The Institute of Cancer Research shared a post on LinkedIn:
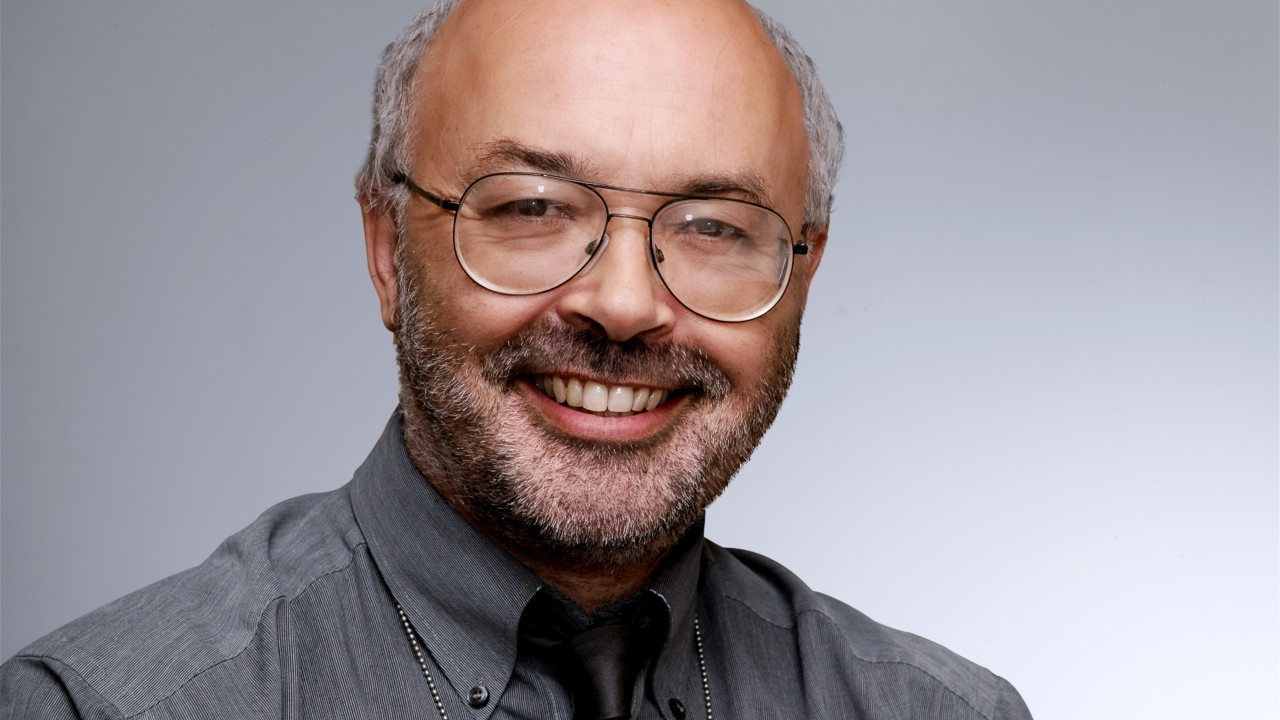
“Over the last four decades, radiotherapy has seen a technological revolution – evolving from broad, relatively simple deliveries to highly targeted, patient-specific treatment. Few individuals have played a more pivotal role in its transformation than Emeritus Professor Steve Webb, former Head of the Joint Department of Physics at The Institute of Cancer Research, London, and The Royal Marsden NHS Foundation Trust.
From his early work on computed tomography (CT) imaging to becoming one of the so-called ‘Founding Fathers’ of intensity-modulated radiotherapy (IMRT), Professor Webb has helped reshape how radiation is delivered – making it more precise, more effective and more humane.
Professor Webb reflected on his entry into a medical physics career, the innovations that changed cancer care and the challenges that remain, with Robbie Lockyer.
The birth of IMRT
In 1989, at The Institute of Cancer Research (ICR), Professor Webb used mathematical optimisation to improve medical imaging in nuclear medicine by finding the best possible settings through iterative adjustment – a method called simulated annealing. When he moved to the radiotherapy group, he realised the same approach could be used to shape radiation doses more precisely around tumours.
