Taletrectinib (Ibtrozi): What Patients Should Know About in 2025?
Taletrectinib is a new, targeted cancer drug approved for adults with ROS1-positive non-small cell lung cancer (NSCLC). It belongs to a class of medicines called tyrosine kinase inhibitors (TKIs) and is designed to block the activity of gene fusions that drive certain types of cancer. The U.S. Food and Drug Administration (FDA) granted full approval for Ibtrozi in June 2025, marking an important advancement in treatment for patients with this rare type of lung cancer.
This article explains how Taletrectinib works, the cancers it treats, what patients can expect during treatment, and how to manage side effects. We’ll also explore the results from clinical trials and the future of this promising therapy.
What Is Taletrectinib and How Does It Work?
Taletrectinib, marketed under the brand name Ibtrozi, is an oral, next-generation tyrosine kinase inhibitor (TKI). It works by targeting abnormal proteins that form when two genes—ROS1 or NTRK—fuse together. These fusion proteins act like a stuck accelerator pedal in a car, causing cancer cells to grow uncontrollably. By blocking these fusion proteins, Taletrectinib helps stop the cancer from growing or spreading.
What makes Taletrectinib different from older drugs is its ability to overcome resistance mutations, especially ROS1 G2032R, which often causes earlier treatments like crizotinib to stop working. It also works in the brain, which is important for patients whose cancer has spread to the central nervous system.
What Cancers Does Taletrectinib Treat?
Taletrectinib is currently approved to treat adults with advanced or metastatic ROS1-positive non-small cell lung cancer (NSCLC). This includes patients who:
- Have never received ROS1-targeted therapy, or
- Have already been treated with another ROS1 inhibitor but saw their cancer return or progress.
The drug is not yet approved for NTRK-positive cancers, but research is underway. In the U.S., Taletrectinib is sold as Ibtrozi. In China, it is approved under the name Dovbleron®, and it is being developed for approval in Japan as well.
Clinical Trial Results: How Effective Is Taletrectinib?
Taletrectinib’s FDA approval was based on results from two important clinical trials: TRUST-I, which took place in China, and TRUST-II, an international study. These trials involved 273 patients with advanced ROS1-positive NSCLC. Of these, 160 had not received any ROS1-targeted treatments before, while 113 had previously been treated with such therapies.
In patients who were new to treatment, Taletrectinib achieved a response rate of 88.8%, meaning nearly 9 out of 10 patients saw their tumors shrink. The median duration of response was 44.2 months, and the cancer remained under control for about 45.6 months on average. The drug also showed strong activity in the brain, with a 76.5% intracranial response rate.
Among patients who had previously received ROS1-targeted therapy, the response rate was 55.8%, the median duration of response was 16.6 months, and the cancer stayed controlled for 9.7 months on average. Intracranial responses were also seen in these patients, with a 65.6% brain response rate. These results highlight Taletrectinib’s ability to deliver durable responses both in the body and in the brain, even in patients whose cancer has progressed on earlier treatments.
You can also read about Non-Small Cell Lung Cancer: Causes, Symptoms, Diagnosis, Treatment Options, and Latest 2025 Advances in Targeted and Immunotherapy on OncoDaily.
What Is a Clinical Trial and Why Does It Matter?
A clinical trial is a research study designed to test new drugs and treatments in patients to determine their safety and effectiveness. Before Taletrectinib was approved, it went through multiple phases of clinical trials to assess how well it worked, what side effects it caused, and whether it was better than existing treatments. Clinical trials are essential because they provide scientific evidence that a drug can help patients while ensuring it is safe for widespread use.
