
Is Cancer Hereditary? Myths and Facts about Cancer Genetics
While many people fear that a cancer diagnosis in the family means they are destined to face the same fate, the truth is more nuanced. Not all cancer is hereditary—but genetics can play a significant role in cancer risk. Understanding the difference between inherited mutations and other risk factors is key to informed decision-making. In this article, we explore the role of genetics in cancer, including how inherited mutations contribute to only a small percentage of all cancer cases. We’ll also cover how genetic testing works, what it means for prevention and treatment, and who should consider it. This guide helps clarify what makes a cancer hereditary and what does not.
What Does It Mean If Cancer Runs in a Family?
Many families may observe multiple cancer cases among relatives and assume the cause is purely genetic. However, it’s important to distinguish between familial cancer patterns and hereditary cancer. Familial cancers occur more frequently within a family than expected by chance, but they are often linked to shared environmental exposures, lifestyle habits (like diet, smoking, or alcohol use), or even socioeconomic factors—not necessarily inherited gene mutations.
In contrast, hereditary cancers result from specific genetic mutations passed down through generations. These mutations significantly increase a person’s lifetime risk of developing certain types of cancer. For example, multiple cases of breast cancer in a family might be due to a shared BRCA1 or BRCA2 mutation—an indicator of hereditary breast and ovarian cancer syndrome.
A thorough three-generation family history is crucial for healthcare providers to assess cancer risk accurately. Red flags include early-onset cancers (before age 50), rare cancer types, multiple cancers in one person, and patterns across several generations. According to the American Cancer Society, only 5–10% of all cancers are caused by inherited genetic mutations, while 15–20% may cluster in families due to shared behaviors or environments. The rest occur sporadically, without a clear familial or hereditary link.
Understanding this distinction helps guide decisions about genetic counseling, testing, and personalized cancer screening strategies.
How to Identify a Family History of Cancer
Identifying a family history of cancer is a key step in understanding your personal risk and determining whether genetic counseling or testing may be appropriate. Start by gathering information about both your maternal and paternal relatives, ideally covering at least three generations—including grandparents, parents, siblings, aunts, uncles, and cousins.
As you speak with relatives, focus on collecting details such as the type of cancer diagnosed, the age at diagnosis, whether the individual had multiple types of cancer, their current age or age at death (and the cause, if known), and their ethnic background, as certain inherited cancers are more common in specific populations.
There are several red flags that may suggest a hereditary cancer syndrome. These include multiple close relatives with the same or related types of cancer, cancer diagnosed at an unusually young age (typically before age 50), individuals who have developed more than one primary cancer, and the presence of rare cancers such as male breast cancer or medullary thyroid cancer.
It’s helpful to organize this information into a written or digital family cancer history chart or pedigree. Sharing this with your healthcare provider or a genetic counselor can help determine whether genetic testing might be recommended, or if earlier or more frequent cancer screening is warranted.
Genetic Red Flags in Family History
Certain patterns in a family’s cancer history may point to a potential hereditary cancer syndrome. One of the most telling signs is a diagnosis of cancer at an unusually young age—often before the age of 50—when most cancers typically develop later in life. Another red flag is when the same type of cancer appears repeatedly in close family members across multiple generations, such as breast, ovarian, or colon cancer.
A family history that includes individuals with more than one primary cancer—meaning they’ve been diagnosed with different types of cancer at different times—can also signal an inherited genetic mutation. The presence of rare or gender-atypical cancers, like breast cancer in men or early-onset pancreatic cancer, may further suggest a hereditary risk.
Additionally, cancers that occur in both paired organs, such as bilateral breast or kidney cancer, or combinations of cancers known to be linked by genetics (like breast and ovarian cancer or colon and endometrial cancer), are important indicators. If you observe these patterns in your family, it may be time to consult a genetic counselor to evaluate your inherited risk and discuss potential next steps.
What is Hereditary Cancer?
Hereditary cancer refers to cancers caused by inherited genetic mutations that significantly increase a person’s risk of developing certain types of cancer. These mutations are passed down from parent to child through DNA and are present in all cells of the body from birth.
Unlike most cancers, which result from genetic changes acquired over a person’s lifetime due to environmental exposures, aging, or random errors during cell division, hereditary cancers are linked to germline mutations—changes in specific genes that are inherited and can be traced through families. Common examples include mutations in the BRCA1 and BRCA2 genes, which are strongly associated with breast and ovarian cancers, and MLH1, MSH2, and other mismatch repair genes involved in Lynch syndrome, which increases the risk of colorectal and other cancers.
Although many people worry about cancer “running in the family,” only about 5% to 10% of all cancers are truly hereditary, according to the National Cancer Institute. Understanding whether a cancer is hereditary is important, as it can influence not only the patient’s treatment and surveillance but also provide valuable insights for at-risk family members.
Identifying these inherited mutations through genetic testing allows for targeted prevention, early detection, and personalized care strategies, helping reduce the impact of cancer across generations.
