Schwannoma in Children: What patients and caregivers should know about
Introduction
Pediatric schwannomas are rare, benign tumors originating from Schwann cells, which form the myelin sheath around peripheral nerves. These tumors can occur in various parts of the body, including the head, neck, and extremities, and are often associated with genetic conditions such as Neurofibromatosis type 2 (NF2). Despite their benign nature, they can cause significant morbidity due to their location and potential to compress adjacent structures.
Prevalence and Epidemiology
Schwannomas are relatively rare in the pediatric population. They constitute about 5-10% of all intracranial tumors and are even less common in the spinal region, representing only 2.5-4% of pediatric spinal tumors. The incidence of vestibular schwannomas (one of the most common types), is significantly lower in children compared to adults, with most cases occurring sporadically or in association with NF2.
Common Types
- Vestibular: These tumors arise from the vestibular nerve and are the most common type of schwannoma in both adults and children. They often present with hearing loss and tinnitus.
- Spinal: These tumors occur along the spinal cord and can cause neurological deficits due to compression of spinal nerves.
- Peripheral: These can occur in any peripheral nerve and are often found in the head, neck, and extremities.
- Other Cranial Nerve Schwannomas: These include the trigeminal, facial, and hypoglossal nerves, which can cause specific neurological symptoms depending on the affected nerve.
Causes and Risk Factors
The exact cause of these tumors is not well understood, but several risk factors have been identified:
- Genetic Mutations: Mutations in the NF2 gene (encodes a tumor suppressor protein) on chromosome 22 are a significant risk factor, particularly for vestibular schwannomas.
- Neurofibromatosis Type 2 (NF2): This genetic disorder is strongly associated with the development of multiple schwannomas, including bilateral vestibular schwannomas.
- Radiation Exposure: Prior exposure to radiation, particularly in the head and neck region, has been linked to an increased risk of developing schwannomas.
Symptoms
The symptoms of pediatric schwannomas vary depending on the tumor’s location and size. Detailed symptoms include:
Vestibular Schwannomas
- Hearing Loss: Progressive, unilateral hearing loss is the most common symptom.
- Tinnitus: Ringing or buzzing in the ear.
- Balance Issues: Dizziness and unsteadiness.
- Facial Numbness or Weakness: Due to compression of the facial nerve.
Spinal Schwannomas
- Back Pain: Persistent pain in the affected region.
- Neurological Deficits: Weakness, numbness, or tingling in the limbs.
- Bladder and Bowel Dysfunction: In severe cases, due to spinal cord compression.
Peripheral Schwannomas
- Visible Mass: A painless or painful lump that grows slowly over time.
- Tinel Shock: An electric-like shock when the affected area is touched.
- Motor and Sensory Deficits: Depending on the nerve involved.
Other Cranial Nerve Schwannomas
- Trigeminal Schwannomas: Facial pain, numbness, or weakness.
- Facial Schwannomas: Facial muscle weakness or paralysis.
- Hypoglossal Schwannomas: Difficulty swallowing and tongue movement issues.
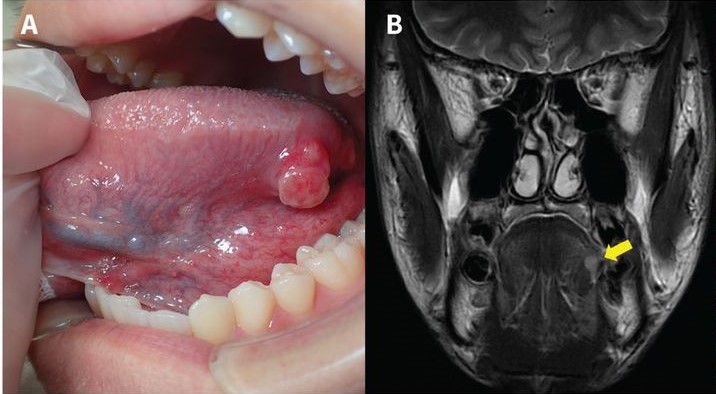
Tongue schwannoma in a 17-year-old boy. A magnetic resonance imaging scan reveals a well-defined lesion in the tongue. The image is taken from a paper authored by Ohta and Yoshimura (2021).
Diagnosis
Diagnosing pediatric schwannomas involves a combination of clinical evaluation, imaging studies, and histopathological examination.
Clinical Evaluation
The initial step in diagnosing pediatric schwannomas is a thorough clinical evaluation. This includes taking a detailed medical history and performing a physical examination to assess symptoms and neurological deficits. Common symptoms that may prompt further investigation include hearing loss, tinnitus, balance issues, back pain, and neurological deficits such as weakness or numbness in the limbs.
Imaging Studies
Imaging studies are crucial for the accurate diagnosis and localization of schwannomas. The primary imaging modalities used are:
- Magnetic Resonance Imaging (MRI): MRI is the preferred imaging technique for detecting schwannomas due to its superior soft tissue contrast. It provides detailed images of the tumor and its relationship with surrounding structures, which is essential for surgical planning. MRI with contrast enhancement can help differentiate schwannomas from other types of tumors and cysts. Schwannomas typically appear as well-defined, enhancing masses on MRI scans.
