Adjuvant Therapy in Cancer: Benefits, Types, Timing, and Precision-Based Innovations
Adjuvant therapy has become a cornerstone of modern oncologic care, representing a proactive approach to reducing cancer recurrence and improving long-term outcomes. Defined as treatment administered after the primary modality—most often surgery—adjuvant therapy aims to eliminate microscopic residual disease that may not be clinically detectable but poses a risk for future metastasis. Unlike neoadjuvant therapy, which is given before the main treatment to shrink tumors or enable resection, or palliative therapy, which focuses on symptom relief in advanced disease, adjuvant therapy is typically curative in intent.
The concept of adjuvant therapy has evolved from empirical practice to a rigorously evidence-based standard, with randomized clinical trials confirming its ability to increase disease-free survival (DFS) and overall survival (OS) across numerous malignancies. This article explores the scientific rationale, types, patient selection strategies, and emerging innovations in adjuvant therapy—highlighting its critical role in contemporary cancer management.
Biological Rationale and Clinical Justification for Adjuvant Therapy
Despite successful surgical resection of the primary tumor, many patients remain at risk for disease recurrence due to the presence of minimal residual disease (MRD)—microscopic clusters of malignant cells that may have disseminated before or during surgery. These undetectable remnants, including micrometastases lodged in regional lymphatics or distant organs, can eventually seed relapse if left untreated.
Adjuvant therapy is designed to eliminate these residual malignant cells through a range of mechanisms. Cytotoxic chemotherapy targets rapidly dividing cells, while antiangiogenic agents disrupt tumor vascularization, starving residual cancer cells of oxygen and nutrients. In recent years, immune checkpoint inhibitors have emerged as effective adjuvant options by enhancing the immune system’s ability to recognize and destroy remaining tumor cells. Additionally, endocrine therapies and targeted agents offer tumor-specific mechanisms that block proliferative signals in hormonally driven or genetically defined cancers.
Importantly, not all patients require or benefit equally from adjuvant therapy. Careful risk stratification—based on pathological features such as lymph node involvement, tumor grade, size, surgical margins, and increasingly, molecular signatures—guides the decision to offer adjuvant treatment. This personalized approach ensures that therapy is reserved for those at highest risk of relapse, optimizing benefit while minimizing unnecessary toxicity.
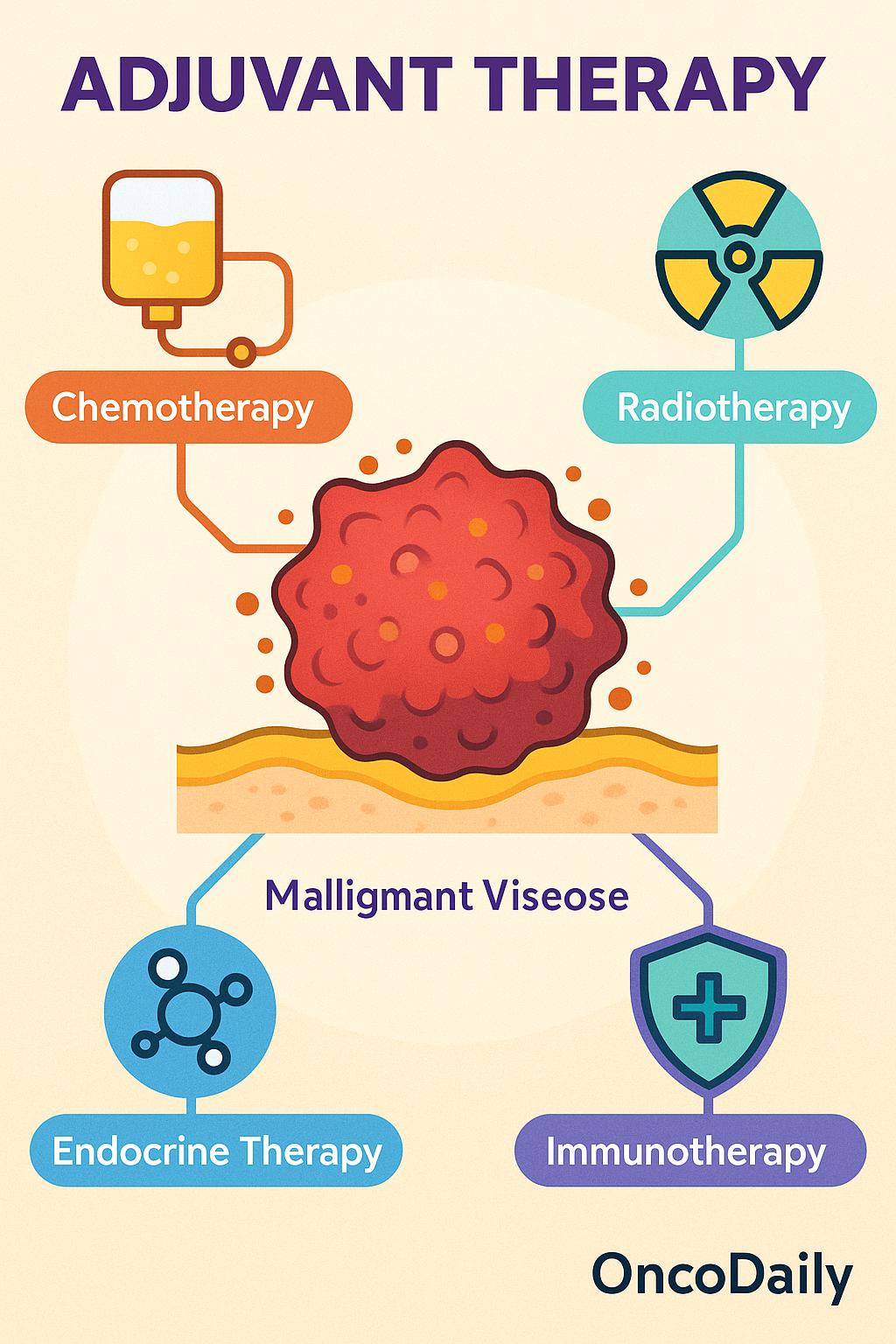
Types of Adjuvant Therapies
