New Advisory Urges Public Action and Enhanced Awareness on Alcohol Consumption
A Surgeon General’s Advisory serves as a critical public statement aimed at raising awareness about urgent public health issues and providing actionable recommendations. This particular advisory focuses on the significant relationship between alcohol consumption and cancer risk, emphasizing the need for immediate national attention and action.
“Alcohol is a well-established, preventable cause of cancer responsible for about 100,000 cases of cancer and 20,000 cancer deaths annually in the United States – greater than the 13,500 alcohol-associated traffic crash fatalities per year in the U.S. – yet the majority of Americans are unaware of this risk. This Advisory lays out steps we can all take to increase awareness of alcohol’s cancer risk and minimize harm.” – said U.S. Surgeon General Dr. Vivek Murthy.

The advisory highlights that alcohol consumption is a major preventable cause of cancer in the United States, contributing to nearly 100,000 new cancer cases and approximately 20,000 cancer-related deaths each year. Despite the prevalence of alcohol use – 72% of U.S. adults reported consuming alcohol weekly – less than half are aware of its link to cancer risk.
Alcohol as a Leading Cause of Cancer in US
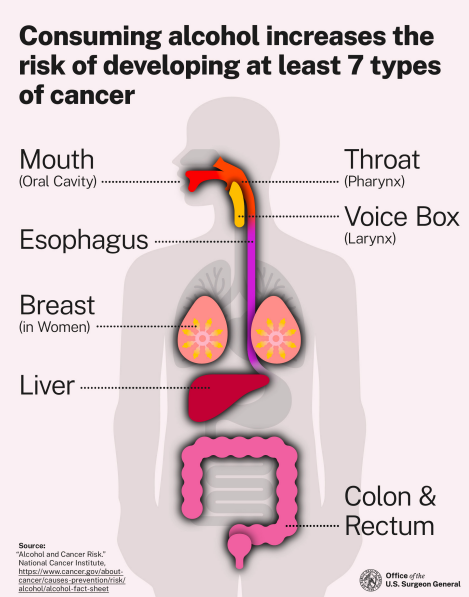
In 2019, an estimated 96,730 cancer cases in the United States were attributed to alcohol consumption, with 42,400 cases in men and 54,330 in women. This statistic translates to nearly 1 million preventable cancer cases over a ten-year period. The burden of alcohol-related cancer is particularly pronounced for breast cancer among women, which accounted for approximately 44,180 cases in 2019.
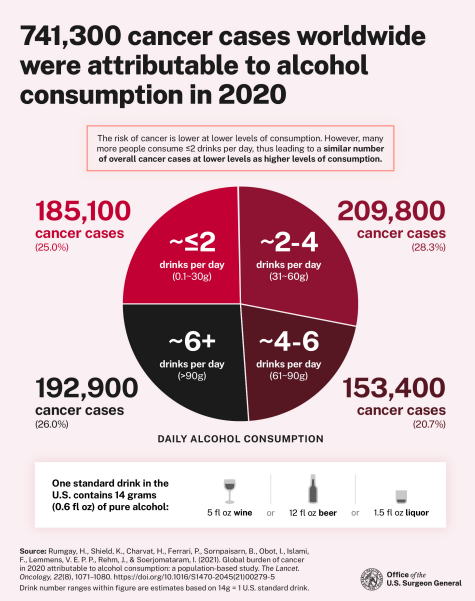
This figure represents 16.4% of the total breast cancer cases reported for women that year.Globally, the impact of alcohol on cancer incidence is also significant. In 2020, there were 741,300 cancer cases related to alcohol consumption worldwide, with 185,100 cases linked to the consumption of about two drinks daily or fewer. These statistics underscore the urgent need to address alcohol consumption as a critical public health issue.
Alcohol-Related Cancer Deaths
In the U.S., there are about 20,000 alcohol-related cancer deaths annually, a figure that exceeds the approximately 13,500 fatalities from alcohol-associated traffic crashes each year. The average life expectancy of those who die from alcohol-related cancers is shortened by about 15 years, resulting in a total loss of approximately 305,000 years of potential life annually due to these deaths.
