What Is Intensity-Modulated Radiation Therapy (IMRT) and How It Works? Pros and Cons
Intensity-modulated radiation therapy (IMRT) is an advanced radiation therapy that precisely targets tumors, minimizing damage to healthy tissue. It’s significant in modern cancer treatment due to its ability to deliver higher doses of radiation to tumors while reducing side effects. Pros include improved tumor control and reduced toxicity; cons include increased planning time and potential for increased low-dose radiation to a larger volume of healthy tissue.
What is IMRT?
Intensity-modulated radiation therapy (IMRT) is a sophisticated and precise form of radiation therapy that represents a significant advancement in cancer treatment. It builds upon the principles of conformal radiation therapy by not only shaping the radiation beams to match the tumor’s three-dimensional shape, but also by modulating, or varying, the intensity of those beams. This allows for the delivery of highly targeted radiation doses, maximizing the dose to the tumor while minimizing the radiation exposure to surrounding healthy tissues and organs.
IMRT utilizes advanced computer technology and detailed imaging techniques, such as 3D CT scans, to create a comprehensive treatment plan. This plan meticulously maps the tumor’s location, size, and shape, allowing radiation oncologists to design radiation beams that precisely conform to the tumor’s contours. The intensity of each beam is then carefully adjusted, enabling the delivery of higher doses to areas within the tumor that require more aggressive treatment, while simultaneously reducing the dose to nearby critical structures.
The process involves the use of specialized equipment, such as multi-leaf collimators (MLCs), which are composed of movable leaves that can shape the radiation beams with exceptional accuracy. These leaves move independently, creating complex radiation patterns that precisely target the tumor while sparing healthy tissue. This precise control over the radiation dose and distribution allows for improved tumor control and reduced side effects, making IMRT a valuable tool in the treatment of various cancers.
How Does IMRT Work?
IMRT works by using a machine called a linear accelerator (LINAC) that has a device called a multileaf collimator. This collimator is made up of thin leaves that can move independently to form shapes that precisely fit around the treatment area. These leaves can move while the machine moves around the patient, shaping the beam of radiation to the tumor. This allows the tumor to receive a very high dose while normal healthy cells nearby receive a much lower dose.
Each radiotherapy beam is divided into many small beamlets, which can vary the intensity of radiation, giving different doses of radiation across the tumor. Planning IMRT involves imaging tests like CT scans, and sometimes MRI or PET scans, which provide information that feeds directly into the radiotherapy planning computer. The treatment team then plans the treatment using the scan images and advanced computerized calculations to find the dose strength pattern that best matches the tumor shape.
source: www.biomedcentral.com
Treatment Planning
In IMRT treatment planning, imaging plays a crucial role in mapping the tumor and surrounding tissues. CT scans are the standard imaging modality for radiotherapy planning, providing geometrically accurate information and electron density data necessary for planning algorithms. MRI is also increasingly used, especially for tumors in areas like the pelvis, head and neck, and brain, as it offers excellent soft tissue contrast. PET, SPECT, and MRI are functional imaging techniques that can provide valuable information about tumor physiology.
These different imaging modalities can be used together through image fusion to aid tumor localization. The information from these scans feeds directly into the radiotherapy planning computer. The treatment team then carefully plans the treatment using the scan images. They use advanced computerized calculations to find the dose strength pattern that best matches the tumor shape. This allows for customized treatment plans for each patient, tailored to the specific characteristics of their tumor and its location relative to surrounding healthy tissues.
Treatment Delivery
During IMRT treatment delivery, the patient is positioned on a treatment table, and immobilization devices such as masks or molds may be used to ensure the treatment area remains completely still. These devices help maintain proper position and improve the accuracy of the treatment.
IMRT often requires multiple treatment sessions. Typically, patients are scheduled for IMRT sessions five days a week for several weeks. The total number of treatments depends on factors like the type of cancer, tumor size, and location. Most treatment sessions take between 10 and 30 minutes, although some sources indicate they can range from 15 minutes to one hour.