- Computed Tomography (CT) Scan: CT scans are useful for evaluating bone involvement and are particularly helpful in cases where MRI is contraindicated. They provide detailed images of the bony structures and can help identify any bone erosion or remodeling caused by the tumor.
- Ultrasound: In some cases, particularly for peripheral schwannomas, ultrasound can be used as an initial imaging modality. It helps in identifying the location and size of the tumor and can guide fine-needle aspiration biopsies.
Histopathological Examination
A definitive diagnosis of schwannoma is made through histopathological examination of the tumor tissue. This involves:
- Biopsy: A biopsy is performed to obtain a tissue sample from the tumor. This can be done through fine-needle aspiration, core needle biopsy, or surgical excision, depending on the tumor’s location and accessibility. The tissue sample is then examined under a microscope to confirm the diagnosis.
- Immunohistochemistry: Immunohistochemical staining is used to identify specific markers that are characteristic of schwannomas. Schwannomas typically express S-100 protein (found in nerve and pigment-producing cells, serves as a marker for diagnosing conditions like melanoma and nerve disorders), which helps distinguish them from other types of tumors.
Additional Diagnostic Tools
- Electrophysiological Studies: Electrophysiological studies, such as nerve conduction studies and electromyography, can be used to assess the functional impact of the tumor on the affected nerves. These studies help in evaluating the extent of nerve damage and planning surgical intervention.
- Genetic Testing: In cases where schwannomas are associated with genetic conditions such as NF2, genetic testing may be recommended. This involves analyzing the NF2 gene for mutations that predispose individuals to developing schwannomas.
Treatment Options
The treatment of pediatric schwannomas involves a multidisciplinary approach tailored to the individual patient’s needs, considering factors such as tumor location, size, symptoms, and overall health.
Surgical Treatment
Surgery is often the primary treatment for schwannomas, especially when the tumor is causing significant symptoms or is accessible without undue risk to critical structures.
- Microsurgical Excision: This is the standard approach for most schwannomas, allowing for precise removal of the tumor with minimal damage to surrounding tissues. The goal is to achieve complete resection while preserving nerve function. For vestibular schwannomas, the retrosigmoid approach is commonly used, which provides good access to the tumor while aiming to preserve facial nerve function.
- Minimally Invasive Surgery: Techniques such as endoscopic surgery are used for certain cranial nerve schwannomas. These approaches offer reduced recovery time and fewer complications by avoiding large incisions and minimizing disruption to surrounding tissues. For tumors near the skull base, endoscopic approaches through the nasal cavity can be employed, using advanced imaging and navigation systems to avoid critical structures.
- Surgical Management of Peripheral Schwannomas: Early surgical resection is recommended for peripheral nerve schwannomas causing significant pain or neurological deficits. This approach can lead to excellent functional outcomes and improved quality of life.
Radiation Therapy
Radiation therapy is a key treatment modality for schwannomas, particularly when surgery is not feasible or the tumor is located in a challenging area.
- Stereotactic Radiosurgery (SRS): SRS, including Gamma Knife and CyberKnife, is a highly precise, minimally invasive method of delivering radiation directly to the tumor. It is effective in controlling tumor growth while preserving surrounding structures. Fractionated CyberKnife radiotherapy has been shown to be effective and well-tolerated for pediatric oculomotor nerve schwannomas, achieving excellent tumor control with minimal side effects.
- Intensity-Modulated Radiation Therapy (IMRT): IMRT uses sophisticated software and 3D imaging to deliver high doses of radiation conforming to the tumor’s shape, minimizing exposure to healthy tissue. This approach is beneficial for tumors in complex anatomical locations.
- Image-Guided Radiation Therapy (IGRT): IGRT uses real-time imaging during radiation therapy to ensure precise targeting and minimal movement, enhancing the accuracy and effectiveness of the treatment.
Emerging Therapies
Recent advances in molecular biology and genetics have led to the development of targeted therapies for schwannomas, particularly for those associated with NF2.
- Bevacizumab: Bevacizumab, a VEGF inhibitor (a drug that stops the growth of new blood vessels), has shown efficacy in reducing tumor size and improving hearing in patients with NF2-related vestibular schwannomas. It is considered a first-line medical therapy for cases resistant to radiotherapy. Lower dosages of bevacizumab have been found to be effective while reducing the risk of side effects such as hypertension and menorrhagia.
- Protein Kinase Inhibitors: These drugs target signaling pathways involved in tumor growth and are being investigated for their potential to slow tumor progression.
- Immunotherapy: Novel approaches such as nanobody-decorated bacterial outer membrane vesicles are being explored for their potential to stimulate the immune system to target schwannoma cells.
- Non-Surgical Treatments: Research is ongoing to develop non-surgical treatments for schwannomas, including drugs that block pro-tumor signaling pathways. Early-phase clinical trials are being conducted to evaluate the efficacy of these new compounds.
More information about completed and ongoing clinical trials for pediatric schwannoma can be found here – clinicaltrials.gov.