Adjuvant therapy is not a singular approach but a modality-specific strategy tailored to the tumor’s biology, staging, and risk profile. Depending on the cancer type and patient characteristics, adjuvant treatment may include chemotherapy, radiotherapy, endocrine therapy, targeted agents, or immunotherapy—each designed to attack residual disease through distinct mechanisms.
Adjuvant Chemotherapy
Adjuvant chemotherapy exerts systemic cytotoxic effects, targeting proliferating cancer cells that may have escaped resection. By interfering with DNA replication or mitosis, these agents help eliminate micrometastases and reduce the risk of recurrence. Common regimens include FOLFOX (5-fluorouracil, leucovorin, oxaliplatin) in stage III colorectal cancer, and anthracycline-taxane combinations in high-risk breast cancer. Landmark trials such as NSABP B-20 and MOSAIChave demonstrated significant improvements in both disease-free and overall survival, cementing chemotherapy’s role as a foundational component of adjuvant care in select malignancies.
Adjuvant Radiotherapy
Unlike chemotherapy, adjuvant radiotherapy provides localized control, typically delivered to the tumor bed or regional lymphatics to eliminate residual cancer cells in high-risk zones. It is especially critical when surgical margins are close or positive, or when anatomical constraints limit complete resection. Radiotherapy is standard in early-stage breast cancer following breast-conserving surgery, and in head and neck or central nervous system tumors where recurrence patterns are often locoregional. The timing, radiation dose, and treatment field are determined based on surgical pathology and risk stratification.
Adjuvant Endocrine Therapy
Endocrine therapy is specific to hormone receptor–positive tumors, primarily breast and prostate cancers. These therapies disrupt the hormonal environment that fuels tumor proliferation through estrogen receptor blockade, aromatase inhibition, or ovarian suppression.
In estrogen receptor–positive breast cancer, agents like tamoxifen or aromatase inhibitors are administered for 5–10 years post-surgery to significantly reduce recurrence and mortality. The choice and duration of therapy are guided by menopausal status, recurrence risk, and tolerability.
Adjuvant Targeted Therapy
Targeted therapies act on specific molecular alterations within cancer cells, offering precision treatment with typically less off-target toxicity. Their use in the adjuvant setting is expanding rapidly as genomic profiling becomes routine. For instance, trastuzumab has revolutionized outcomes in HER2-positive breast cancer, with long-term data supporting durable benefit when added to chemotherapy. Similarly, osimertinib, an EGFR tyrosine kinase inhibitor, has shown substantial benefit in reducing recurrence in resected EGFR-mutant non–small cell lung cancer (NSCLC).
