What is Pilocytic astrocytoma?
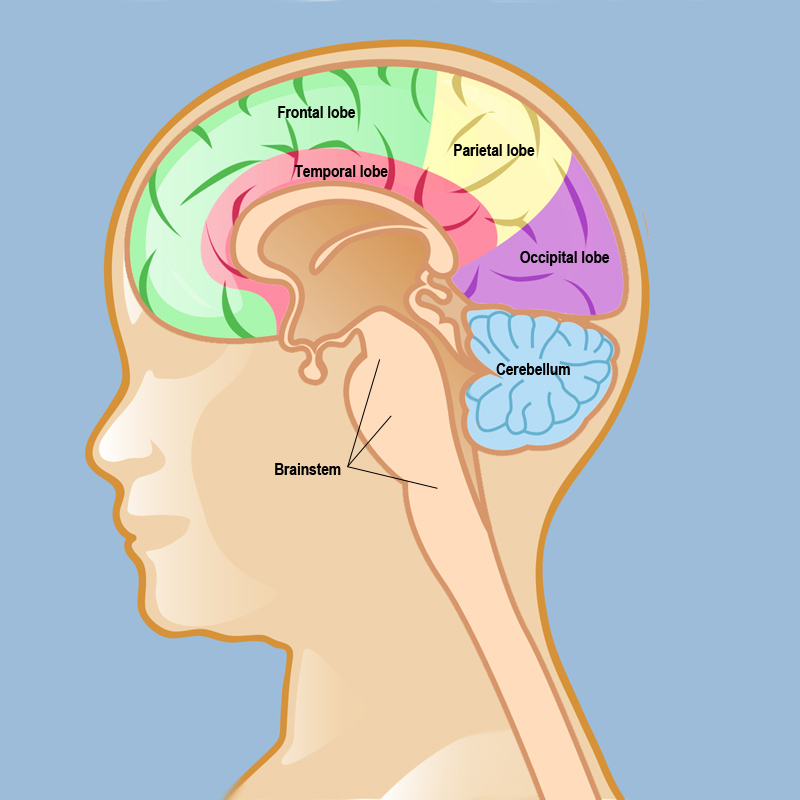
Pilocytic astrocytoma (PA) is a type of brain tumor that primarily affects children and young adults, typically occurring within the first two decades of life. It is classified as a World Health Organization (WHO) grade I tumor, indicating that it is generally benign and slow-growing. Pilocytic astrocytomas most commonly occur in the cerebellum and the optic pathway. These tumors are composed of astrocytes, which are star-shaped glial cells that support neurons in the brain.
Source of image neurosurgery.weillcornell.org
Causes and Risk Factors
Genetic Factors
Several genetic conditions are associated with an increased risk of developing pilocytic astrocytoma:
- Neurofibromatosis Type 1 (NF1): This genetic disorder is one of the most common conditions linked to PA. It is characterized by changes in skin pigmentation and the growth of tumors along nerves in the skin, brain, and other parts of the body.
- Neurofibromatosis Type 2 (NF2): Although less commonly associated with PA than NF1, NF2 can also increase the risk of developing these tumors.
- Li-Fraumeni Syndrome: This rare inherited disorder increases the risk of several types of cancer, including PA.
- Tuberous Sclerosis Complex: This genetic disorder causes non-malignant tumors to form in many different organs, including the brain, and is associated with an increased risk of PA.
- Nevoid Basal Cell Carcinoma Syndrome (Gorlin Syndrome): This condition increases the risk of various cancers, including PA.
- Turcot Syndrome: This rare genetic condition is associated with an increased risk of brain tumors, including PA, and colorectal cancer.
Environmental and Other Factors
In addition to genetic predispositions, certain environmental and immunologic factors may contribute to the development of pilocytic astrocytoma:
- Exposure to Ionizing Radiation: Previous exposure to radiation, such as radiation therapy for other medical conditions, can increase the risk of developing PA.
- Ultraviolet (UV) Rays: Some studies suggest that exposure to UV rays may play a role in the development of pilocytic astrocytoma, although this is less well-established.
