Medulloblastoma: What patients should know about
What is Medulloblastoma?
Medulloblastoma is a malignant (cancerous) brain tumor that originates in the cerebellum, which is located at the base of the brain near the brainstem. It is the most common type of cancerous brain tumor in children, though it can also occur in adults, typically between the ages of 20 and 44.
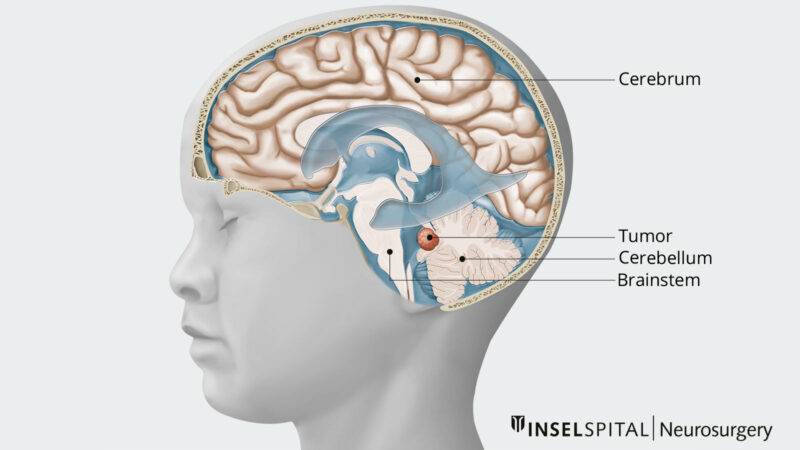
Source of image neurochirurgie.insel.ch
Causes and Risk Factors
The exact cause of medulloblastoma is not well understood, but several genetic and environmental factors have been identified as potential risk factors.
Genetic Mutations and Syndromes:
- BRCA1 and BRCA2 Mutations: These genes, typically associated with breast cancer, can also play a role in the development of medulloblastoma by failing to repair damaged DNA properly.
- Gorlin Syndrome: Also known as nevoid basal cell carcinoma syndrome, this genetic condition increases the risk of developing medulloblastoma.
- Turcot Syndrome: A subtype of Lynch syndrome, this condition is associated with a higher risk of medulloblastoma.
- Li-Fraumeni Syndrome: This genetic disorder, which increases the risk of various cancers, is also linked to medulloblastoma.
Chromosomal Abnormalities:
- Nearly half of childhood medulloblastomas have a genetic abnormality on chromosome 17. Other chromosomal abnormalities have been identified on chromosomes 1, 7, 8, 9, 10q, 11, and 16.
Age and Gender:
- Medulloblastoma is most common in children, particularly those under the age of 16, with the highest incidence between ages 5 and 9. It is more prevalent in boys than girls.
Environmental Factors:
- While radiation exposure is a known risk factor, there are currently no other established environmental or lifestyle-related risk factors for medulloblastoma in children.
Symptoms
Medulloblastoma symptoms can vary depending on the tumor’s size, location, and the pressure it causes in the brain. Here are the common symptoms as detailed in the provided sources:
General Symptoms
- Headaches: Often worse in the morning.
- Nausea and Vomiting: Frequently associated with headaches and can provide temporary relief.
- Dizziness
- Double Vision
- Poor Coordination and Balance: Issues with walking, balance, and fine motor skills.
- Unsteady Walk
- Tiredness and Lethargy
- Seizures: In some cases, seizures may occur.
- Behavioral Changes: Increased irritability, changes in interaction with family members, and loss of appetite.
Symptoms Related to Hydrocephalus (Fluid Buildup in the Brain)
- Blurred Vision
- Extreme Sleepiness
- Confusion
- Seizures and Passing Out
- Increasing Head Size: An increasing head circumference can be a sign in infants
- Bulging Fontanelle: Swollen Soft Spot on the Skull (Fontanelle) in infants
Symptoms of the Tumor spread to the Spine
- Weakness or Numbness in the Arms and/or Legs
- Changes in Bowel or Bladder Habits
- Back pain
Symptoms of the Tumor spread to Other Organs
- Coughing, Chest Pain, and Shortness of Breath
- Enlarged Lymph Nodes
- Bone Pain
Diagnosis
Diagnosing medulloblastoma involves a combination of clinical evaluations, imaging studies, and laboratory tests. Here are the key steps and methods used in the diagnosis:
Neurological Exam
- A neurological exam is often the first step in diagnosing medulloblastoma. This exam tests vision, hearing, balance, coordination, and reflexes to help identify which part of the brain might be affected by the tumor.