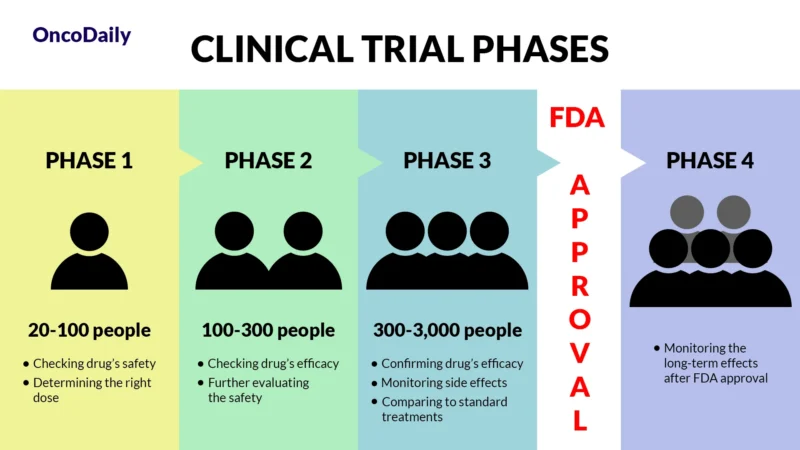
What Does FDA Approval Mean?
When a drug receives FDA approval, it means that after rigorous testing in clinical trials, it has been shown to be both safe and effective for treating a specific condition. This approval makes the drug widely available for doctors to prescribe and helps patients access new, cutting-edge treatments sooner.
Common Side Effects and How to Manage Them?
Like many targeted cancer treatments, Ibtrozi may cause side effects. Some are common and mild, while others are less frequent but more serious. Knowing what to expect and how to manage these effects is important for safe and effective treatment.
Common Side Effects
The most common side effects include stomach problems, tiredness, skin changes, dizziness, and changes in liver function. Diarrhea affects over half of patients, often in the first few weeks, and can usually be managed with fluids, diet changes, and medications like loperamide. Nausea and vomiting are also common but often improve with anti-nausea drugs and taking the medication on an empty stomach.
Fatigue occurs in about 1 in 5 people. Light activity, rest, and healthy meals can help. Dizziness is usually mild and short-lived, but it’s best to avoid driving if it happens. Some patients may get a skin rash, especially in sun-exposed areas, which can be eased with sunscreen and moisturizers. Liver enzyme changes are common and usually found through routine blood tests. Less frequent symptoms include appetite changes, dry mouth, and constipation—often manageable with simple adjustments.
Less Common Side Effects
Rare but serious side effects include heart rhythm changes (QT prolongation), which require ECG monitoring, and lung inflammation (ILD or pneumonitis), which should be checked right away if new breathing problems appear.
Other uncommon effects include high uric acid levels, muscle issues, and, in some cases, bone fractures. Sun sensitivity is also possible, so daily sunscreen and protective clothing are advised.
Managing Side Effects
Most side effects can be managed with regular monitoring, supportive medications, and early communication with your healthcare team. Liver and heart function are routinely checked with blood tests and ECGs. Side effects like diarrhea, fatigue, and rash can often be controlled. More serious symptoms, especially breathing issues, should be reported immediately. With proper care, many patients can stay on treatment and maintain quality of life.

How Long Does Taletrectinib Work?
In clinical studies, Taletrectinib provided long-lasting control of ROS1-positive NSCLC, especially in patients who had never received targeted therapy before. Many patients remained progression-free for more than three years. Even patients who had previously taken another ROS1 inhibitor benefited from treatment, experiencing meaningful tumor shrinkage and delayed cancer progression. The drug is also highly effective against brain metastases, helping patients with central nervous system involvement maintain control of their disease. Although Taletrectinib is not a cure, it offers an important tool for managing cancer over the long term and improving quality of life.
Recommended Dosage of Taletrectinib
Taletrectinib is typically prescribed at a dose of 600 mg once daily, taken by mouth. It is supplied in 200 mg capsules, and most patients take three capsules at the same time each day. Treatment continues until the cancer progresses or side effects become unmanageable.
If side effects occur, the dose may be reduced in steps—first to 400 mg daily, and then to 200 mg daily. In cases where even the lowest dose cannot be tolerated, treatment may be permanently discontinued. Before starting therapy, patients usually undergo tests to check liver function, heart rhythm, and other baseline health indicators.