Hereditary vs. Sporadic Cancer: What’s the Difference?
Hereditary and sporadic cancers differ primarily in their origin and underlying genetic cause.
Hereditary cancers are caused by inherited genetic mutations passed from a parent to their child. These mutations are present in every cell of the body from birth and significantly increase the risk of developing certain cancers, often at a younger age than usual. For example, someone who inherits a mutation in the BRCA1 gene has a much higher lifetime risk of breast and ovarian cancer. These cancers often show family patterns, with several close relatives affected by the same or related types of cancer across generations.
In contrast, sporadic cancers are the result of random mutations that occur over a person’s lifetime. These changes can be caused by factors like aging, environmental exposures (such as tobacco smoke or UV radiation), lifestyle choices, or simply by chance. These mutations are not inherited and are only present in the cancer cells—not the rest of the body. Most cancers fall into this category. For example, a person who develops lung cancer after decades of smoking likely has a sporadic form of the disease.
While hereditary cancers account for only 5–10% of all cancer cases, they are important to recognize because they carry implications for both the individual and their relatives. Sporadic cancers, which make up the vast majority of diagnoses, generally occur without a clear inherited risk and are not typically passed down through families.
Understanding the Role of Genetics in Cancer
DNA mutations drive cancer development by disrupting the normal regulation of cell growth, often through accumulated genetic alterations in key oncogenes and tumor suppressor genes. Recent research has underscored the importance of clustered mutations—simultaneous alterations affecting multiple genes and signaling pathways—in accelerating malignant transformation. These mutations contribute to genomic instability, impair DNA repair mechanisms, and enable cancer cells to proliferate uncontrollably, spread to distant sites, and resist conventional therapies. Yi Li Int Mol Sci 2024
Among the most well-studied genetic contributors to cancer are the tumor suppressor genes BRCA1 and BRCA2, which are essential for repairing double-stranded DNA breaks via homologous recombination. Mutations in these genes compromise DNA repair efficiency, resulting in the accumulation of genetic errors that drive carcinogenesis.
BRCA1 mutations are closely associated with triple-negative breast cancer, with approximately 70% of BRCA1-related cases lacking estrogen, progesterone, and HER2 receptors—features that complicate standard treatment. Pathogenic variants in BRCA1 have also been linked to increased lifetime risks for pancreatic and stomach cancers, with absolute risks estimated at around 2.5% and 2%, respectively, by age 80. Notably, de novo BRCA1 mutations, although rare, have been documented—such as in a 30-year-old woman with hormone-positive breast cancer and no family history—highlighting the potential for spontaneous mutations in early-onset disease. Shuai Li J Clin Oncol 2022
Will Barnet, (Beverly 1911 – New York 2012), Four generations, 1984, Oil on canvas, 100 x 130 cm
BRCA2 mutations present different risk patterns. Carriers face a 27% cumulative risk of prostate cancer by age 80, significantly higher than those with BRCA1 mutations. Male breast cancer is also more commonly associated with BRCA2, with an absolute risk of 6.8% by age 80—markedly above the population average. Emerging evidence also links BRCA2 variants to increased susceptibility to biliary tract and esophageal cancers, with odds ratios reported at 17.4 and 5.6, respectively.
These associations carry important clinical implications. Individuals with BRCA1 or BRCA2 mutations benefit from enhanced cancer screening protocols, such as breast MRI for women and prostate-specific antigen (PSA) testing for men. Additionally, tumors harboring BRCA mutations often respond to PARP inhibitors, which exploit a vulnerability in DNA repair pathways through a mechanism known as synthetic lethality.
Recent case studies support the need for broader genetic testing criteria. A 2023 report described a de novo BRCA1 mutation (c.4065_4068delTCAA) in a young breast cancer patient who would not have qualified for testing under traditional guidelines. Another study published in 2022, involving 5,341 BRCA2 carriers, revealed that the relative risk of stomach cancer was 6.89 times higher in women and 2.76 times higher in men compared to non-carriers.
These findings highlight the growing spectrum of BRCA-related cancers and reinforce the importance of personalized risk assessment, early detection, and tailored interventions in hereditary cancer care.
Debunking Myths About Hereditary Cancer
Many people misunderstand hereditary cancer, leading to unnecessary fear or false reassurance. In reality, only 5–10% of cancers are caused by inherited mutations—most result from aging, lifestyle, or environmental factors. Carrying a gene like BRCA1 increases risk but doesn’t guarantee cancer, and both parents can pass down these mutations. A negative BRCA test doesn’t rule out hereditary cancer, as many other genes may be involved. Family history often reflects shared habits, not just genetics. The key is personalized care—genetic counseling, testing, and healthy choices can help prevent or manage most cancer risks.
Does Having a Family History Mean You Will Get Cancer?