Imaging Tests
Imaging tests are crucial for visualizing the tumor and assessing its size, location, and potential spread. The primary imaging modalities include:
- Magnetic Resonance Imaging (MRI): MRI is the preferred imaging technique as it provides detailed images of the brain and spinal cord. It can show the tumor’s size, location, and whether it has caused hydrocephalus (fluid buildup in the brain).
- Computed Tomography (CT) Scan: CT scans can also be used to visualize the tumor, though they are less detailed than MRIs. They are often used in emergency settings or when MRI is not available.
Tissue Sample Testing (Biopsy)
In some cases, a biopsy may be performed to confirm the diagnosis. This involves removing a small sample of the tumor tissue for examination under a microscope. However, biopsies for medulloblastoma are uncommon and typically done only in specific situations.
Lumbar Puncture (Spinal Tap)
A lumbar puncture involves inserting a needle between two bones in the lower spine to draw cerebrospinal fluid (CSF). The CSF is then tested for the presence of tumor cells. This test is usually performed after managing any increased pressure in the brain or after tumor removal.
Additional Tests
- Spinal MRI: To check for the spread of the tumor to the spinal cord.
- Audiometry: Hearing tests may be conducted before starting treatments like cisplatin, which can affect hearing.
- Echocardiogram and Pulmonary Function Tests: These are baseline tests performed before starting chemotherapy to assess heart and lung function.
The diagnosis of medulloblastoma is a multi-step process that includes a thorough neurological exam, advanced imaging techniques like MRI and CT scans, and laboratory tests such as lumbar puncture and, in some cases, biopsy. These methods help determine the tumor’s characteristics, its spread, and the best course of treatment.
Treatment
The treatment for medulloblastoma typically involves a multimodal approach combining surgery, radiation therapy, and chemotherapy. The specific treatment plan is tailored based on factors such as the patient’s age, the extent of the tumor, and the molecular subgroup of the medulloblastoma.
Surgery
The first step in treatment is usually surgical resection, which aims to remove as much of the tumor as possible without causing further neurological damage. Complete surgical removal is often difficult due to the location of the tumor in the posterior fossa and its tendency to spread through the cerebrospinal fluid.
Radiation Therapy
After surgery, radiation therapy is a crucial component of treatment for most patients. The standard approach is craniospinal radiation therapy (CSI), which involves irradiating the entire brain and spinal cord. This is because medulloblastoma cells can spread through the cerebrospinal fluid.
Chemotherapy
Chemotherapy is an essential component of treatment, used in combination with surgery and radiation therapy.
The specific chemotherapy regimen may vary based on the patient’s risk stratification and molecular subgroup of medulloblastoma.
Prognosis and Survivorship
Survival rates vary based on factors like the child’s age, how much of the tumor can be removed through surgery, whether it has spread, and the specific molecular subtype of the tumor. Some subtypes have very high survival rates over 90%, while others are more aggressive and have lower survival chances. With advances in treatment like targeted therapies and improved radiation and chemotherapy, the prognosis for medulloblastoma continues to improve. Still, many survivors face long-term side effects from the intensive treatments required, so close follow-up care is essential. The path forward is challenging but hopeful for most children with this condition.
Watch Jules’s Survival Story from Dayton Children’s Hospital
Survivorship Challenges
Survivorship for medulloblastoma patients involves navigating a range of long-term challenges that can significantly impact quality of life. These challenges stem from the aggressive treatments required to manage the disease, including surgery, radiation, and chemotherapy, which can lead to various physical, cognitive, and psychosocial issues.
Long-Term Physical Effects
- Endocrine Dysfunction: A high prevalence of endocrine issues, such as growth hormone deficiency and hypothyroidism, is common among survivors due to the impact of craniospinal irradiation and chemotherapy on the hypothalamic-pituitary axis.
- Hearing Loss: Many survivors experience hearing impairments, which can affect communication and social interactions.
- Secondary Cancers: There is an increased risk of secondary malignancies due to the mutagenic effects of radiation and chemotherapy.
- Cardiovascular and Cerebrovascular Issues: Survivors have a higher risk of stroke and cardiovascular diseases, necessitating ongoing monitoring and preventive care.
