Renal Cell Carcinoma in Children: What patients and caregivers should know about
What is Renal Cell Carcinoma?
Renal cell carcinoma (RCC) is a rare type of kidney cancer that primarily affects children and young adults. While RCC is the most common type of kidney cancer in adults, it accounts for only 3.5% of all pediatric renal neoplasms. However, the incidence of renal cell carcinoma (RCC) in children and adolescents has been steadily rising over the past several years. There are a few key factors that contribute to this increase:
- Improved diagnostic techniques: Advances in imaging technologies, such as CT scans and MRI, have allowed for earlier and more accurate detection of RCC in younger patients.
- Increased awareness and surveillance: There is greater awareness among healthcare providers about the potential for RCC to occur in children and adolescents, leading to more vigilant screening and diagnosis.
- Underlying genetic conditions: Certain genetic syndromes, such as von Hippel-Lindau disease, are known to predispose children and adolescents to developing RCC. As genetic testing has become more widespread, more cases of RCC associated with these conditions are being identified.
- Environmental and lifestyle factors: Some studies suggest that exposure to certain environmental toxins or changes in lifestyle factors (e.g., obesity) may be contributing to the rise in pediatric and adolescent RCC cases, though the evidence is still limited.
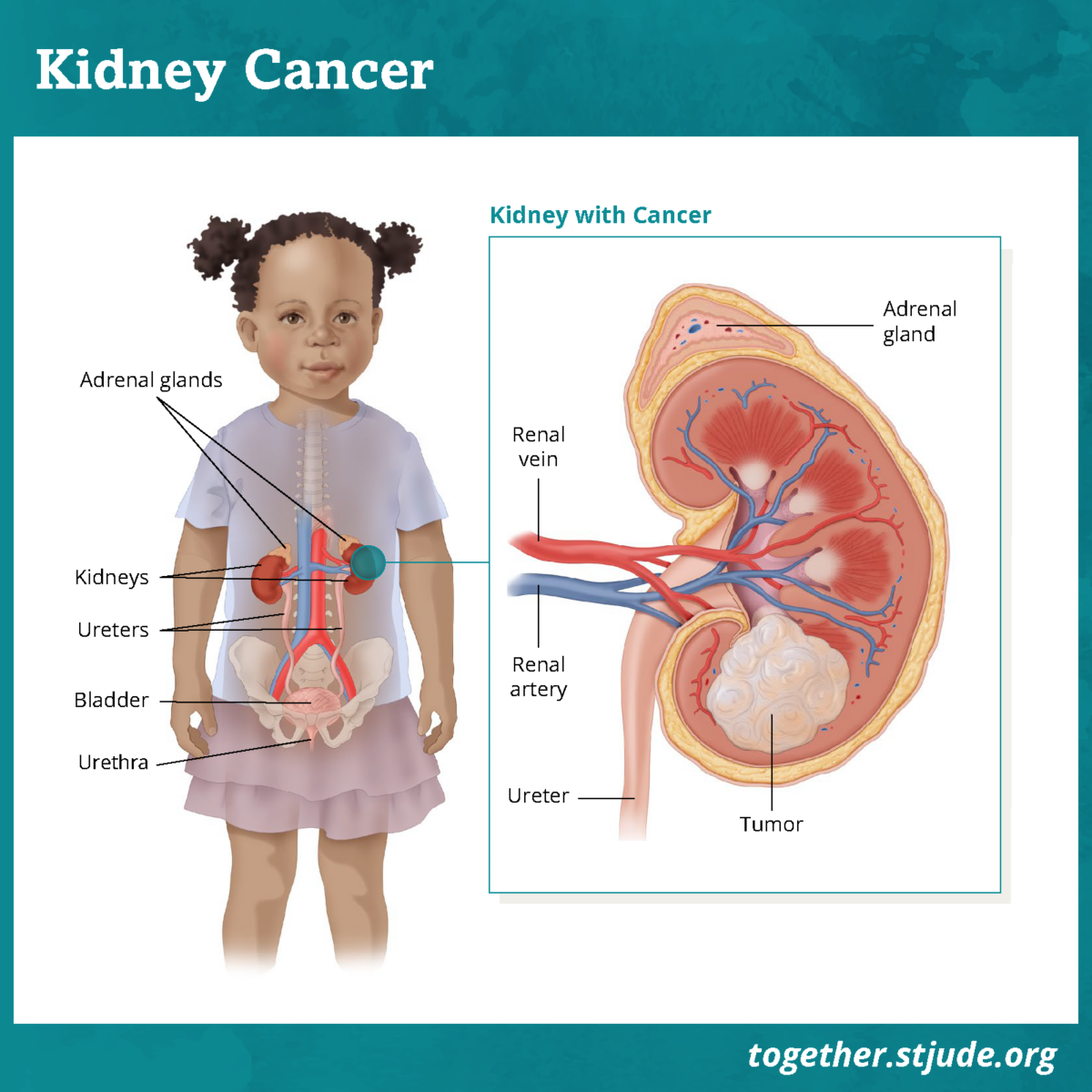
This image is taken from together.stjude.org.