Patient Selection and Precision Medicine in Adjuvant Therapy
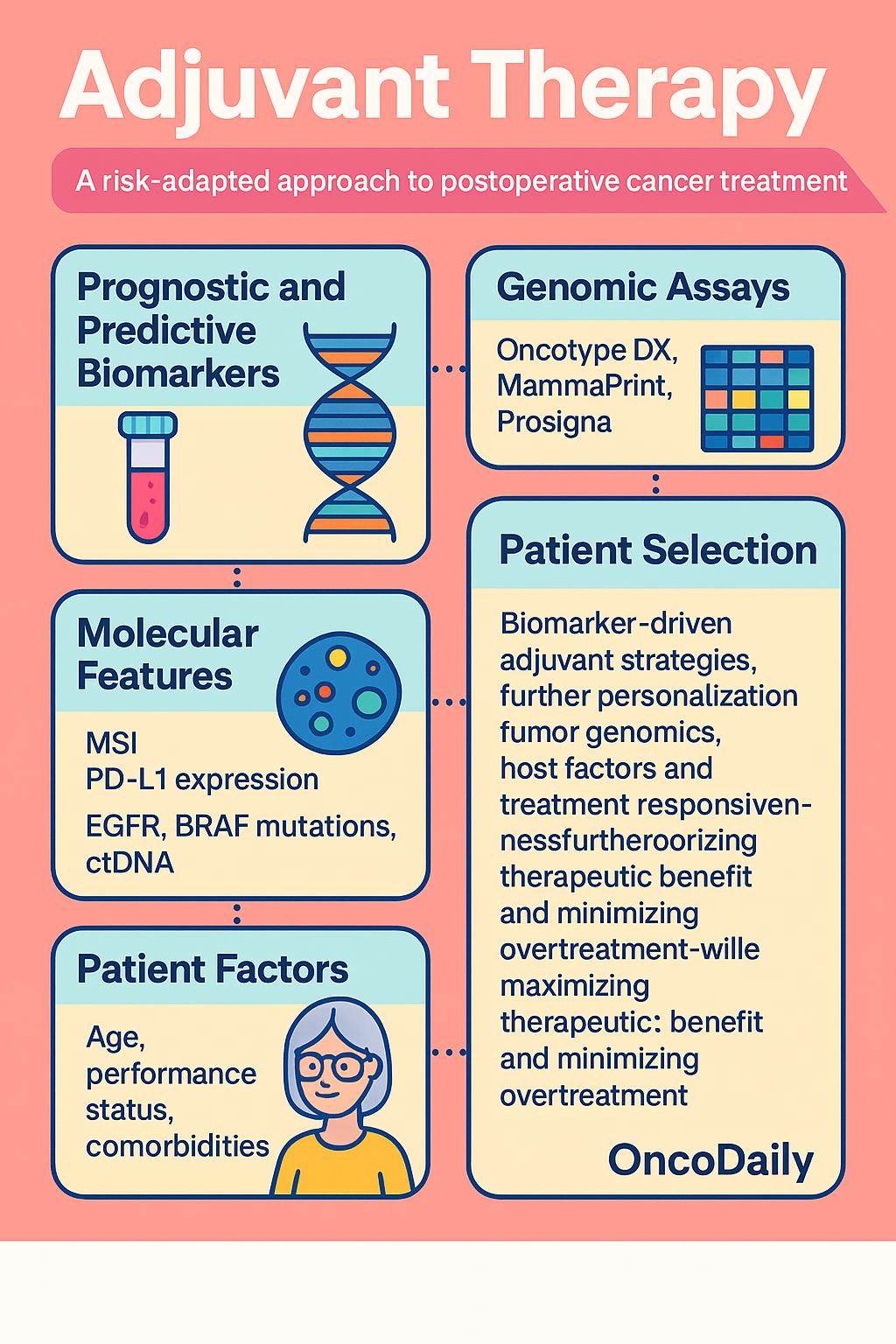
In the era of precision oncology, the decision to administer adjuvant therapy is no longer based solely on traditional staging parameters such as tumor size or nodal involvement. Instead, a personalized risk-adapted approach has emerged, incorporating molecular profiling, genomic assays, and biomarker-driven insights to identify patients most likely to benefit from post-surgical treatment.