What Are the Main Types of IMRT?
The main types of IMRT treatment delivery techniques are segmental MLC, dynamic MLC, tomotherapy, and Volumetric Modulated Arc Therapy (VMAT). Segmental MLC, or step-and-shoot IMRT, uses several different MLC-shaped fields, or segments, for each beam orientation, and the radiation is only turned on when the segments are in position. Dynamic MLC-IMRT involves continuous motion of the MLC leaves during treatment of each field, where the leaves are swept across the target volume to produce the desired radiation intensity. Tomotherapy delivers IMRT with a fan beam, similar to CT scanning, and a helical tomographic system has also been developed.
Multileaf Collimator (MLC) IMRT
Multileaf collimator (MLC) IMRT uses a linear accelerator equipped with a multileaf collimator to shape and modulate radiation beams, delivering radiation through multiple fixed beams, typically up to 25. This technique provides precise control over radiation dose distribution by adjusting the position of the leaves during treatment.
Volumetric Modulated Arc Therapy (VMAT)
Volumetric Modulated Arc Therapy (VMAT), also known as Rapid Arc, involves the linear accelerator rotating around the patient in an arc shape, continuously reshaping and changing the intensity of the radiation beam as it moves. VMAT is known for its accuracy, shorter treatment times, and lower overall radiation doses.
TomoTherapy (Serial Tomotherapy)
TomoTherapy uses a donut-shaped machine that rotates around the patient in a spiral pattern, enabling precise delivery of radiation beams from multiple angles, enhancing tumor targeting while sparing healthy tissues.
What Are the Potential Side Effects of IMRT?
IMRT, while designed to minimize damage to healthy tissues, can still result in a range of potential side effects. The specific side effects experienced depend largely on the area of the body being treated and the amount of radiation administered. Common short-term side effects include skin irritation or redness in the treated area, fatigue, and hair loss at the treatment site, which can sometimes be permanent. If the head and neck region is treated, patients may experience dry mouth, thickened saliva, difficulty swallowing, a sore throat, changes in taste, and mouth sores. Abdominal treatments can lead to nausea, vomiting, and diarrhea, while pelvic treatments may cause diarrhea, bladder irritation, frequent urination, and changes in sexual function.
Although IMRT significantly reduces the risk of long-term side effects compared to traditional radiation therapy, there is still a potential for late effects. These can include the development of secondary cancers years or even decades after treatment, though this is a very rare occurrence. It’s important to note that while IMRT’s precision helps to spare healthy tissue, some degree of radiation exposure to surrounding areas is unavoidable, which can lead to these potential side effects. However, the advanced technology and precise targeting of IMRT aim to significantly reduce the severity and frequency of these side effects compared to older radiation techniques.
Wortel et al. (Int J Radiat Oncol Biol Phys, 2016) found that image-guided IMRT (IG-IMRT) significantly reduced late grade ≥2 gastrointestinal (GI) toxicity compared to 3D-CRT in prostate cancer patients (24.9% vs. 37.6%, HR 0.59, P=.005), particularly proctitis and increased stool frequency. Genitourinary (GU) toxicity was comparable between the two. The study suggests IG-IMRT is the preferred treatment due to reduced GI complications.
Short-Term Side Effects
Short-term side effects from IMRT vary depending on the treatment area. Common effects include skin irritation or redness at the treatment site, fatigue, and hair loss in the treated area. Head and neck treatments may cause dry mouth, thickened saliva, trouble swallowing, sore throat, changes in taste, and mouth sores. Abdominal treatments can lead to nausea, vomiting, and diarrhea, while pelvic treatments may cause diarrhea, bladder irritation, frequent urination, and changes in sexual function. Management strategies include using gentle skin care products, staying hydrated, eating soft foods, and taking medications for nausea or diarrhea. Healthcare professionals can provide supportive care to manage these side effects during and after treatment.