Causes and Risk Factors
The exact causes of RCC in children are not fully understood, but several risk factors have been identified:
- Genetic predisposition: Certain genetic syndromes, such as von Hippel-Lindau (VHL) disease, tuberous sclerosis, and Birt-Hogg-Dubé syndrome, are associated with an increased risk of RCC.
- Environmental factors: Exposure to certain chemicals, such as trichloroethylene, has been linked to an increased risk of RCC in adults, but the evidence in children is limited.
- Radiation exposure: Children who have undergone radiation therapy, particularly for other cancers, may have a higher risk of developing RCC.
You can find information about kidney cancer in this video prepared by the National Kidney Foundation.
Symptoms
The presenting symptoms of RCC in children can be highly variable and non-specific, which often leads to delayed diagnosis. The most common symptoms include:
- Abdominal or flank pain
- Hematuria (blood in urine)
- Palpable abdominal mass
- Weight loss
- Fever
Some children may be asymptomatic, with the tumor discovered incidentally during imaging for other medical conditions. In rare cases, paraneoplastic syndromes such as hypertension, polycythemia, or hypercalcemia may be the initial presentation.
Diagnosis
Early and accurate diagnosis of RCC in children is crucial for effective treatment and management. The diagnostic workup typically includes
- Imaging studies: Magnetic resonance imaging (MRI) is the preferred imaging modality for evaluating pediatric RCC, as it provides detailed information about the tumor’s size, location, and extent without the use of ionizing radiation. Computed tomography (CT) scans may also be used, but they carry a higher risk of radiation exposure.
- Biopsy: In some cases, a biopsy may be performed to confirm the diagnosis and determine the tumor’s histological subtype.
- Genetic testing: Genetic testing may be recommended, especially in cases with a family history or suspicion of an underlying genetic syndrome.
The National Kidney Foundation has a helpful video that provides valuable insights into the diagnosis of kidney cancer.
Treatment and Prognosis
The treatment of pediatric RCC depends on the stage of the disease, the histological subtype, and the patient’s overall health and age. The main treatment modalities include:
Surgery
- The primary treatment for localized RCC in children is surgical resection, either partial or radical nephrectomy.
- Surgical removal of the affected kidney, with or without lymph node dissection, is the mainstay of treatment for localized disease.
- Studies have shown excellent survival rates for children who undergo successful surgical resection
- Partial nephrectomy, which preserves healthy kidney tissue, has also been associated with higher survival rates in children.
Systemic Therapy
- For advanced or metastatic RCC, systemic therapies such as targeted therapies and immunotherapies are being investigated.
- Newer targeted therapies, including tyrosine kinase inhibitors and mTOR inhibitors, have shown promising results in the treatment of advanced or metastatic RCC in children.
- Immunotherapy agents, such as checkpoint inhibitors, are also being explored for the treatment of pediatric RCC.
- However, the search results indicate that the survival rates for children with advanced or metastatic RCC remain poor
Radiation Therapy
- Radiation therapy may be used in certain cases, such as for the treatment of metastatic disease or as palliative care for symptomatic patients.
- The role of radiation therapy in the management of pediatric RCC is limited, as the search results do not provide detailed information on its efficacy.
