over 25 years, so I had really a good appreciation for the care of patients with malignancies. So I’ve had that experience. During the period of time that I was in academic medicine, I spent a great deal of my time on drug development, both in the early drug development, phase one studies, but also in GI malignancies.
I came to the FDA, and I realized the importance that the FDA had in shaping the drug development program of the world, basically. And I think it’s very important for people to realize that when a job came open such as this, I saw the opportunity, and I also saw the opportunity of how to change the FDA into a much more integrative, a much more interactive part of the oncology really community. So we had many programs aimed at community outreach, interactions with academic groups, with professional groups such as ASCO, AACR, ASH.
So there’s been a great deal of interaction. And this also breeds, basically, interest by our reviewers because they are integrated into really the general oncology community and not just separated into a regulatory aspect. Well, I would never have imagined that I would be here.
I always tell people nobody goes to medical school and writes on their medical school application that they’re going to go work at the FDA. I’ve never met anyone that did that. And so all of us have had that work here at the FDA have had a relatively circuitous route.
I’ve had a varied career in medical oncology, and I think it’s important for people to realize that when I entered the field of medical oncology, it was relatively a very young discipline, okay? As I stated before, we only had a few drugs. They were all cytotoxic therapies.
It was really a discipline in its infancy. When I was in high school, I knew I wanted to become a physician, and I really thank my parents really for nurturing that interest. I like the combination of science and the care of patients.
I originally was not planning to become an oncologist. My first aspiration when I entered medical school was to become a psychiatrist. I changed.
I thought I would be a cardiologist. In fact, I was all signed up for a cardiology fellowship and actually did a stint in the cath lab and said, I really don’t want to do this for the rest of my life. So I happened to take my last rotation as an internal medicine resident in the area of oncology, and I really found the people that were working in the field and the field itself as really one that really was subject to a great deal of growth.
You know, in 1979, I had a much different opinion of what oncology would become. I thought oncology would be primarily an academic discipline with very few people treated in the community. I thought that most of the drugs would come from the NCI and the pharmaceutical companies would have very little interest in developing drugs.
And obviously, I was quite wrong. Obviously, the vast majority of patients in the United States are treated in the community, and as you pointed out, over 40 percent of pharma activity is now in this area. So I was wrong, but there are certain forces that we don’t know at a specific time that could really impact the field.
I think we have approved many drugs that really were transformational during this 25-year period of time. Many of them have really revolutionized the practice of medical oncology. I always look back at the times when I was just beginning oncology, and that was in 1979, when we only had about 35 to 40 oncology drugs.
And now, almost every year, we approve somewhere between 10 to 15 new molecular entities for the treatment of the diseases that are classified as oncology diseases. I think it’s important to see diseases that have been transformed during this period of time in the past 25 years. Diseases such as multiple myeloma, where the life expectancy has been greatly increased.
Melanoma, where again, the life expectancy has been increased. Novel therapies such as CAR-T cells, the rebirth of cancer immunology with the PD-1 drugs, the checkpoint inhibitors, which really revolutionized, really, the treatment of oncological diseases. Well, there are certain aha moments, okay, in medical oncology, where you really do see true breakthrough therapies.
Here again, when we were looking at the treatment of CML, throughout the vast majority of my career, before imatinib came out, basically, we were controlling the counts of patients with CML, and actually just monitoring the natural progression of the disease. But we really saw a major sea change in the treatment of CML with the introduction of the tyrosine kinases and the subsequent drugs that came after imatinib. So, it’s an aha moment, you realize that there is a true magic here, so to speak.
It is somewhat of a bitter, sweet moment, because again, we see these major advances. But as somebody that has treated patients with this disease, okay, and they did not have this drug, and we see their faces in my mind, that they, just by chance, were not here at the time when this drug was developed. It’s somewhat not hurtful, but disappointing that they did not have the advantage of being and receiving these drugs.
So, it’s kind of a bittersweet issue here, one of having these breakthrough therapies, but then also realizing that some of the past generations of patients did not have access to these drugs. My legacy is the people that work for me. We here at the FDA are only as good as the people that are working in the review divisions here at the FDA.
When I first started in 1999, 25 years ago, there were about 10 medical oncologists. Now, we have over 100 medical oncologists. And what we did over this period of time is really take the oncologists that work for us and really place them in disease-specific areas and disease-specific teams.
So, similar to cancer centers in other academic areas, we have a group of physicians that work in breast cancer, lung cancer, pediatric malignancies, hematological diseases, and these are broken down, obviously, into multiple myeloma, acute leukemia, other diseases. But really, we recognize that it was very important, really, to have physicians that are highly specialized in these diseases. The diseases, obviously, became much more complicated, complex regarding what is being involved, what is the current treatment landscape in each of these diseases.
I’ve had many, many mentors. One of my mentors was Dr. Phil Bonomi from Rush Presbyterian St. Luke’s Hospital in Chicago. He recently retired.
He was one of the most excellent clinicians that I have ever seen. He really understood what patients want and really demonstrated a degree of clinical judgment that many times, I think, might be lacking in modern-day clinicians that view the practice of medicine as being following guidelines, et cetera. And I’m not trying to minimize the importance of guidelines, et cetera, but many times, one has to use judgment, so to speak.
There’s a difference between, obviously, knowledge and wisdom, okay, and Phil truly had wisdom. Well, the most important thing is the foundation of the Oncology Center of Excellence here at the FDA. This was the FDA’s initiative for the Moonshot Program when it was initiated more than five years ago, and I think it’s a lasting tribute to the Moonshot Program to have set up the Oncology Center.
It really gave oncology a presence here in the agency, additional resources to develop the many programs that we have developed in international outreach, in community outreach to underserved populations here in the United States, as well as really solidifying the interest of our staff in developing their careers and staying at the FDA.