A family history of cancer does not equate to an inevitable diagnosis. While genetic predispositions play a role in some cancers, most cases arise from complex interactions between inherited mutations, environmental factors, and lifestyle choices. Below, we clarify this using evidence from scientific studies.
Genetic Mutations vs. Environmental Factors
Only 5–10% of cancers are directly linked to inherited genetic mutations, such as BRCA1/2 (breast/ovarian cancer) or MLH1/MSH2 (Lynch syndrome). The majority of cancers result from acquired mutations due to aging, environmental exposures (e.g., smoking, UV radiation), or lifestyle factors (e.g., diet, alcohol). For example smoking accounts for ~85% of lung cancers, even in families with a cancer history. Obesity increases colorectal cancer risk independently of genetic background.
Environmental factors often explain familial cancer clusters more than heredity. Families sharing habits like smoking or poor diet may show similar cancer patterns without a genetic link.
Lynch Syndrome Families
Even among carriers of MLH1/MSH2 mutations, colorectal cancer risk varies widely. Some families with these mutations show no cancer cases due to protective genetic modifiers or lifestyle factors (e.g., high-fiber diets).
Cancer-Free Families (CFFs)
A study of 51 elderly individuals with no personal/family cancer history found fewer high-risk genetic variants (e.g., BRCA1/2) compared to the general population. This suggests that some families avoid passing down predisposing mutations. Guoqiao Zheng 2020 Cancers (Basel)
Male Infertility and Cancer Risk
Relatives of men with infertility (a potential genetic marker) show elevated risks for specific cancers (e.g., thyroid, colon). However, not all relatives develop cancer, highlighting the role of non-genetic factors like shared environmental exposures.
Are Men Exempt from Hereditary Cancer Risks?
Only women need to worry about hereditary cancer risks, this is a common misconception. Men also face significant hereditary cancer risks, particularly related to BRCA1 and BRCA2 mutations, which impact male breast and prostate cancers.
Elwes Family, Three Generations of the, 1920, Oil on canvas 208 x 170 cm (81.89 x 66.93 in.)
BRCA Mutations and Male Breast Cancer
Men carrying BRCA2 mutations have an estimated 6–8% lifetime risk of developing breast cancer, which is significantly higher than the general male population risk of about 0.1%. Although male breast cancer is rare, BRCA mutations markedly increase this risk and often present at younger ages.
BRCA Mutations and Prostate Cancer
Hereditary prostate cancer has one of the highest heritability rates among common cancers, estimated at around 58%. Pathogenic variants in BRCA2 and BRCA1 significantly increase prostate cancer risk and are associated with more aggressive disease. For example, men with BRCA2 mutations have a 2 to 6-fold increased risk of developing prostate cancer compared to non-carriers. Additionally, mutations in other DNA repair genes (e.g., ATM, CHEK2) also contribute to hereditary prostate cancer risk. Cristina V Berenguer Curr Oncol 2023
Statistical Evidence
- A study found 4.6% of men with prostate cancer carried pathogenic BRCA1/2 variants, even without prior genetic testing.Mary Pritzlaff MS, Natrue 2020
- Familial prostate cancer accounts for about 26.4% of cases, with DNA repair gene mutations dominating the hereditary landscape. Kari Hemminki, Hered Cancer Clin Pract 2025
- Men with BRCA mutations are more likely to develop early-onset and aggressive prostate cancer, underscoring the importance of genetic screening.
Clinical Implications
Men with a family history of breast, ovarian, pancreatic, or Lynch syndrome–associated cancers should consider genetic counseling and testing, as these mutations affect cancer risks across genders. Identification of mutations can guide targeted screening and treatment, including use of PARP inhibitors and immunotherapies in advanced prostate cancer.
In summary, hereditary cancer risk is not exclusive to women. Men with BRCA and related mutations face elevated risks for breast and prostate cancers, warranting awareness, genetic evaluation, and appropriate surveillance.
Does a Lack of Family History Mean You’re Safe?
Not having a family history of cancer does not eliminate an individual’s risk. Research shows that many cancers arise from sporadic (acquired) mutations, which occur over a person’s lifetime due to DNA replication errors, environmental exposures, or lifestyle factors like smoking, poor diet, and UV radiation.
A large population study found that while 35.6% of adults report a family history of cancer, most cancers develop in people without one. Additionally, individuals with hereditary cancer-related mutations but no first-degree family history still face a measurable—though generally lower—risk. This shows that family history influences, but does not solely determine, cancer risk.
Lifestyle factors play a major role, regardless of genetics. Healthy behaviors such as maintaining a balanced diet, avoiding tobacco, limiting alcohol, and staying physically active can significantly reduce cancer risk. For instance, smoking increases lung cancer risk regardless of family history, and obesity contributes to colorectal and breast cancers in both hereditary and sporadic cases.
In summary, cancer risk is multifactorial. Most cancers result from a mix of sporadic mutations, environmental exposures, and lifestyle factors. Family history is important, but its absence does not mean immunity. Prevention through healthy living is essential for everyone.