This short video explains three types of immunotherapy used to treat cancer: nonspecific immune stimulation, T-cell transfer therapy, and immune checkpoint inhibitors.
Patient’s Survivorship
For children who undergo successful treatment for RCC, the long-term prognosis and quality of life can be quite good, especially for those with localized, low-stage disease. However, children treated for RCC may face several long-term challenges and potential complications, including:
- Chronic kidney disease and the need for lifelong monitoring and management of kidney function
- Increased risk of developing other types of cancer, particularly in those with genetic predispositions
- Psychosocial and emotional challenges, such as anxiety, depression, and body image issues
- Fertility and reproductive concerns, especially in those who have undergone extensive treatment or radiation therapy
Comprehensive long-term follow-up care, including regular check-ups, monitoring of kidney function, and access to supportive services, is essential for ensuring the best possible outcomes for children who have survived RCC.
Recommendations for Patients
- Early Detection and Diagnosis
- Be aware of the common symptoms of RCC in children, including abdominal/flank pain, hematuria, palpable abdominal mass, weight loss, and fever.
- Seek prompt medical attention if any of these symptoms are present, as early detection is crucial for improving outcomes.
- Undergo appropriate imaging tests, such as MRI or CT scans, to confirm the diagnosis and determine the stage of the disease.
- Consider genetic testing if there is a family history or suspicion of an underlying genetic syndrome.
- Treatment and Management
- Work closely with a multidisciplinary team of pediatric oncologists, urologists, and other specialists experienced in the treatment of RCC.
- Understand that the primary treatment for localized RCC is surgical resection, either partial or radical nephrectomy.
- Be aware that for advanced or metastatic disease, targeted therapies, immunotherapy, and other systemic treatments may be used in addition to or instead of surgery.
- Discuss the potential benefits and risks of each treatment option with the healthcare team to make an informed decision.
- Survivorship and Long-Term Care
- Recognize that the prognosis for children with low-stage RCC is generally good
- Understand that children with advanced or metastatic disease at diagnosis have a poorer prognosis
- Be prepared to manage potential long-term effects of treatment, such as chronic kidney disease, increased cancer risk, and psychosocial challenges.
- Participate in regular follow-up care, including monitoring of kidney function and screening for recurrence or secondary cancers.
- Seek support from healthcare providers, patient advocacy groups, and mental health professionals to address any physical, emotional, or social needs during and after treatment.
Conclusion
While the rise in pediatric RCC cases is concerning, there is reason for hope. Remarkable strides have been made in the early detection and treatment of this rare cancer in young patients.
Advances in diagnostic imaging, like CT scans and MRI, now allow doctors to identify RCC at earlier, more treatable stages. As genetic testing becomes more widespread, we are better able to detect underlying conditions that predispose children to developing RCC, enabling proactive monitoring and care.
As importantly, pediatric RCC patients’ treatment options have expanded significantly. Innovative surgical techniques, targeted therapies, and immunotherapies are giving young people with this disease a fighting chance. With a dedicated, multidisciplinary care team, many children can achieve long-term remission and go on to live full, vibrant lives.
While challenges remain, the future for children with RCC is brighter than ever before. By staying vigilant, leveraging the latest medical breakthroughs, and maintaining a spirit of hope, these young patients and their families can look ahead with optimism. With continued progress in research and care, the prognosis for pediatric RCC will only continue to improve.
Resources
- National Cancer Institute – cancer.gov
- American Cancer Society – cancer.org
- American Society of Clinical Oncology (ASCO) – Cancer.net
- Memorial Sloan Kettering Cancer Center – mskcc.org
- Clinicaltrials.gov
- National Kidney Foundation – Kidney.org
- Oncodaily.com
- Children’s Hospital of Philadelphia – Chop.edu
- Factors impacting survival in children with renal cell carcinoma – Pubmed
- Canadian Cancer Society – Cancer.ca
- The Diagnosis, Treatment, and Follow-up of Renal Cell Carcinoma – PubMed
- Renal cell carcinoma in children and adolescents – PubMed
- Characteristics and Outcome of Children with Renal Cell Carcinoma: A Narrative Review – PubMed
-
Challenging the Status Quo in Colorectal Cancer 2024
December 6-8, 2024
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023