A fundamental distinction in this approach lies between prognostic and predictive biomarkers. Prognostic markers provide information about the natural course of the disease, helping to estimate the risk of recurrence, while predictive markers inform treatment response—guiding clinicians on whether a particular adjuvant therapy is likely to be effective. Genomic assays such as Oncotype DX, MammaPrint, and Prosigna (PAM50) are widely used in early-stage hormone receptor–positive breast cancer to assess the risk of distant recurrence and the potential benefit of chemotherapy. These multigene panels stratify patients into low-, intermediate-, or high-risk categories, often allowing many patients to safely avoid unnecessary chemotherapy without compromising outcomes.
Beyond breast cancer, molecular features like microsatellite instability (MSI) in colorectal cancer or PD-L1 expressionin non–small cell lung cancer are increasingly used to determine candidacy for adjuvant immunotherapy, while EGFR mutations, BRAF status, and circulating tumor DNA (ctDNA) are being explored as dynamic tools to personalize adjuvant interventions. Importantly, patient selection also accounts for age, performance status, and comorbidities. In elderly or frail patients, the risks of toxicity may outweigh the potential benefits of aggressive adjuvant regimens. Geriatric assessment tools and patient preference play a crucial role in such cases, ensuring that treatment decisions align with both clinical evidenceand individual goals of care.
As biomarker-driven trials continue to refine adjuvant strategies, the integration of tumor genomics, host factors, and treatment responsiveness will further personalize the adjuvant landscape—maximizing therapeutic benefit while minimizing overtreatment.
Timing, Duration, and Sequencing of Adjuvant Therapy
The success of adjuvant therapy depends not only on selecting the right treatment but also on administering it at the right time, for the appropriate duration, and in the optimal sequence with other modalities. These factors can significantly influence therapeutic efficacy, toxicity, and patient outcomes.
Numerous studies have shown that early initiation of adjuvant therapy following surgery is associated with improved outcomes. For example, in colorectal cancer, delays beyond 8 weeks postoperatively have been linked to reduced overall survival. The rationale is that residual microscopic disease may begin to proliferate soon after surgical removal of the primary tumor, creating a window of vulnerability where systemic therapy is most effective. However, initiating treatment too early—before adequate recovery—can increase complications, highlighting the need to balance urgency with patient readiness.
The duration of adjuvant therapy is another critical consideration. In stage III colon cancer, for instance, the IDEA collaboration compared 3 months vs 6 months of oxaliplatin-based chemotherapy. The findings suggested that for certain lower-risk patients, shorter courses were non-inferior, significantly reducing cumulative toxicity—especially neurotoxicity—without compromising efficacy. Conversely, in breast cancer, longer durations of endocrine therapy (up to 10 years) have been shown to reduce late recurrences in hormone receptor–positive disease, particularly in high-risk subgroups.
Sequencing decisions also play a pivotal role, particularly when multimodal therapy is involved. In breast cancer, adjuvant chemotherapy is typically given before radiotherapy to avoid delays and reduce overlapping toxicities. In other cancers, such as rectal cancer or head and neck malignancies, concurrent chemoradiation may be preferred for synergistic effects and better local control. The ideal sequence is tailored to tumor type, risk of distant metastasis, and anatomical constraints.
Emerging approaches are exploring de-escalation strategies for low-risk patients—aiming to reduce overtreatment and long-term toxicity—as well as intensification protocols for high-risk cases, such as incorporating immunotherapy or extending treatment duration based on circulating tumor DNA (ctDNA) persistence.
Evidence-Based Benefits of Adjuvant Therapy Across Tumor Types
The impact of adjuvant therapy on cancer outcomes is supported by high-level evidence across multiple tumor types, with survival benefits varying by cancer biology, stage, and patient risk profile.