Freedman et al. (Am J Clin Oncol, 2006) reported that IMRT in breast cancer patients significantly reduced the severity of acute skin desquamation compared to conventional radiation therapy. Specifically, 42% of IMRT patients experienced no desquamation, 37% dry desquamation, and 21% moist desquamation, compared to 52% grade 0, 10% grade 1, and 38% grade 2 desquamation in conventional patients (P = 0.001). For large breast sizes, moist desquamation grade 2 was 48% with IMRT versus 79% in controls. The study concluded IMRT reduces acute desquamation severity, though breast size remains a significant factor.
Long-Term Side Effects
Long-term side effects from IMRT are rare but can occur months or years after treatment. These late effects may include brain changes, spinal cord changes, lung changes, kidney changes, colon and rectal changes, infertility, joint changes, lymphedema, mouth changes, and secondary cancers. The prevalence of these effects is low, and they are often permanent. Monitoring these risks involves regular check-ups with the radiation oncologist to detect any potential complications early. Mitigating these risks involves utilizing techniques like IMRT to minimize radiation exposure to healthy tissues during treatment.
Read OncoDaily’s Special Article About Radiotherapy Side Effects
Pros and Cons of IMRT
IMRT offers the advantage of highly accurate radiation delivery, targeting tumors precisely and avoiding more invasive procedures. This precision translates to fewer side effects compared to traditional radiotherapy. However, IMRT can be more costly and, despite its precision, still poses a risk of side effects and some radiation exposure to healthy tissues. IMRT is often preferred for tumors located near critical organs, such as those in the head and neck, where minimizing damage to surrounding tissues is essential. For instance, in prostate cancer, IMRT reduces rectal and bladder complications, making it a better option than older radiation techniques.
Which Cancers Are Treated with IMRT?
IMRT is a common cancer treatment, particularly effective for prostate, head and neck, brain, and breast cancers. Its precision allows for high-dose radiation to tumors while minimizing damage to nearby sensitive organs. This is crucial for prostate cancer (protecting rectum/bladder), head and neck cancers (protecting salivary glands/spinal cord), brain tumors (protecting neurological structures), and breast cancer (minimizing heart/lung exposure). This precise delivery improves outcomes and reduces side effects.
How to Prepare for IMRT Treatment?
Preparing for IMRT treatment involves several key steps. Patients typically begin with consultations and evaluations to determine if IMRT is the appropriate treatment. Simulation sessions are crucial for planning, where imaging tests like CT scans are used to map the tumor and surrounding tissues. Immobilization devices, such as masks or molds, may be used to ensure the patient remains in the correct position during treatment. Patients can expect skin markings or tattoos to be placed to guide the radiation delivery. It’s important to discuss potential side effects with the healthcare team and understand the treatment schedule. Staying hydrated and maintaining a healthy diet can also aid in preparing for and managing the treatment process.
What to Expect During IMRT Sessions?
During an IMRT session, patients are carefully positioned on a treatment table, sometimes with the aid of immobilization devices to ensure they remain still. The radiation therapy team, including radiation therapists, monitors the patient from a separate room, observing them via closed-circuit television and maintaining communication through an intercom. The linear accelerator, the machine delivering the radiation, moves around the patient, emitting radiation beams that are shaped and modulated to target the tumor. Patients typically do not feel the radiation itself, but they may hear clicking or whirring noises from the machine as it operates. The process is generally painless, though some patients may experience discomfort from the positioning required for treatment.
Innovations in Intensity-Modulated Radiation Therapy
Advancements in IMRT are continually enhancing its precision and safety. Improved imaging techniques, such as cone-beam CT integrated with linear accelerators, allow for real-time adjustments during treatment, ensuring accurate targeting. Sophisticated computer programs and AI integration aid in optimizing treatment plans and dose calculations, leading to more personalized and effective therapies. New radiation delivery methods, like Volumetric Modulated Arc Therapy (VMAT), shorten treatment times and reduce radiation exposure to healthy tissues. These innovations collectively improve tumor control and minimize side effects, making IMRT an increasingly powerful tool in cancer treatment.