Can Genetic Testing Guarantee You Won’t Get Cancer?
A negative genetic test result means that no harmful genetic mutations were detected in the genes tested, but it does not eliminate a person’s overall cancer risk. Genetic testing identifies specific inherited mutations known to increase cancer risk, such as those in BRCA1 or BRCA2, but it cannot account for all possible genetic changes or environmental and lifestyle factors that contribute to cancer development.
For example, a “true negative” result—when a known family mutation is absent—indicates the tested individual likely has the same cancer risk as the general population. However, if no familial mutation is known, a negative result is considered “uninformative,” meaning there could still be unknown genetic factors at play. Moreover, cancer can arise from sporadic mutations acquired during life due to aging, exposure to carcinogens, or other risk factors such as smoking, diet, and UV radiation, none of which are detected by inherited genetic testing.
Therefore, even with a negative genetic test, individuals should continue appropriate cancer screening based on their personal and family history and maintain healthy lifestyle practices. Genetic counseling is essential to interpret test results accurately and guide ongoing risk management.
Is Hereditary Cancer the Most Common Type?
The belief that most cancers are hereditary is incorrect. Scientific evidence demonstrates that the vast majority of cancers are sporadic, meaning they arise from mutations acquired during a person’s lifetime rather than inherited genetic mutations. For example, studies show that only about 5% of breast and ovarian cancers are attributable to inherited mutations in genes like BRCA1 or BRCA2, while the remaining 90–95% are sporadic and result from somatic mutations and environmental exposures. Similarly, in colon cancer, only a small subset is due to inherited syndromes such as familial adenomatous polyposis (FAP), while the majority develop sporadically through the accumulation of mutations over time.
Sporadic cancers are influenced by factors such as aging, lifestyle, and environmental exposures (e.g., smoking, diet, UV radiation). Even in families with multiple cancer cases, these may occur by chance or due to shared non-genetic risk factors rather than a hereditary syndrome.
Do Only Older People Develop Hereditary Cancer?
The myth that hereditary cancers only occur later in life is incorrect. Scientific evidence shows that hereditary cancers often present at younger ages compared to sporadic cases. Studies indicate that a significant portion of early-onset cancers—diagnosed before age 50—are linked to genetic predispositions. For example, one study found that 19.2% of early-onset cancers harbor germline pathogenic variants, and many of these mutations are associated with high-penetrance genes like BRCA1, BRCA2, and others (source). Zsofia Kinga Stadler. Journal Clinical Oncology, 2023
Research also highlights that early-onset cancers—such as colorectal, breast, and CNS cancers—are often diagnosed in individuals under 50, sometimes even in their 20s or 30s, and tend to be more aggressive. For instance, familial aggregation studies show that cancers like colorectal and CNS are significantly more common at younger ages in families with inherited syndromes (sources,).
Moreover, specific cancers such as hereditary breast and ovarian cancers, Lynch syndrome-associated colorectal cancers, and certain brain tumors frequently occur in younger individuals due to germline mutations. These early-onset cases are often less responsive to standard treatments and require more aggressive management.
Are All Types of Cancer Linked to Genetics?
While genetics can influence the risk of many cancers, most cancers are not directly linked to hereditary mutations. According to recent studies, over 90% of cancers are primarily caused by environmental and lifestyle factors, with only a small proportion (around 5–10%) attributable to inherited genetic mutations (sources,). Abdulmalik Idris Koya 2024
Cancers with strong hereditary links include breast, ovarian, and colon cancers, where germline mutations such as BRCA1/2 for breast and ovarian cancers, and APC or MLH1 for colon cancers, significantly increase risk (sources,). Conversely, many other cancers—such as lung, skin, and stomach cancers—are largely influenced by environmental exposures like tobacco smoke, UV radiation, and carcinogenic chemicals, rather than inherited mutations (sources,).
This distinction underscores that most cancers develop due to acquired mutations caused by external factors, emphasizing the importance of lifestyle and environmental risk reduction strategies alongside genetic screening.
Can Lifestyle Choices Negate Hereditary Cancer Risks?
While inherited genetic mutations significantly increase cancer risk, healthy lifestyle habits cannot completely eliminate that risk. Recent evidence shows that adopting behaviors such as avoiding tobacco and excessive alcohol, maintaining a healthy weight, eating a balanced diet, and engaging in regular physical activity can mitigate but not fully prevent cancers linked to hereditary mutations. Pasquale Marino Nutrients 2024
For example, a study published in Cancer Research found that individuals with high genetic risk who maintained healthy lifestyles had substantially lower cancer incidence than those with unhealthy habits, demonstrating that lifestyle factors can modify but not erase inherited risks. Similarly, lifestyle changes can influence how the body responds to cancer-promoting factors, potentially delaying onset or improving outcomes, but they do not alter the underlying genetic predisposition.