In breast cancer, adjuvant systemic therapy has been a standard for decades. Meta-analyses from the Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) demonstrated that adjuvant chemotherapy and endocrine therapy reduce both recurrence and mortality, particularly over long-term follow-up (EBCTCG, Lancet, 2012). HER2-positive patients benefit from the addition of trastuzumab, as established in the HERA trial (Piccart-Gebhart et al., NEJM, 2005). Risk stratification has been refined with genomic assays such as Oncotype DX and MammaPrint, which guide chemotherapy decisions based on recurrence risk (Sparano et al., NEJM, 2018).
In colon cancer, the role of adjuvant chemotherapy is well established for stage III disease. The MOSAIC trial demonstrated that adding oxaliplatin to 5-FU/LV (FOLFOX) significantly improved disease-free and overall survival (André et al., NEJM, 2004). In stage II, the benefit is limited to patients with high-risk features, and molecular markers like microsatellite instability (MSI) now inform therapy choices (NCCN Guidelines Colon Cancer, 2025).
In non–small cell lung cancer (NSCLC), adjuvant cisplatin-based chemotherapy has shown modest survival benefits in resected stage II–III disease. More recently, targeted therapy with osimertinib in EGFR-mutant tumors (ADAURA trial, Wu et al., NEJM, 2020) and immunotherapy with atezolizumab for PD-L1–positive tumors (IMpower010, Felip et al., Lancet, 2021) have shown superior disease-free survival and are being incorporated into standard practice.
In melanoma, the introduction of adjuvant checkpoint inhibitors represents a major shift. The CheckMate 238 trial demonstrated that nivolumab significantly reduced recurrence risk compared to ipilimumab in resected stage III/IV melanoma (Weber et al., NEJM, 2017), while KEYNOTE-054 showed similar benefit with pembrolizumab (Eggermont et al., NEJM, 2018). These findings have led to routine use of adjuvant immunotherapy in high-risk resected melanoma.
Emerging evidence supports adjuvant therapy in renal, bladder, and gastroesophageal cancers. In renal cell carcinoma, the KEYNOTE-564 trial showed that pembrolizumab improved disease-free survival in high-risk post-nephrectomy patients (Choueiri et al., NEJM, 2021). In bladder cancer, the CheckMate 274 trial demonstrated that adjuvant nivolumab improved DFS post–radical cystectomy (Bajorin et al., NEJM, 2021). In gastric and gastroesophageal junction cancers, perioperative chemotherapy and postoperative chemoradiation have shown improved outcomes in high-risk patients.
Risks, Toxicities, and Limitations of Adjuvant Therapy
While adjuvant therapy offers meaningful survival benefits, it is not without risks. A balanced understanding of its acute and long-term toxicities, along with psychosocial and financial implications, is essential for informed decision-making and responsible clinical application.
Chemotherapy is associated with a broad range of systemic toxicities. Myelosuppression remains a major concern, leading to neutropenia, anemia, and thrombocytopenia, which increase the risk of infection and fatigue. Peripheral neuropathy, particularly from agents like oxaliplatin or taxanes, can persist long after treatment, impacting daily functioning and quality of life. In some regimens, particularly those involving anthracyclines, cardiotoxicity is a serious long-term risk, necessitating cardiac monitoring during and after therapy.
Radiotherapy, though localized, can cause tissue fibrosis, skin reactions, and organ-specific complications depending on the anatomical site. In breast cancer, for example, radiation to the left side has been associated with late cardiac effects, while in head and neck cancers, xerostomia and dysphagia may become chronic. There is also a recognized, though rare, risk of radiation-induced secondary malignancies, particularly in younger patients .
Immunotherapy, especially immune checkpoint inhibitors, has introduced a new class of immune-related adverse events (irAEs). These can affect virtually any organ system—commonly presenting as dermatitis, colitis, pneumonitis, thyroiditis, or hepatitis—and may necessitate immunosuppressive therapy. While often manageable, some irAEs can be life-threatening or permanent, and their unpredictable nature poses a clinical challenge in the adjuvant setting, where patients are otherwise disease-free.
Endocrine therapy in hormone receptor–positive cancers, though generally well tolerated, can significantly affect quality of life. Common symptoms include hot flashes, arthralgia, mood changes, and sexual dysfunction, which can undermine treatment adherence over prolonged treatment durations. Adherence is particularly challenging in younger patients or those experiencing menopausal symptoms without adequate supportive care .