AI and Machine Learning in IMRT Planning
AI and machine learning are revolutionizing IMRT planning by using algorithms to refine the allocation of radiation dosages. These intelligent systems analyze complex imaging data and treatment parameters to determine the most effective radiation distribution, significantly shortening the planning phase and boosting the accuracy of tumor targeting. This leads to more tailored treatment plans that enhance tumor control while minimizing harm to healthy tissues.
Sheng et al. (J Appl Clin Med Phys, 2025) developed an in-house AI platform for head-and-neck IMRT planning, reducing average plan generation time to 10-15 minutes, with AI predictions taking approximately 1 second. The platform offered six AI models providing various trade-offs between parotid sparing and PTV-OAR preferences, demonstrating robust performance and validation compared to clinical plans.
Adaptive IMRT: Real-Time Treatment Adjustments
Adaptive radiation therapy (ART) allows for real-time adjustments to radiation plans by monitoring changes in the tumor’s size, shape, and position during the course of treatment. This approach enables clinicians to modify the radiation dose distribution based on the tumor’s response, ensuring that the treatment remains optimally targeted. This is particularly beneficial for tumors that change rapidly, as it allows for a more dynamic and personalized treatment strategy, ultimately enhancing patient outcomes.
Tsuji et al. (Int J Radiat Oncol Biol Phys, 2010) evaluated automatic contour deformation for adaptive head-and-neck cancer IMRT planning. Automatic plans showed significantly lower mean coverage for GTV (V95: 89.9% vs. 98.6%, p=0.004) and CTV (V95: 89.8% vs. 98.4%, p<0.001), and a higher mean maximum dose to 1 cm³ of the spinal cord (42.8 Gy vs. 39.9 Gy, p=0.034) compared to manual plans. While automatic normal structure contours were dosimetrically acceptable, GTV segmentation was not robust enough to replace physician-drawn volumes.
Proton Therapy vs. IMRT: A Hybrid Approach
A combined approach using proton therapy and IMRT is emerging, particularly for delicate treatment areas. Proton beams, known for their ability to deposit radiation precisely, are used for highly sensitive regions to minimize radiation exposure to surrounding healthy tissues, while IMRT is employed for other areas. This hybrid strategy is gaining traction in treating pediatric cancers and brain tumors, where protecting developing tissues and critical neurological structures is paramount. By leveraging the strengths of both proton therapy and IMRT, clinicians can achieve greater precision and reduce the risk of long-term side effects in these vulnerable patient populations.
Duts et al. (Acta Oncol, 2018) compared PBT and IMRT for prostate cancer, finding no significant differences in GI and GU toxicities, except for lower late urinary urgency with PBT (0% vs. 25%, p=.047). Late GU toxicities correlated with bladder dose-volume parameters. QoL was similar between groups, with slight advantages for IMRT in late global health status and PBT in early constipation. Overall, both treatments were well-tolerated.

Read OncoDaily’s special article about Proton therapy.
FLASH Radiotherapy: Ultra-Fast Radiation Delivery
FLASH radiotherapy delivers ultra-high dose radiation in fractions of a second, potentially minimizing healthy tissue damage (“FLASH effect”) while targeting cancer. Preclinical research is promising, showing reduced toxicity and improved tumor control, though clinical use is early. Scientists are working to understand the “FLASH effect” and overcome technological hurdles. FLASH radiotherapy holds promise for more effective, less toxic cancer treatment.
How Much Does IMRT Cost?