One of my thrills is to see my people succeed, and they could succeed not only here in the FDA, but also when they leave the FDA, if they choose to do so, in the pharmaceutical world, in the academic world. When people come and tell me that they’re leaving the FDA, I think they expect me to say, please stay, don’t leave.
I just ask them one question, or one statement, make sure you’re leaving for something and not away from something. Move toward an opportunity rather than moving away from something, and I think that that has always been something that I have incorporated in my life. I really have to tell people that I had a varied career in academic medicine and patient care before I came to the FDA, so I can’t discourage people from having other careers and other opportunities.
But here again, you need to have a vision when you go into a job of what you want that job to be, how you’re going to mold that job, what advantages is it going to be for you. Again, leave towards something, not away from something. I think in the next 5 or 10 years, we’re really going to see a growth of tumor immunology.
Here again, one of the major pivotal areas that we saw in the last decade was the introduction of the checkpoint inhibitors, and as you can see, they have had a tremendous impact on the treatment of patients with oncological diseases with some of the drugs having over 40 indications. They range from the treatment of head and neck cancer, lung cancer, hematological diseases, so they’ve had a major, major impact.
What we’re also going to see, and we’re seeing this already, is the introduction of these therapies that were initially developed in the advanced disease setting moving forward into the neoadjuvant and adjuvant setting, and this obviously offers a chance for cure to patients with these malignancies.
Well, I think when you see innovation, particularly in one area, and success in one area, success follows success. We’ve seen, for example, in diseases such as multiple myeloma, renal cell carcinoma, the subsegmenting of lung cancer into various types of lung cancer based on both immunological markers as well as targeted therapies in this disease, that really the most important thing is understanding the underlying biology of the disease and how these diseases are different, okay? And most of our advances that have occurred in this field were really based on understanding the basic science of diseases.
For example, when I started oncology, lung cancer was divided into small cell lung cancer and non-small cell lung cancer, and now we realize that there are many more markers here, biomarkers, different targets that people can look at and develop drugs. So really, the major issue is not the clinical development of the drug, but really the basic science that underlies these drugs and really investing money and resources also in the basic science of oncology. Well, we here at the Oncology Center of Excellence have a large, large international program.
One of the programs that we have developed is called Project Orbis, which attempts really to encourage applications to be reviewed with various countries and the U.S. FDA at the same time. So members of these include not only Western Europe, but also Israel, Brazil, Australia, Canada, many countries that are involved, the U.K. also, and Japan and the E.U. is also involved. One of the important issues is realizing and really telling companies that we really want to have a global presence for drug development.
We here in the United States are a diverse population, okay, and when we talk about diversity, we have to be cognizant that some of this information may come from outside of the United States, and hence we really encourage sites to be developed in Central America, where we have a vast population coming into the United States, and also some Sahara Africa, where we could really get clues to the intrinsic challenges of drug metabolism, of how drugs are handled differently in various ethnic populations.
I think really having a global population in a clinical trial representative of the entire global population will help us here in the United States because we are a country that is quite diverse and really needs this information. Here in the United States, we only have about 20% of the accrual in oncology, so we really rely and have to have a reliance on trials that are done on an international level. They give everybody more confidence that these results can be extrapolated to the diverse population here in the United States, as well as rapidly bringing medications to these other countries.
Well, there’s been a great deal of effort in the United States and in Europe to encourage pediatric development through various legislative initiatives. Basically, these have focused on taking drugs that have been developed and investigated in adult malignancies and then exploring them in childhood malignancies. We have to be cognizant that these diseases are different from what we see in the adult malignancies, with few exceptions.
However, I think one of the things that we should take a look at is potentially looking at drugs specifically aimed at childhood malignancies rather than trying to repurpose drugs that have already been developed in adult malignancies. What’s the role of media? It’s a very important role.
I think it’s very important to realize because oncology is a very, very rapidly growing field that we incorporate media really to educate patients. This is a very important issue. I’m talking about really understanding the value of a drug and putting that therapy into the context of current treatments.
Many times when I was in practice, I saw patients come with requests for treatments that were totally inappropriate because they really didn’t understand the context where these discoveries were developed. For example, they came in asking for drugs that were simply used on animals, were never used in patients before. Here again, people have to have a knowledge.
This is, I think, where one of the major challenges for the media is how to put these new therapies into context for individual patients. Also, it’s very important that patients listen to their physicians and be partners with their physicians in their care. Here again, I think this partnership is a vital one.
It’s not about getting multiple opinions about a disease. Ultimately, when one is facing a disease, one has to have a captain of the ship and one has to have trust in the physician that is prescribing their medication and taking care of them. I have many, many books because I read a lot.
I’ll tell you one that we had actually the author come to the FDA. We have a series called Meet the Press, a parody of the NBC program where we bring in journalists. This book was called For Blood and Money.
The author is Nathan Vardi. What it did was explain what was going on with the DTK inhibitors and their development behind the scenes in the drug company. I really wanted the author to come because, first of all, we were mentioned in it, but more importantly, we see things from across the table when the companies come and see us.
We don’t see what goes on behind the scenes. I think that this was extremely important to really have that view of what goes on with the finances of company, how decisions are made, how decisions are not made, how decisions are prioritized. The author did really an excellent job really giving a very colorful story of what was going on behind the scenes.
That’s one book. My favorite author is Doris Kearns Goodwin, one of the other authors that I read a lot. She’s a historical presidential scholar.
She’s written many books, one on LBJ, which I read recently, the other, Lyndon Baines Johnson. The other is regarding World War II, No Ordinary Time, regarding what was going on in the White House during World War II. Excellent writer.
Recently wrote a book regarding her life story with her husband, which is also just a very sentimental and really impactful book to read.
For more information visit oncodaily.com