Breast cancer accounts for around 60% of alcohol-related cancer deaths in women, while liver cancer (approximately 33%) and colorectal cancer (an additional 21%) account for the majority of such deaths in men. Notably, about 83% of the estimated 20,000 U.S. alcohol-related cancer deaths occur at levels exceeding the 2020-2025 U.S. Dietary Guidelines for Americans’ recommended limits—two drinks daily for men and one drink daily for women. Alarmingly, the remaining 17% occur even within these recommended limits.
Public Awareness and Understanding
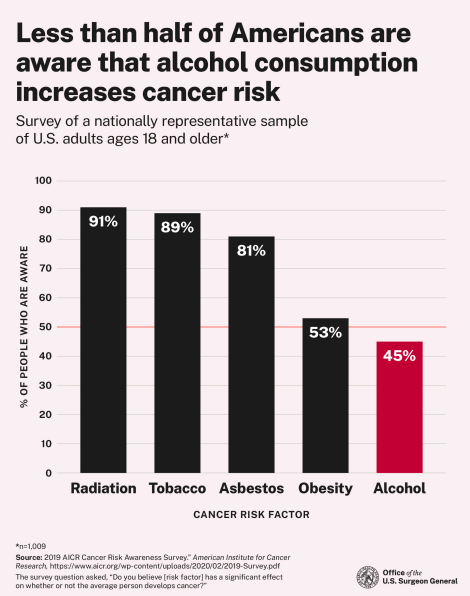
Despite clear evidence linking alcohol consumption to cancer risk, public understanding remains inadequate. A 2019 survey indicated that only 45% of Americans recognized alcohol use as a risk factor for cancer. In comparison, recognition rates for other known carcinogens are significantly higher: 91% for radiation exposure, 89% for tobacco use, and 81% for asbestos exposure. Furthermore, awareness of alcohol as a cancer risk factor has not improved substantially over nearly two decades, even as evidence of this link has grown stronger.
Establishing Causality: Evidence Summary
Determining whether a causal relationship exists between a risk factor (such as alcohol consumption) and a health outcome (like cancer) involves comprehensive assessments of scientific evidence using established criteria like the Bradford Hill criteria. This process includes evaluating observational studies where large cohorts are followed over time and reviewing animal studies alongside research into biological mechanisms leading to cancer.
Numerous high-quality observational studies and meta-analyses have consistently shown a significant relationship between alcohol consumption and increased cancer risk. For instance, a global meta-analysis involving data from 572 studies and over 486,538 cancer cases confirmed this association. Another pooled analysis indicated that individuals consuming about one drink daily had a 40% increased risk of mouth cancer compared to non-drinkers.
Additionally, research involving more than one million women found that consuming up to one drink daily was associated with a 10% increased risk of breast cancer.The International Agency for Research on Cancer (IARC) classifies alcohol as a Group 1 carcinogen—indicating sufficient evidence that it can cause cancer in humans—while the World Cancer Research Fund/American Institute for Cancer Research ranks the evidence linking alcohol and cancer as “Convincing: Increases Risk.”
How Alcohol Causes Cancer?
Extensive biological studies have identified several mechanisms through which ethanol (the type of pure alcohol found in alcoholic beverages) contributes to cancer development:
1. Acetaldehyde Production: Alcohol is metabolized into acetaldehyde in the body—a compound that binds to DNA and causes damage. This DNA damage can lead to uncontrolled cell growth and tumor formation.
2. Reactive Oxygen Species: Alcohol consumption generates reactive oxygen species that increase inflammation and can damage DNA, proteins, and lipids through oxidation.
3. Hormonal Changes: Alcohol alters hormone levels (including estrogen), which may play a significant role in breast cancer development.
4. Carcinogen Solvent Effect: Alcohol can dissolve carcinogens from other sources (e.g., tobacco smoke), facilitating their absorption into the body and increasing risks for cancers of the mouth and throat.