How Taletrectinib Is Taken?
Taletrectinib capsules should be swallowed whole with water and taken on an empty stomach. Patients are advised not to eat for at least two hours before and two hours after taking the medication. The capsules should not be opened, crushed, or chewed.
It is important to take the drug at the same time every day. If a dose is missed or vomited, patients should skip it and resume with the next scheduled dose. Taking extra doses to make up for a missed one is not recommended. While on Taletrectinib, patients should avoid grapefruit and grapefruit juice, as these can affect how the drug is metabolized. If antacids or acid-suppressing medications are needed, they should be taken at least two hours apart from Taletrectinib to avoid interference with absorption.
Metabolism and Half-Life of Taletrectinib
Taletrectinib is processed in the body primarily by CYP3A enzymes, as well as by non-CYP450 pathways such as sulfation and acetylation. It is also partly metabolized by CYP2C8 and CYP2C9 enzymes. These pathways help break down the drug and prepare it for elimination.
The drug has a long half-life of approximately 66 hours, which means it remains active in the body for several days after each dose. Most of the drug is excreted through the feces (about 75%), with a smaller portion eliminated in the urine (around 11%). This long half-life supports once-daily dosing and helps maintain steady drug levels in the bloodstream over time.
What to Avoid During Treatment?
While taking Taletrectinib, certain precautions are necessary. Patients should avoid grapefruit and grapefruit juice, as these can interfere with how the drug is processed in the body. Antacids can affect how Taletrectinib is absorbed, so they should be taken at least two hours apart from your dose.
You should also avoid medications that could impact your heart rhythm or liver function unless your doctor approves them. Because dizziness is possible, avoid driving or activities requiring alertness if you feel unsteady. Patients should also avoid live vaccines during treatment and always check with their doctor before receiving any new vaccines or starting supplements.
Real-World Effectiveness
Outside of clinical trials, Taletrectinib continues to show promise. In real-world settings, it is helping patients with advanced NSCLC, especially those with brain metastases. Doctors report that the drug is well tolerated, offers long-lasting benefits, and can be safely integrated into everyday cancer care. These results provide additional confidence in the drug’s role as a frontline treatment option for eligible patients.
Looking Ahead: The Future of Taletrectinib
Taletrectinib represents an exciting development in precision oncology, offering a targeted treatment for a specific genetic alteration. Ongoing studies may lead to its use in other cancers, such as breast cancer with CDH1 mutations or other ROS1- or NTRK-driven tumors. Researchers are also exploring how Taletrectinib could be combined with other therapies to improve outcomes even further.
Read more about Metastatic Lung Cancer: Causes, Symptoms, Treatment, and 2025 Advances in Therapy on OncoDaily.
Ongoing Clinical Trials with Taletrectinib
Taletrectinib is being further studied in other cancer types. One ongoing Phase II trial (NCT06214793) is focused on patients with metastatic invasive lobular breast cancer (ILC) that carries a mutation in the CDH1 gene. This mutation affects a protein called E-cadherin, and research suggests it may activate ROS1, making such cancers responsive to ROS1 inhibitors like Taletrectinib. The trial is enrolling patients who have previously received other treatments and aims to determine how effective the drug is in this specific subtype of breast cancer.
Another real-world study is taking place to observe how Taletrectinib performs in routine clinical care. This study (NCT07008287) includes patients with ROS1-positive NSCLC and brain metastases. It is non-interventional, meaning Taletrectinib is given as part of standard medical care, and researchers are collecting data on how patients respond, how long the treatment works, and what side effects occur.
Taletrectinib (Ibtrozi) represents an exciting advancement for patients with ROS1-positive non-small cell lung cancer. With its ability to overcome resistance mutations, control brain metastases, and provide long-term disease management, it offers new hope to many people living with advanced cancer.
If you’re a healthcare provider, access the professional version here.
-
Challenging the Status Quo in Colorectal Cancer 2024
December 6-8, 2024
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023