The result was intensity-modulated radiotherapy (IMRT), a technique that allows the intensity of the radiation beam to be varied as the machine rotates around the patient. This made it possible to more precisely wrap the dose around the tumour while avoiding surrounding healthy tissue.
Professor Webb said: ‘I often compare it to cling film. You want that radiation dose to wrap around the tumour, like cling film around cheese, but avoiding damaging the healthy structures nearby.’
IMRT was not the invention of a single individual – like most breakthroughs in science, it was developed concurrently by several individuals internationally including at the Memorial Sloan Kettering Cancer Center in the US, the DKFZ German Cancer Research Center in Heidelberg and the The Netherlands Cancer Institute. Back in 1989, only a handful of researchers worldwide were exploring the concept, with Professor Webb at the ICR and The Royal Marsden, being the first in the UK to pursue this approach.
Among the most influential contributions to IMRT was Professor Webb’s 1989 paper, published in Physics in Medicine and Biology, which laid out the foundation for inverse planning – the process of calculating how to shape and modify radiation beams to match a prescribed dose distribution. The paper remains a cornerstone in the field and became his most cited, earning invitations to speak around the world and drawing the attention of researchers and manufacturers alike.
From theory to global standard
Professor Webb said: ‘My early lectures on IMRT were entirely theoretical, including one I gave at the World Health Organization in Geneva in 1992. I remember saying that it couldn’t yet be done in practice as we didn’t have the technology. The next speaker got up and showed a working prototype. That was a wake-up call!’
In the US, the NOMOS Corporation began clinical treatments using Professor Webb’s planning methods, which were publicly available in peer-reviewed journals and free to use, dominating the field of IMRT until 1997.
In 1994, the company Elekta, which manufactured accelerators – machines used to administer radiotherapy beams – got interested in IMRT and formed the Elekta International IMRT Consortium. The group, working to adapt standard radiotherapy machines for IMRT delivery, comprised of eight individuals at first, turning to 20 in 2000, including Professor Webb.
In September 2000, the ICR and The Royal Marsden team became the first internationally to treat prostate cancer patients with IMRT – a milestone that marked its true clinical launch.
Professor Webb said: “I remember The Royal Marsden treated its first IMRT patient and it made all the national newspapers, such as The Guardian. One headline claimed we had ‘bent X-rays,’ which isn’t quite right – but it got the idea across.
‘Professor David Dearnaley was instrumental in launching this with the Physics and Radiotherapy Teams (led by Professor Alan Horwich) funded by Cancer Research UK (CRUK) and radiographer support from Professor Helen McNair.’
Professor Paul Workman, Harrap Professor of Pharmacology and Therapeutics and former Chief Executive of the ICR between 2014 and 2021, said: ‘By the time Professor Webb retired in 2011, IMRT had become the global standard for treating a range of cancers, including my own. It’s estimated that millions of patients globally have benefited from Professor Webb’s co-invention of IMRT.
‘It remains one of the most impactful pieces of applied medical physics in modern cancer care and underpins the precision of technologies such as the MR Linac – technology that combines magnetic resonance imaging (MRI) and radiotherapy allowing the clinical team to see real-time images of tumours and tailoring the radiotherapy delivery to maximum the dose to the tumour and minimise the dose to surrounding normal tissue.’
Reducing unwanted side effects
IMRT wasn’t just a technical triumph; it also made treatment gentler for patients. The bladder and rectum could now be avoided during radiotherapy for prostate cancer, reducing unwanted side effects such as urinary problems and bowel irritation. Equally, for head-and-neck cancers, the salivary glands could be spared, which meant patients didn’t lose the ability to eat or speak comfortably.
Professor Webb said: ‘Clinical trials led by ICR researchers, including Professor Chris Nutting and Professor John Yarnold, confirmed these benefits. We finally had the data to show that it worked – not just in theory, but in the livelihoods improved.’
The challenge of motion
Despite its proven success, IMRT isn’t perfect. One of the remaining challenges is treating tumours that move during treatment, particularly those in the lungs.