Therefore, balancing lifestyle modifications with regular medical monitoring and screening is crucial, especially for those with known hereditary mutations. Genetic counseling and surveillance enable early detection and preventive interventions, complementing healthy habits to reduce overall cancer burden.
Does Everyone Need Genetic Testing?
Genetic testing is not recommended for everyone; it is typically advised for individuals with significant family history or specific risk factors suggestive of hereditary cancer syndromes. According to the National Cancer Institute and other expert guidelines, testing is most appropriate when there is:
A family member with a known inherited harmful genetic mutation
- Cancer diagnosed at a young age (e.g., colon cancer before age 50)
- Multiple relatives affected by the same or related cancers (breast, ovarian, colon)
- Rare cancers or multiple cancers in the same individual
- Certain ethnic backgrounds with higher mutation prevalence (e.g., Ashkenazi Jewish ancestry)
Genetic counseling plays a critical role before and after testing. Counselors assess family and personal history to determine if testing is warranted, help interpret results, and guide management decisions. They ensure patients understand the implications, limitations, and possible outcomes of testing. This targeted approach avoids unnecessary testing in low-risk individuals and focuses resources on those most likely to benefit.
The American College of Obstetricians and Gynecologists (ACOG) emphasizes the importance of regularly updating family history and referring patients with positive findings for genetic services. The goal is to provide personalized risk assessment and appropriate preventive care rather than universal testing.
Types of Cancers with Hereditary Links
Healthy habits—such as not smoking, maintaining a healthy weight, exercising, and eating well—can significantly reduce cancer risk, even in individuals with high genetic susceptibility. However, these habits cannot eliminate the risk posed by inherited genetic mutations. Recent large-scale studies show that while a favorable lifestyle lowers cancer incidence among those at high genetic risk (e.g., reducing 5-year cancer incidence from 7.23% to 5.51% in men and from 5.77% to 3.69% in women), the risk remains higher than in those without genetic predisposition. Therefore, individuals with inherited mutations should balance healthy living with regular medical monitoring and personalized screening to effectively manage their cancer risk.
Is Colon Cancer Hereditary?
Lynch syndrome, or hereditary nonpolyposis colorectal cancer (HNPCC), is the most common inherited cause of colon cancer, responsible for about 3% of all colorectal and endometrial cancers. It is an autosomal dominant disorder caused by inherited mutations in mismatch repair (MMR) genes—primarily MLH1, MSH2, MSH6, PMS2, and deletions in EPCAM that impact MSH2 function. These genes normally fix DNA replication errors; when mutated, they lead to microsatellite instability and accumulation of mutations that drive cancer development.
People with Lynch syndrome face a significantly increased lifetime risk of colorectal cancer, often developing it before age 50. The syndrome also elevates risk for endometrial, ovarian, stomach, small intestine, urinary tract, brain, and skin cancers. While early-onset colon polyps may occur, they are not necessarily more numerous than in the general population. Each child of a mutation carrier has a 50% chance of inheriting the mutation, though incomplete penetrance means not all carriers develop cancer.
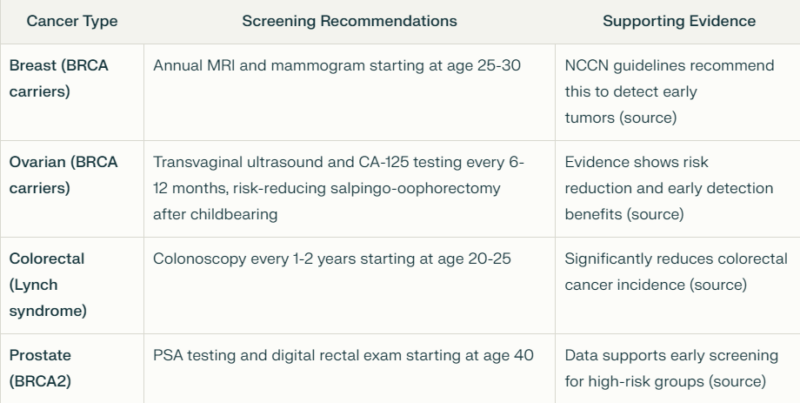
Screening recommendations include colonoscopy starting at age 20–25 or 2–5 years earlier than the youngest diagnosis in the family, repeated every 1–2 years. Women should be screened for endometrial cancer, and genetic counseling and testing are advised for at-risk relatives. Early and routine screening significantly reduces cancer-related morbidity and mortality by enabling detection at a treatable stage.
Diagnosis of Lynch syndrome involves family history, tumor testing (microsatellite instability or immunohistochemistry), and germline genetic testing, all of which are essential for guiding management and prevention strategies.
You Can Also Read ColoSense: Advancing Noninvasive Colorectal Cancer Screening Through Innovative Diagnostics by Oncodaily
Is Pancreatic Cancer Hereditary?