- Contact with Certain Chemicals: Exposure to specific chemicals has been proposed as a potential risk factor, though more research is needed to confirm this link.
While the exact cause of pilocytic astrocytoma remains unclear, a combination of genetic predispositions and environmental exposures are believed to contribute to its development.
Symptoms
The symptoms of pilocytic astrocytoma (PA) can vary widely depending on the size and location of the tumor. Here are the common symptoms as reported by various sources:
General Symptoms
- Headaches: Often one of the first symptoms, headaches can be persistent and severe.
- Nausea and Vomiting: These symptoms are frequently associated with increased intracranial pressure due to the tumor.
- Vision Problems: These can include blurred vision, double vision, or other visual disturbances, especially if the tumor is near the optic pathways.
- Difficulty Walking or Balancing: Tumors in the cerebellum can affect coordination and balance.
- Seizures: Although not very common, seizures can occur.
- Fatigue: General tiredness and lack of energy can be a symptom.
Location-Specific Symptoms
- Cerebellum: Tumors here can cause problems with coordination, balance, and fine motor skills.
- Brainstem: Tumors in this area can lead to more severe symptoms, including difficulty swallowing, facial weakness, and other cranial nerve deficits.
- Optic Pathways: Tumors affecting the optic nerves or chiasm can lead to visual disturbances and even vision loss.
- Hypothalamic Region: Tumors in this area can cause hormonal imbalances, weight gain, and other endocrine-related symptoms.
Complications
- Hydrocephalus: This is a condition where fluid builds up in the brain, leading to increased intracranial pressure, which can be life-threatening if not treated.
- Brainstem Compression: Large tumors can press against the brainstem, causing severe neurological deficits.
Diagnosis
Diagnosing pilocytic astrocytoma (PA) involves a combination of clinical evaluation, imaging studies, and sometimes histopathological examination.
Clinical Evaluation
- Initial Assessment: The diagnostic process often begins with a thorough medical history and physical examination, focusing on neurological symptoms such as headaches, nausea, vomiting, vision problems, and coordination issues.
Imaging Studies
- Magnetic Resonance Imaging (MRI): MRI is the gold standard for diagnosing pilocytic astrocytoma. It provides detailed images of the brain and spinal cord, helping to identify the size, location, and characteristics of the tumor. PAs typically appear as well-circumscribed, cystic lesions with an enhancing mural nodule on MRI scans.
- Computed Tomography (CT) Scan: While less detailed than MRI, CT scans can be useful, especially in emergency settings. They can help detect calcifications and the extent of the tumor, particularly in cases where MRI is not available.
Histopathological Examination
- Biopsy: In some cases, a biopsy may be performed to confirm the diagnosis. This involves surgically removing a small sample of the tumor tissue for microscopic examination. The histopathological features of pilocytic astrocytoma include biphasic patterns with both compacted and loose, microcystic areas, and the presence of Rosenthal fibers and eosinophilic granular bodies.
Additional Diagnostic Tools
- Spectroscopy: MR spectroscopy can provide metabolic information about the tumor, which can help differentiate pilocytic astrocytoma from other types of brain tumors.
- Functional MRI (fMRI): This imaging technique can be used to assess the functional areas of the brain and plan surgical approaches to minimize damage to critical brain regions
Treatment
The primary treatment for pilocytic astrocytoma (PA) is surgical resection, with the goal of completely removing the tumor if possible. The extent of surgical resection depends on the tumor’s location and proximity to critical brain structures. Additional treatments may be recommended based on the extent of resection, tumor location, and other factors.
Surgery
- Complete Resection: If the tumor is located in accessible areas like the cerebellum or cerebral hemispheres, complete surgical removal is often achievable and can be curative.
- Partial Resection: In cases where the tumor is located near critical brain regions (e.g., brainstem, optic pathways), complete removal may not be feasible due to the risk of neurological deficits. In such cases, partial resection (debulking) is performed to remove as much of the tumor as safely as possible.