The expense of IMRT varies based on several factors. The type of malignancy being treated, the length of the treatment period, and the location of the medical facility all contribute to the overall cost. Due to the advanced technology and detailed planning involved, IMRT often has a higher price tag compared to traditional radiation therapies.
Carter et al. (Radiotherapy and Oncology, 2014) estimated that IMRT, post-radical prostatectomy, was more effective and less costly than 3DCRT over 20 years, with 20 additional QALYs ( Quality-Adjusted Life Year) gained and over $1.1 million saved per 1000 patients. The study concluded IMRT has a modest long-term advantage, providing quantitative guidance on its cost-effectiveness.
Recovery of the Body After IMRT
Recovery following IMRT varies, with physical recovery timelines dependent on the specific cancer and treatment intensity. Residual side effects, such as fatigue and skin sensitivity, can be managed with supportive care, including gentle skin products and rest. Long-term monitoring is essential to detect any potential late effects like xerostomia and taste dysfunction after head and neck irradiation. Lifestyle adjustments, such as maintaining a balanced diet, engaging in appropriate exercise, and managing stress, can significantly aid in the recovery process.
Chen et al. (2022) in JAMA Otolaryngology – Head & Neck Surgery found that most head and neck cancer patients experienced taste dysfunction (TD) during (91.9%) and 3 months after (33.3%) IMRT. Long-term TD was less common. Higher oral cavity radiation dose was associated with TD at 3 months post-IMRT, suggesting dose reduction could improve early taste recovery.
Written by Aren Karapetyan, MD
FAQ
How does IMRT compare to traditional 3D conformal radiation therapy?
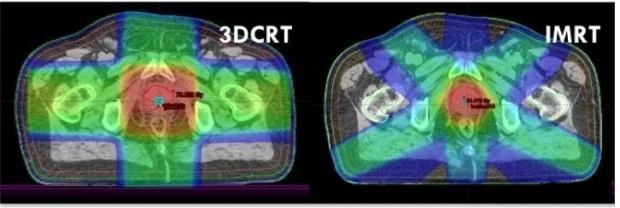
IMRT provides greater precision than 3D conformal radiation therapy by modulating beam intensity. This allows for higher radiation doses to the tumor while minimizing exposure to surrounding healthy tissues. In contrast, 3D conformal therapy delivers uniform radiation, potentially increasing side effects.
Can IMRT be used for recurrent cancers after previous radiation treatments?
Yes, IMRT is often used for re-irradiation when cancer recurs after previous radiation. Its highly targeted approach reduces risks to already irradiated tissues, making it a safer option. Feasibility depends on prior radiation doses, tumor location, and patient health.
Does IMRT require a longer treatment time than other types of radiation therapy?
IMRT sessions typically last longer than standard radiation therapy due to complex planning and beam modulation. While conventional treatments take 10-15 minutes, IMRT can take 30-60 minutes per session, depending on tumor size and location.
Is IMRT effective for treating moving tumors, such as those in the lungs?
IMRT is effective for many tumors, but for moving tumors (e.g., lung, liver), image-guided radiation therapy (IGRT) or respiratory gating may be combined with IMRT. These techniques track tumor movement in real-time, ensuring better accuracy and reduced healthy tissue exposure.
How soon after IMRT can I return to normal activities?
Recovery varies, but many patients resume normal activities shortly after treatment ends, depending on side effects.
Is IMRT a painful procedure?
No, IMRT itself is painless; patients may experience discomfort from positioning or side effects
Can IMRT be used to treat multiple tumors at once?
Yes, IMRT can treat multiple tumors, but planning complexity increases.
What imaging is used for IMRT planning?
CT scans are standard, with MRI and PET scans used to provide additional details.
How often are IMRT treatments given?
Typically, five days a week for several weeks.
What is VMAT?
Volumetric Modulated Arc Therapy, a type of IMRT, where the linear accelerator rotates around the patient.
-
Challenging the Status Quo in Colorectal Cancer 2024
December 6-8, 2024
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023