Hereditary pancreatic cancer accounts for approximately 10% of all pancreatic cancer cases, with the remaining 90% attributed to sporadic causes, particularly modifiable risk factors such as tobacco and alcohol abuse. This hereditary component manifests through various cancer syndromes and familial patterns. Familial Pancreatic Cancer (FPC) is defined as pancreatic cancer occurring in a patient with at least two first-degree relatives with pancreatic cancer, without an identified genetic cause. This accounts for a significant portion of hereditary cases, though specific causative genes often remain unidentified.
Several hereditary cancer syndromes are associated with increased pancreatic cancer risk:
- Peutz-Jeghers Syndrome: Caused by mutations in the STK11 gene, this syndrome confers the highest relative risk at 139.7-fold and a lifetime risk of 11-36%.
- Hereditary Pancreatitis: Associated with mutations in PRSS1 and SPINK1 genes, this condition involves recurrent or chronic pancreatitis beginning in childhood or adolescence. It carries a 59-67-fold increased relative risk and a lifetime risk of 7.2-18.8% for pancreatic cancer. The risk significantly increases after age 50, particularly in smokers and diabetics.
- Familial Atypical Multiple Mole Melanoma (FAMMM): Linked to CDKN2A mutations, this syndrome increases pancreatic cancer risk 13.1-22-fold with a lifetime risk of approximately 17%.
- Hereditary Breast and Ovarian Cancer Syndrome: BRCA2 mutations confer a 3.5-10-fold increased risk with a lifetime risk of 4.9%, while BRCA1 mutations present a 2.3-fold increased risk with a 1% lifetime risk.
- Lynch Syndrome: Caused by mutations in mismatch repair genes (MLH1, MSH2, MSH6, PMS2, EpCAM), this syndrome carries an 8.6-fold increased risk with a 3.7% lifetime risk of pancreatic cancer.
Other relevant genes include PALB2 (2.4-fold risk), ATM (4.2-fold risk), TP53 in Li-Fraumeni syndrome (7.3-fold risk), and APC in Familial Adenomatous Polyposis (4.5-fold risk with 1.7% lifetime risk).
Next-generation sequencing has identified new susceptibility genes like PALB2 and ATM, which participate in homologous recombination repair. Interestingly, some sporadic cases that don’t meet FPC criteria also harbor similar mutations, suggesting that relying solely on family history for genetic testing might overlook some carriers.
For treatment, promising approaches include poly (ADP-ribose) polymerase inhibitors for BRCA-mutated cases and immune checkpoint inhibitors for mismatch repair deficient cases, with clinical trials currently underway.
While hereditary pancreatic cancer represents a minority of cases, studying these genetic predispositions provides valuable insights into the etiology, pathogenesis, and potential treatment approaches for pancreatic cancer more broadly.
Is Thyroid Cancer Hereditary?
Genetic mutations play a significant role in the development of thyroid cancer, particularly medullary thyroid cancer (MTC) and syndromes like Multiple Endocrine Neoplasia type 2 (MEN2). Approximately 25% of MTC cases are hereditary, primarily linked to germline mutations in the RET proto-oncogene, which is inherited in an autosomal dominant pattern (source). These hereditary cases are strongly associated with MEN2 syndromes, including MEN2A and MEN2B, with RET mutations present in over 95% of MEN2-related MTC cases (source).

In hereditary MTC, RET mutations are highly prevalent; for example, in MEN2A, mutations in exon 11—particularly at codon 634—account for about 85% of mutations, while in MEN2B, the RET M918T mutation in exon 16 is found in approximately 95% of cases (source,). These mutations confer a high risk of early-onset, aggressive MTC, with penetrance approaching 95% in mutation carriers (source).
In sporadic MTC, somatic RET mutations are also common, detected in 43–71% of cases, with an increase to 85% in metastatic and advanced tumors, especially involving the M918T mutation (source,). Besides RET, mutations in RAS genes (NRAS, HRAS, KRAS) are present in about 35.4% of thyroid cancers overall, with RAS mutations being more common in sporadic cases and associated with less aggressive disease (source).
In summary, RET mutations are central to hereditary MTC and are present in a large proportion of familial cases, with specific mutations correlating with disease severity and age of onset. Sporadic cases also frequently harbor somatic RET mutations, especially in advanced disease, emphasizing the importance of genetic testing for risk assessment and management.
What Are Hereditary Cancer Syndromes?
Lynch Syndrome (LS)
Lynch syndrome, also called hereditary nonpolyposis colorectal cancer (HNPCC), is the most common inherited cause of colorectal and endometrial cancers. It is caused by germline mutations in mismatch repair (MMR) genes—MLH1, MSH2, MSH6, PMS2, or EPCAM. These mutations impair DNA repair, leading to microsatellite instability and increased cancer risk. LS follows an autosomal dominant inheritance pattern, meaning each child of a carrier has a 50% chance of inheriting the mutation.