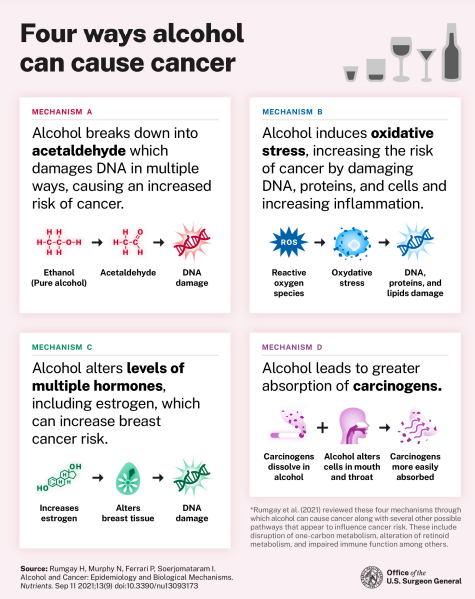
The first two pathways – acetaldehyde production and inflammation – are particularly well-established as key contributors to carcinogenesis.
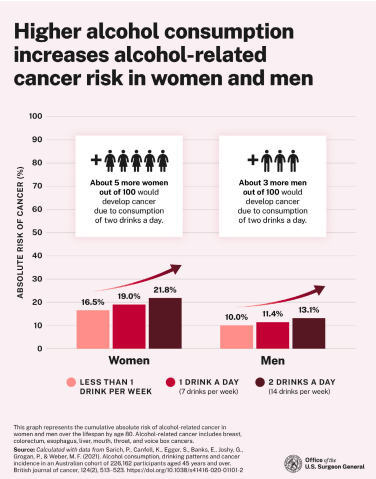
The amount of alcohol consumed significantly influences individual cancer risk. Evidence suggests that risk increases with higher levels of consumption; however, even low levels may elevate risk for specific cancers such as breast and throat cancers.
Understanding Risk: Absolute vs. Relative
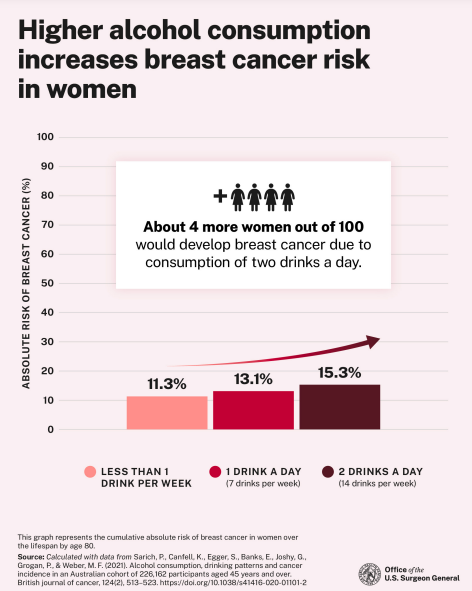
- Absolute Risk: This refers to the actual probability of developing an outcome (e.g., a new cancer diagnosis). For instance, among women consuming less than one drink per week, the absolute risk of developing any alcohol-related cancer over their lifetime is approximately 16.5%, compared to 19.0% for those consuming one drink daily and around 21.8% for those consuming two drinks daily.
- Relative Risk: This compares the probability of an outcome occurring between different groups (e.g., drinkers vs. non-drinkers). For example, women who consume up to one drink per day experience a 10% relative increase in breast cancer risk compared to non-drinkers; this rises to a 32% relative increase for those consuming more than two drinks daily.
Long-term cessation or reduction in drinking has been associated with decreased risks for certain cancers like mouth and esophageal cancers.
Recommendations for Reducing Alcohol-Related Cancer Risks
To mitigate the impact of alcohol on public health regarding cancer risks, several key actions are recommended:
1. Update Health Warning Labels: Revise existing Surgeon General’s health warning labels on alcoholic beverages to include warnings about the risk of cancer associated with consumption.
2. Reassess Recommended Limits: Reevaluate current guidelines on alcohol consumption based on emerging evidence linking it to increased cancer risk.