Neurocognitive and Functional Challenges
- Cognitive Impairments: Survivors often face significant neurocognitive deficits, including problems with processing speed, attention, working memory, and executive functions. These impairments can worsen over time and are more pronounced in those diagnosed at a younger age.
- Educational and Employment Difficulties: Cognitive challenges contribute to lower academic achievement, higher rates of unemployment, and difficulties in living independently.
- Early Aging: Adult survivors may exhibit signs of early aging, such as the continued decline in working memory and other cognitive functions, regardless of the age at diagnosis.
Psychosocial Issues
- Social Isolation: Many survivors experience social isolation, difficulties in forming relationships, and lower rates of marriage and parenthood.
- Mental Health: Anxiety, depression, and other mental health issues are common, often exacerbated by the physical and cognitive challenges faced by survivors.
Management Strategies
Rehabilitation Services:
- Physical and Occupational Therapy: These therapies help address motor deficits, improve coordination, and enhance daily functioning. They are particularly important for patients who experience ataxia or other motor impairments.
- Speech Therapy: For patients with speech and swallowing difficulties, speech therapy can be beneficial.
Educational Support:
- Individualized Education Plans (IEPs): Tailored educational plans and classroom accommodations help address cognitive and learning challenges. Schools may provide special education services based on the results of neuropsychological assessments.
Psychosocial Support:
- Counseling and Support Groups: Emotional and social support through counseling, support groups, and social workers can help patients and families cope with the psychological impact of the disease and its treatment.
- Mental Health Services: Access to mental health professionals for managing anxiety, depression, and other psychological issues.
Medical Interventions:
- Hormone Replacement Therapy: For managing endocrine disorders like hypothyroidism and growth hormone deficiency, hormone replacement therapies are often necessary.
- Medications for Late Effects: Medications may be prescribed to manage other late effects, such as anticonvulsants for seizures or medications for managing secondary cancers.
Follow-up Care
Regular Monitoring and Assessments
Physical Exams and Imaging:
- Regular MRI Scans: Patients typically undergo MRI scans every 3 to 4 months for the first few years after treatment to monitor for tumor recurrence. The frequency of these scans may decrease over time if no recurrence is detected.
- Physical Exams: Regular physical exams are essential to assess the patient’s overall health and detect any signs of recurrence or new health issues.
Endocrine Function Tests:
- Hormone Level Monitoring: Given the risk of endocrine dysfunction due to radiation therapy, regular blood tests to monitor hormone levels (e.g., thyroid, growth hormone) are necessary. Endocrinologists often manage these aspects of care.
Neurocognitive Assessments:
- Cognitive Testing: Periodic neuropsychological evaluations help assess cognitive function and identify any learning or memory issues. These assessments guide interventions to support educational and cognitive development.
Hearing and Vision Tests:
- Audiometry: Regular hearing tests are important, especially for patients who received ototoxic chemotherapy agents like cisplatin.
- Vision Tests: Routine eye exams to monitor for any vision changes or issues related to treatment.
Lifestyle and Health Maintenance
Healthy Lifestyle Choices:
- Nutrition and Exercise: Encouraging a balanced diet and regular physical activity to support overall health and well-being.
- Avoiding Smoking and Alcohol: Advising against smoking and excessive alcohol consumption to reduce the risk of secondary cancers and other health issues.
Regular Health Screenings:
- Routine Health Check-Ups: Regular visits to primary care physicians for general health maintenance and early detection of any new health issues.
Vaccinations:
- Immunizations: Ensuring that patients are up-to-date with vaccinations, especially if they have been immunocompromised due to treatment.
Resources
- American Cancer Society – Cancer.org
- National Cancer Institute – Cancer.gov
- American Society of Clinical Oncology (ASCO) – Cancer.net
- Cancer Research Institute – cancerresearch.org
- Childhood Medulloblastoma: An Overview – PubMed
- Risk factors for the prognosis of pediatric medulloblastoma: a retrospective analysis of 40 cases – PubMed
- Current Strategies for Management of Medulloblastoma – PubMed
- ScienceDirect – Sciencedirect.com
- Johns Hopkins Medicine – Hopkinsmedicine.org
- Oncodaily.com
-
Challenging the Status Quo in Colorectal Cancer 2024
December 6-8, 2024
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023