- Cancer Risks: LS significantly increases lifetime risks of colorectal and endometrial cancer, varying from 10–80% depending on the mutated gene. Additional risks include ovarian, gastric, pancreatic, small bowel, and urothelial cancers. UK Biobank data estimate CRC incidence at 11.8% and endometrial cancer at 13.4% by age 70 in mutation carriers—substantially higher than in the general population.
- Screening: Intensive surveillance is essential, including colonoscopy every 1–2 years starting at age 20–25. Women should also be monitored for endometrial and ovarian cancer.
Li-Fraumeni Syndrome (LFS)
LFS is a rare, autosomal dominant cancer syndrome caused by germline TP53 mutations. This tumor suppressor gene regulates the cell cycle, DNA repair, and apoptosis.
- Cancer Risks: LFS is linked to a broad range of early-onset cancers, including breast cancer, soft tissue and bone sarcomas, brain tumors, leukemia, and adrenocortical carcinoma. Lifetime cancer risk is extremely high, approaching 70–90% by age 70.
- Screening: Surveillance often follows the Toronto protocol, including annual whole-body and brain MRI and early breast cancer screening in women, starting in childhood.
Familial Adenomatous Polyposis (FAP)
FAP is an autosomal dominant condition caused by mutations in the APC gene. It is marked by the development of hundreds to thousands of adenomatous colon polyps, typically beginning in adolescence.
- Cancer Risks: Without surgical intervention, FAP carries a nearly 100% risk of colorectal cancer by age 40. There are also elevated risks for duodenal, gastric, thyroid (especially papillary), brain (medulloblastoma), and desmoid tumors.
- Screening: Management includes frequent colonoscopies starting in adolescence and prophylactic colectomy to prevent colorectal cancer. Upper endoscopy is used to monitor for duodenal adenomas.
How to Manage Hereditary Cancer Risks
Regular screenings, risk-reducing surgeries, and lifestyle modifications are vital strategies to lower cancer risk in individuals with hereditary predispositions. Evidence shows that these measures can significantly improve outcomes. For example, women with BRCA mutations who undergo prophylactic mastectomy can reduce breast cancer risk by up to 90%, and regular colonoscopies in Lynch syndrome carriers can decrease colorectal cancer incidence by early detection and polyp removal (source).
Step-by-Step Guide to Genetic Testing
1. Preparation: Gather detailed personal and family medical history, including ages at diagnosis and types of cancers. Consult with a healthcare provider or genetic counselor to evaluate the need for testing.
2. Testing Process: A blood or saliva sample is collected. The lab analyzes for mutations in relevant genes (e.g., BRCA1/2, MLH1, APC).
3. Results Interpretation: Results are classified as positive (mutation detected), negative (no mutation), or variants of uncertain significance. A genetic counselor helps explain what the findings mean for cancer risk and management.
4. Follow-up: Based on results, personalized screening, risk-reducing options, and family testing recommendations are made. For positive results, cascade testing of relatives is advised.
You Can also Read Does Processed Meat Cause Cancer? Myths and Facts by OncoDaily

Can Lifestyle Choices Offset Genetic Cancer Risks?
Environmental and lifestyle factors such as smoking, diet, and exercise interact with genetic risk to influence cancer development. For example, exposures like tobacco smoke, air pollution, and processed foods can damage DNA or disrupt repair mechanisms, especially in individuals with genetic susceptibilities, thereby increasing cancer risk. Gene-environment interactions mean that people with certain genetic variants may be more vulnerable to carcinogens—such as those with specific CYP gene variants facing a two- to tenfold higher risk of tobacco-related cancers when exposed to smoke.
However, evidence shows that lifestyle changes—like adopting a healthy diet, regular physical activity, and avoiding harmful exposures—can mitigate risk even in those with genetic predispositions, with estimates suggesting up to 40% of cancers could be prevented through such modifications. This underscores the importance of combining genetic awareness with healthy behaviors to lower overall cancer risk.
Communicating Genetic Risks with Family
When discussing genetic risks with family members, it’s important to approach the conversation thoughtfully, considering each person’s readiness, communication preferences, and emotional response. Start with close relatives—parents, siblings, and children—who are most likely to share the genetic risk, then extend to second-degree relatives like aunts, uncles, and cousins if appropriate.
Choose the communication method that fits your family dynamic—whether that’s in person, by phone, email, or text. Before starting the conversation, gather your medical records, genetic test results, and family health history to provide clear, accurate information. Involving a genetic counselor can also be helpful; they can guide the discussion or even help draft a family letter explaining the implications of the findings.
Be mindful that family members may react differently. Some will want in-depth details, others may not. Respect privacy, timing, and emotional boundaries. Consider enlisting a trusted family member to help share the information or act as a family health historian.
To keep track of inherited risk, use tools like family health history charts, apps (e.g., My Family Health Portrait), or shared digital documents. Genetic counseling reports often include summaries that can be shared with relatives. Encourage cascade testing—where at-risk family members undergo genetic testing and screening—to help prevent or detect disease early.