Adjuvant Therapy
Adjuvant therapy may be recommended after surgery, depending on the extent of resection and other factors:
- Radiation Therapy: Radiation therapy may be used as an adjuvant treatment after partial resection or in cases where the tumor cannot be surgically removed. However, radiation is generally avoided in young children (under 3-5 years old) due to the potential for long-term neurocognitive side effects.
- Chemotherapy: Chemotherapy is sometimes used as an adjuvant treatment, particularly in cases where radiation therapy is not recommended or when the tumor is unresectable. Common chemotherapy agents used include carboplatin, vincristine, and temozolomide.
Emerging Targeted Therapies
Recent advances in molecular profiling have led to the identification of targetable genetic alterations in pilocytic astrocytoma, paving the way for targeted therapies:
- BRAF* Inhibitors: Have shown promising results in clinical trials.
- MEK* Inhibitors: Drugs targeting the MEK pathway have also demonstrated efficacy in clinical trials for PAs with BRAF or NF1 alterations.
- Combination Therapies: Ongoing research is exploring the potential of combining targeted therapies with chemotherapy or other agents to enhance efficacy and overcome resistance mechanisms.
*These are genes, activation of which may lead to uncontrolled cellular division and cancerogenesis.
Follow-up and Monitoring
Patients with pilocytic astrocytoma require regular follow-up with imaging studies (MRI) to monitor for tumor recurrence or progression. Additional surgery, radiation therapy, or targeted therapies may be considered if the tumor recurs or progresses.
In summary, the treatment approach for pilocytic astrocytoma involves maximizing safe surgical resection, followed by adjuvant therapy (radiation or chemotherapy) as needed. Recent advances in molecular profiling have led to the development of targeted therapies, offering promising new treatment options for patients with specific genetic alterations.
Prognosis and Survivorship
Pilocytic astrocytoma (PA) is a generally benign and slow-growing brain tumor that primarily affects children and young adults, and it has an excellent prognosis, especially when detected early and completely removed through surgery. Most patients can expect a good quality of life after treatment, with high long-term survival rates. Regular follow-up with imaging is important to monitor for any signs of recurrence. While the prognosis is very favorable for younger patients, it can be less so for older adults, who may experience more aggressive tumor behavior. Overall, with appropriate treatment and monitoring, the outlook for individuals with PA is very positive.
Watch Juvenile’s Cancer Survival Story from Culicchia Neurology
Survivorship Challenges
Survivorship for patients with pilocytic astrocytoma (PA) involves managing a range of long-term physical, cognitive, and psychosocial challenges. While the prognosis for PA is generally excellent, especially in children and young adults, survivors often face various complications that can impact their quality of life.
Physical and Neurological Complications
- Neurological Issues: Survivors may experience seizures, headaches, dysarthria (difficulty speaking), ataxia (lack of muscle coordination), paralysis, fine motor skill deficits, dizziness, and facial palsy.
- Endocrine Problems: These can include precocious puberty, growth hormone deficiency, panhypopituitarism (deficiency of all pituitary hormones), and obesity.
- Cognitive Impairments: Long-term cognitive issues such as difficulties with attention, processing speed, memory, and executive function are common, particularly in those treated for cerebellar pilocytic astrocytoma. These cognitive deficits can affect academic performance and daily functioning.
Psychosocial and Behavioral Challenges
- Psychiatric Complications: Survivors may face psychiatric issues such as alcohol dependence, nervous personality, isolation, major depressive disorder, self-harm, suicide, somatizing syndrome, attention deficit hyperactivity disorder (ADHD), hallucinations, bulimia nervosa, inappropriate behavior, and violent behavior.
- Social and Academic Difficulties: Pediatric brain tumor survivors often experience challenges in social integration, academic performance, and employment. These difficulties can persist into adulthood, affecting their ability to transition smoothly into adult roles and responsibilities.
Quality of Life and Long-term Health
- Health-Related Quality of Life (HRQoL): While many survivors report satisfactory HRQoL, specific areas such as vitality and physical well-being may be impacted. Survivors may also face increased fatigue, reduced strength, and poor cardiorespiratory fitness, which can affect their overall quality of life.