Patient Experience
Survivorship care is crucial for pediatric patients with schwannomas, focusing on long-term monitoring and management of potential complications:
- Regular Follow-Up: Periodic MRI scans to monitor for tumor recurrence or growth.
- Hearing Rehabilitation: For patients with vestibular schwannomas, hearing aids or cochlear implants may be necessary to manage hearing loss.
- Physical Therapy: To address motor deficits and improve functional outcomes, particularly in cases of spinal or peripheral schwannomas.
- Psychosocial Support: Counseling and support groups to help patients and families cope with the emotional and psychological impact of the disease and its treatment.
Problems During and After Treatment and How to Manage Them
Surgical Complications
- Facial Nerve Damage: Can result in facial weakness or paralysis. Early intervention with physical therapy and, in some cases, surgical nerve repair can improve outcomes.
- Cerebrospinal Fluid Leaks: Managed with bed rest, head elevation, and sometimes surgical repair.
Radiation Therapy Complications
- Hearing Loss: Regular audiometric evaluations and use of hearing aids or cochlear implants as needed.
- Radiation-Induced Tumors: Long-term monitoring for secondary malignancies, particularly in young patients.
Neurological Deficits
- Motor and Sensory Deficits: Physical and occupational therapy to improve function and quality of life.
- Pain Management: Use of medications, nerve blocks, and multidisciplinary pain management approaches.
Recommendations for Patients and Their Caregivers
Medical Follow-Up
- Regular Check-Ups: It is crucial for patients to have regular follow-up appointments with their healthcare providers to monitor for any signs of recurrence and manage ongoing symptoms. This includes periodic imaging studies such as MRI or CT scans to ensure that the tumor has not returned.
- Specialist Consultations: Depending on the location and impact of the schwannoma, consultations with specialists such as neurologists, audiologists, or physical therapists may be necessary to address specific issues like nerve damage, hearing loss, or balance problems.
Managing Symptoms
- Physical Therapy: Engaging in physical therapy can help manage and improve balance or coordination issues resulting from nerve damage. This is particularly important for patients who have undergone surgery that affected their motor functions.
- Assistive Devices: For patients experiencing hearing loss, the use of hearing aids or other assistive devices can significantly improve their quality of life. Similarly, other adaptive equipment may be recommended based on individual needs.
Psychological Support
- Counseling: Psychological counseling is essential to help patients and their families cope with the emotional impact of the diagnosis and treatment. This can include individual therapy, family therapy, or support groups specifically for children and families dealing with schwannomas.
- Educational Support: Collaborating with schools to ensure that children receive the necessary accommodations can help them continue their education without significant disruption.
Lifestyle and Wellness
- Healthy Diet and Exercise: Encouraging a healthy diet and regular exercise can promote overall well-being and aid in recovery. Nutritional support and physical activity are important components of a comprehensive care plan.
- Stress Management: Teaching and practicing stress management techniques, such as mindfulness, relaxation exercises, and other coping strategies, can help patients and their families manage anxiety and stress related to the illness and its treatment.
Caregiver Support
- Education: Caregivers should educate themselves about schwannomas and their treatment to better understand what the patient is going through and how they can provide effective support. This includes learning about potential complications and the long-term management of the condition.
- Self-Care: It is important for caregivers to take care of their own physical and emotional health. Caregiving can be demanding, and seeking support from other family members, friends, or professional services can help prevent burnout. Support groups for caregivers can also provide valuable emotional support and practical advice.
By following these recommendations, patients and their caregivers can better navigate the challenges associated with these tumors, ensuring a higher quality of life and more effective management of the condition.
Prognosis
The prognosis for pediatric schwannomas is generally favorable, especially when complete surgical resection is achieved. The recurrence rate is low, and long-term outcomes are excellent, with most patients experiencing significant improvement in symptoms post-surgery. However, the prognosis can be more guarded in cases associated with NF2 due to the potential for multiple tumors and other complications. Factors influencing prognosis include:
- Tumor Size and Location: Larger tumors and those located in critical areas such as the brainstem or spinal cord can pose greater surgical challenges and have a higher risk of complications.
- Genetic Factors: The presence of NF2 significantly influences prognosis due to the likelihood of multiple schwannomas and other associated tumors.
- Extent of Surgical Resection: Complete resection is associated with better outcomes, while subtotal resection can lead to recurrence.
- Age at Diagnosis: Younger patients may have a better capacity for recovery, but early diagnosis is crucial for optimal outcomes.
Conclusion
Pediatric schwannomas, though rare, require a comprehensive and multidisciplinary approach to diagnosis, treatment, and long-term care. Advances in surgical techniques, radiation therapy, and emerging molecular therapies offer hope for improved outcomes. Ongoing research and clinical trials continue to expand our understanding and treatment options for these tumors. By staying informed and engaged in their care, patients and caregivers can navigate the challenges of these tumors and achieve the best possible outcomes.
In this video, Roderick shares his experience as a schwannoma patient. The video is produced by Johns Hopkins Medicine.
Resources
-
Challenging the Status Quo in Colorectal Cancer 2024
December 6-8, 2024
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023