Beyond clinical toxicities, adjuvant therapy may impose substantial financial burdens. The cost of modern regimens, especially those involving targeted therapies or immunotherapies, can be considerable—raising issues of access and affordability. Additionally, prolonged treatment schedules and side effects may lead to work disruptions, emotional distress, and caregiver strain, contributing to broader psychosocial impact. There is also growing recognition of overtreatment concerns. Not all patients who receive adjuvant therapy derive benefit, particularly in settings where molecular or genomic tools are not used to guide decisions. The risk of unnecessary toxicity without survival gain underscores the importance of risk stratification and shared decision-making, especially in low-risk disease.
Innovations and Future Directions in Adjuvant Therapy
Adjuvant therapy is undergoing a profound transformation, driven by advances in molecular diagnostics, trial design, and therapeutic innovation. The traditional one-size-fits-all approach is rapidly being replaced by precision-based strategies that seek to maximize efficacy while minimizing unnecessary treatment.
One of the most promising developments is the use of liquid biopsy—specifically, circulating tumor DNA (ctDNA)—to detect minimal residual disease (MRD) after curative-intent surgery. Unlike imaging or pathology, ctDNA can detect microscopic disease at the molecular level, often months before clinical relapse. Studies in colorectal, breast, and lung cancers have demonstrated that ctDNA positivity post-surgery strongly predicts recurrence, offering a powerful tool to identify patients who may benefit from adjuvant therapy—or conversely, to spare low-risk patients from overtreatment(Tie et al., JAMA Oncol, 2019). Several prospective trials are now testing ctDNA-guided adjuvant strategies.
The adaptive trial model is also reshaping adjuvant therapy research. Trials such as NRG Oncology studies, ALCHEMIST (lung cancer), and IMpower010 (NSCLC) are designed to integrate biomarker selection, treatment stratification, and real-time response assessment. This flexible framework allows for mid-trial modifications, acceleration of promising therapies, and a more efficient path to clinical adoption.
Beyond trial design, advances in artificial intelligence (AI) and integrative genomics are enabling deeper analysis of tumor behavior, host factors, and treatment response. Machine learning algorithms can now process multi-omic data—including genomics, transcriptomics, and proteomics—to predict recurrence risk and personalize adjuvant plans. These tools hold promise for optimizing therapy intensity, sequence, and timing based on individual tumor biology.
On the therapeutic frontier, a new generation of agents is entering the adjuvant space. Antibody-drug conjugates (ADCs), which deliver cytotoxic agents directly to tumor cells via targeted antibodies, are being explored in breast and urothelial cancers. Bispecific antibodies, which engage both tumor antigens and immune effector cells, are another promising class under investigation. The incorporation of these agents into adjuvant regimens may offer greater specificity with fewer off-target effects, especially when guided by biomarkers such as HER2, Trop-2, or DLL3.
You Can Watch More on OncoDaily Youtube TV
Written by Toma Oganezova, MD
FAQ
What is adjuvant therapy in cancer?
It’s treatment given after surgery to eliminate residual cancer cells and reduce recurrence risk.
How does adjuvant therapy differ from neoadjuvant therapy?
Adjuvant is post-surgery, neoadjuvant is pre-surgery to shrink tumors.
Which cancers commonly use adjuvant therapy?
Breast, colon, lung, melanoma, and bladder cancers most commonly benefit from adjuvant treatment.
What types of adjuvant therapies are used?
Chemotherapy, radiotherapy, immunotherapy, endocrine therapy, and targeted agents.
What are the side effects of adjuvant therapy?
Side effects include fatigue, neuropathy, immune reactions, and organ-specific toxicity.
How is adjuvant therapy personalized?
Using biomarkers, genomic assays (e.g., Oncotype DX), and ctDNA to guide who should get treated.
When should adjuvant therapy start after surgery?
Usually within 6–8 weeks postoperatively, balancing urgency and recovery.
How long does adjuvant therapy last?
Duration varies by cancer type and treatment, ranging from a few weeks to several years.
What is ctDNA and how is it used in adjuvant therapy?
Circulating tumor DNA detects residual disease and guides adjuvant treatment decisions.
Are new drugs being tested in the adjuvant setting?
Yes—ADCs, bispecific antibodies, and immune checkpoint inhibitors are under active study.
-
Challenging the Status Quo in Colorectal Cancer 2024
December 6-8, 2024
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023