Professor Webb said: ‘While tumours in the prostate, for example, are relatively static, lung tumours can move with every breath. We’ve tried approaches like gating – where radiation is timed to the patient’s breathing – or using devices like the CyberKnife, a robotic system that tracks and adjusts for tumour movement in real time’.
‘However, we’re still lacking a widespread, elegant solution. Yet technologies like the MR-Linac, which allows for real-time imaging during treatment, offer promise’.
In the 2000s, Professor Webb’s research focused on more precisely defining the shape of the high-dose radiotherapy volume and modulating dose delivery across the tumour. These advances were crucial for not only improving tumour targeting but also for reducing off-set radiation to surrounding healthy tissues and managing tumour movement more effectively.
His 2005 paper, published in Physics in Medicine and Biology, proposed a new way to adjust radiation beams in real time to account for the natural movement of soft tissues using a modified dynamic multileaf collimator – a method for shaping and steering radiation beams with high precision.
Imaging the invisible
Long before the development of IMRT, Professor Webb was helping lay the groundwork for modern radiotherapy through his pioneering work in imaging technologies. For the first 15 years of his career, Professor Webb built a CT scanner for breast imaging when available commercial models had a too-small limiting aperture and published a book in 1990, From the Watching of Shadows, on the history of CT imaging and earlier pre-CT body-slice imaging.
The arrival of CT scanning in the 1970s and 80s was a breakthrough for radiotherapy planning allowing clinicians to create a three-dimensional map of the human body for the first time. Until then, everything was based on 2D x-rays, which made it hard to pinpoint tumours. Later, positron emission tomography (PET) and MRI further enhanced treatment planning by offering functional and metabolic insights, helping clinicians identify not just the location of but the behaviour of tumours.
Professor Webb said: ‘CT only shows you anatomical changes, MRI shows function and PET will show you functional imaging. Now, no radiotherapy treatment plan is created without some form of tomographic imaging, allowing clinicians to tailor treatment plans.’
During this period in 1997, Professor Webb authored The Physics of Conformal Radiotherapy, a widely referenced book that helped define technical best practice in the emerging field.
Cosmic rays to cancer care
Professor Webb’s journey into medical physics, and specifically radiotherapy, wasn’t part of a linear plan. Originally training as a physicist working on cosmic rays – particles from outer space travelling across the universe – at Imperial College London, he had what he calls a ‘Damacus moment’ while waiting for a train at Didcot Railway Station in the mid-1970s.
Professor Webb recalled: ‘I realised I didn’t want to spend my life on something I didn’t necessarily align myself with. A colleague and friend moved into medical physics at the Middlesex Hospital, and I soon arranged a week to shadow him, and that’s all it took. I knew then after the week it was the right decision.
‘An unconventional interview at the ICR followed after a job posting in The Sunday Times. I received a phone call with the then Head of Medical Physics asking me to come in that very afternoon and by that evening, I had been offered a job. There was no HR, forms or vetting – a very different process from today!’
Decades of science and collaboration
Collaboration was a hallmark of Professor Webb’s work throughout his career. He taught across Europe, co-ran IMRT training schools in Germany and held a visiting chair at the German Cancer Research Centre in Heidelberg – a partnership that spanned more nearly two decades.

Professor Webb said: ‘Many of the best people I worked with at the ICR weren’t British – they came from all over. International collaboration, even to this day, remains essential.’
In 2016, Professor Webb was made an Honorary Member of the German Society for Medical Physics (DGMP) – the only non-German to have received the honour. His honorary lecture given that year to the DGMP remains a valuable retrospective on the international development of IMRT. It offers a full account of the decades of science and collaboration that went into a technique now used around the world every day.
Professor Webb is also one of only three recipients of the European Federation of Organisations for Medical Physics (EFOMP) Silver Medal, awarded by EFOMP for exceptional contributions to the field.
Professor Webb said: ‘When asked what I’m most proud of, I don’t hesitate. We made something complex work and it made a difference to patients. That’s what matters.’
From early imaging systems to game-changing cancer treatments, Professor Webb’s career is a story of transformation – for physics, for patients and for the field of radiotherapy itself.”
More posts featuring The Institute of Cancer Research