By starting with close relatives, preparing factual information, and using supportive tools and expert guidance, families can foster understanding and proactive health decisions that may reduce hereditary cancer risk.
Emerging Research in Cancer Genetics
Next-generation sequencing and multigene panel testing have expanded the ability to detect pathogenic variants across numerous cancer predisposition genes, improving early diagnosis and personalized risk assessment. Notably, updated guidelines now recommend broader genetic testing criteria, such as for TP53 mutations linked to Li-Fraumeni syndrome, to better identify carriers who may benefit from intensive surveillance.
Breakthroughs in understanding the functional impact of inherited single nucleotide variants have mapped nearly 400 variants that regulate cancer-related genes and pathways, including DNA repair and immune response, suggesting new targets for prevention and treatment. These insights are expected to enhance genetic screening tools, allowing tailored interventions like lifestyle modifications, pharmacologic prevention, and precision screening.
Preventive measures remain critical: individuals with hereditary risk benefit from regular screenings (e.g., earlier and more frequent colonoscopies for Lynch syndrome, breast MRI for BRCA carriers), risk-reducing surgeries, and lifestyle changes. Emerging targeted therapies, such as PARP inhibitors for BRCA-mutated cancers and immunotherapies for mismatch repair-deficient tumors, are transforming treatment paradigms.
In summary, recent genetic discoveries and improved testing technologies are revolutionizing hereditary cancer management by enabling earlier detection, personalized prevention, and novel therapeutics, ultimately aiming to reduce cancer incidence and improve survival.
You Can Also Read Does Vaping Cause Lung Cancer? Myths and Facts by Oncodaily

How Can You Understand Your Genetic Risk and What Are the Next Steps?
Understanding hereditary cancer risks empowers you to take control of your health. While genetics can increase cancer susceptibility, most cancers result from a combination of inherited mutations, lifestyle, and environmental factors. Regular screenings, healthy lifestyle choices, and, when appropriate, genetic testing and counseling are essential tools to manage and reduce your risk.
If you have a family history of cancer or concerns about inherited risks, consulting a healthcare provider or genetic counselor can provide personalized guidance tailored to your situation. They can help interpret genetic testing results, recommend appropriate surveillance, and discuss preventive options.
Remember, knowledge is power. Taking proactive steps today can lead to earlier detection, better outcomes, and peace of mind for you and your family.
Take Action Now
Reach out to a genetic counselor or healthcare professional to learn more about your risk and available resources. Empower yourself with information and support—your health is worth it.
Written by Aharon Tsaturyan MD
FAQ
What is hereditary cancer and how common is it?
Hereditary cancers are caused by inherited gene mutations that increase cancer risk. About 5–10% of all cancers are hereditary, with some types like breast, ovarian, and colorectal cancers more commonly linked to inherited mutations.
Who should consider genetic testing for hereditary cancer risk?
Testing is recommended for individuals with a strong family history of cancer, early-onset cancers, multiple affected relatives, rare cancers, or certain ethnic backgrounds linked to higher mutation prevalence.
What happens during genetic counseling and testing?
Genetic counseling includes evaluating family history, discussing testing options, and interpreting results. Testing involves analyzing blood or saliva for inherited mutations. Counseling helps understand implications and guides personalized prevention or treatment.
Does a negative genetic test mean I have no cancer risk?
No. A negative test means no known inherited mutation was found, but it does not eliminate cancer risk from sporadic mutations or lifestyle factors. Screening and healthy habits remain important.
What can I do if I have a genetic mutation linked to cancer?
Options include increased surveillance (e.g., earlier and more frequent screenings), risk-reducing surgeries, chemoprevention, and lifestyle changes. Genetic information can also influence treatment decisions if cancer develops.
Can hereditary cancer risk affect family members?
Yes. Inherited mutations can be passed to relatives, so sharing genetic information can help family members pursue testing and preventive care to reduce their risk.
Are there protections against genetic discrimination?
Most states have laws preventing health insurers from using genetic test results to deny coverage or raise rates. Confidentiality measures are also in place to protect genetic information.
Is most cancer inherited or genetic?
No. Only about 5–10% of cancers are caused by inherited genetic mutations. The majority of cancers result from acquired mutations due to aging, environmental exposures (like smoking or UV radiation), and lifestyle factors. Family history can increase risk but is not the sole factor (sources).
If no one in my family has cancer, am I not at risk?
Not necessarily. Many cancers arise sporadically without a family history. Environmental and lifestyle factors can cause mutations leading to cancer even in people without inherited risk. Therefore, absence of family cancer does not guarantee zero risk (sources).
If I have a genetic mutation like BRCA1 or BRCA2, will I definitely get cancer?
No. Having a mutation increases your lifetime risk but does not guarantee cancer development. Penetrance varies, and lifestyle, environment, and medical management influence outcomes. Many mutation carriers never develop cancer, especially with proper surveillance and preventive measures
-
Challenging the Status Quo in Colorectal Cancer 2024
December 6-8, 2024
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023