- Late Effects of Treatment: Long-term complications from treatments, such as surgery, radiation, and chemotherapy, can include secondary chronic health conditions like cardiovascular disease, metabolic disorders, and secondary malignancies.
Support and Interventions
- Follow-up Care: Regular follow-up with healthcare providers is crucial for monitoring and managing long-term complications. This includes ongoing MRI scans, neurological assessments, and social support services.
- Therapeutic Interventions: Therapeutic exercise programs have shown promise in improving physical outcomes and quality of life for pediatric brain tumor survivors. These programs can help address issues like reduced strength and increased fatigue.
- Psychological Support: Early recognition and intervention for psychological symptoms are essential. Counseling and support services can help survivors manage psychiatric complications and improve social and academic integration.
In summary, while the prognosis for pilocytic astrocytoma is generally favorable, survivors often face a range of long-term challenges that require comprehensive and ongoing management. Regular follow-up care, therapeutic interventions, and psychological support are critical components of survivorship care to help improve the quality of life for these patients.
During Treatment
Common Side Effects and Management Strategies
Surgery
- Pain, swelling, and bleeding at the surgical site can occur after tumor removal surgery. Pain medication and applying ice packs can help manage these.
- Temporary neurological deficits like weakness, numbness, and speech problems may happen depending on the tumor location. These usually improve with time but physical/speech therapy may be needed.
- Seizures can sometimes occur after surgery. Anti-seizure medications may be prescribed to control them.
- A cerebrospinal fluid leak is a potential complication that may require additional surgery to repair.
Radiation Therapy
- Fatigue is a very common side effect that can be managed with adequate rest and nutrition.
- Skin irritation in the area being treated. Using fragrance-free moisturizers can help.
- Hair loss can occur in the area of radiation but is usually temporary.
- Nausea and vomiting may happen and can be controlled with anti-nausea medications.
- Long-term effects in children like cognitive deficits, and growth hormone deficiency require monitoring and supportive care.
Chemotherapy
- Nausea, vomiting, and diarrhea are common and can be managed with medications and dietary changes.
- Low blood counts increasing infection/bleeding risk may require medication or transfusions.
- Fatigue is very common and may need rest periods.
- Hair loss is also frequent but temporary.
General Strategies
- Anti-seizure medications for seizure control
- Steroids like dexamethasone to reduce brain swelling/edema
- Physical/occupational/speech therapy for functional deficits
- Psychosocial support for anxiety, depression, cognitive issues
Careful monitoring and proactive management of side effects is important, especially in pediatric patients, to optimize quality of life during and after pilocytic astrocytoma treatment.
After Treatment
Follow-up Care
After treatment for pilocytic astrocytoma, regular follow-up care is essential to ensure the best possible outcome and manage any long-term effects. This includes frequent check-ups with your healthcare team, typically every 1-3 months initially, then less often over time. Patients usually have regular MRI scans to monitor for any signs of the tumor returning, especially in the first few years. It’s also important to have neuropsychological assessments to check on cognitive functions like memory and attention, as well as endocrine evaluations to monitor hormone levels. Physical, occupational, and speech therapy may be recommended to help with any lingering neurological issues.
Resources
- American Cancer Society – Cancer.org
- National Cancer Institute – Cancer.gov
- American Society of Clinical Oncology (ASCO) – Cancer.net
- Cancer Research Institute – cancerresearch.org
- Survival and Prognosis of Patients with Pilocytic Astrocytoma: A Single-Center Study – PubMed
- Pilocytic astrocytoma survival in adults: analysis of the Surveillance, Epidemiology, and End Results Program of the National Cancer Institute – PubMed
- Cerebellar pilocytic astrocytoma in childhood: Investigating the long-term impact of surgery on cognitive performance and functional outcome – PubMed
- Postoperative surveillance of pediatric cerebellar pilocytic astrocytoma – PubMed
- Wikipedia – en.wikipedia.org
- Stanford Medicine – Stanfordhealthcare.org
- University of California San Francisco – Braintumorcenter.ucsf.edu
- Oncodaily.com