3. Enhance Education Efforts: Strengthen educational initiatives aimed at raising awareness about alcohol as a leading modifiable risk factor for cancer.
4. Clinical Awareness: Inform patients about the link between alcohol consumption and increased cancer risk during clinical visits; promote screening and brief interventions when necessary.
5. Incorporate Reduction Strategies: Highlight proven strategies for reducing alcohol consumption within population-level cancer prevention initiatives.
6. Individual Awareness: Encourage individuals to consider their drinking habits in light of their potential impact on cancer risk.
The link between alcohol consumption and increased cancer risk is well-established through extensive research across multiple domains. Despite this knowledge, public awareness remains low, highlighting an urgent need for educational initiatives and policy changes aimed at reducing alcohol-related cancers in the U.S. By implementing recommended strategies and fostering greater understanding among individuals regarding their drinking habits, we can work towards decreasing the incidence of preventable cancers linked to alcohol use.
Individuals have shared this advisory, adding their thoughts and reflections:
“NEW: Today, I’m releasing a Surgeon General’s Advisory on the causal link between alcohol consumption and increased cancer risk. Alcohol is the 3rd leading preventable cause of cancer in the U.S., contributing to about 100,000 cancer cases and 20,000 cancer deaths each year.”
“Today, Dr. Vivek Murthy released a Surgeon General’s Advisory on the causal link between alcohol consumption and increased cancer risk. With about 20,000 alcohol-related cancer deaths per year in the U.S., we must increase awareness of the risks of alcohol consumption. Read more.”
“While I am encouraged seeing this in hard print, especially when I am regularly asked about alcohol by the patient facing groups that I lead, when did we start treating alcohol and cancer as “new news”?
I have immense respect for our Surgeon General Vivek Murthy—a incredible, thought and visionary leader who elevates critical health topics like mental health, burnout, loneliness and isolation.
Yet, the media’s portrayal of alcohol’s risks as groundbreaking caught me off guard.
The link between alcohol and cancer risk is not new alart. Organizations like the American Institute for Cancer Research have long classified alcohol as carcinogen.
Researchers like Noelle K. LoConte, have even challenged the presence of alcohol at oncology events—a bold yet necessary stance. As Chair of the Cancer Member Interest Group for the American College of Lifestyle Medicine, I echo these concerns.
In our work, addressing risky behaviors like alcohol use is included as a pillar of Lifestyle Medicine. However, we’ve expanded the conversation to include sugar-sweetened beverages drinks, inactivity, and metabolic health risks- all within the context of risk reduction and survivorship.
Still, I find it ironic that, while our conferences are 100% plant-based even though that’s not our dietary position, alcohol is present. It raises an important question: Are our habits aligned with our message?
Personally, I don’t drink alcohol. I prioritize regular exercise, whole foods, and sustainable habits—but I’m far from perfect. My diet includes animal products within a minimally processed diet but that’s not 100% of the time. Does this make me a hypocrite or just human?
Here’s my takeaway: It’s not about perfection; it’s about accountability. We owe it to ourselves—and those we serve – to make informed choices, stay rooted in research, and acknowledge where we fall short without excuses. My role includes keeping my toe into clinical oncology, patient focused and organizational work. This requires me to consistently be focused on what research we have, or DON’t have.
What steps can we take – individually or as organizations – to better align our actions with the evidence that we are representing?”
“The Surgeon General has released a public health advisory emphasizing the connection between alcohol consumption and cancer. The advisory includes a call to action to update the existing warning label on alcohol-containing beverages which has not been revised since 1988.
From the oral cavity to the rectum, alcohol can contribute to cancer development in four key ways:
– Acetaldehyde decomposition
– Induction of oxidative stress
– Modifying estrogen and other hormone levels
– Enhancing the absorption of carcinogens
The report highlights that only 45% of Americans surveyed recognized the link between alcohol and cancer, whereas 91% were aware of radiation as a cancer-causing factor.”
“20.5% of Nebraska Adults report binge drinking (four or more [females] or five or more [males] drinks on one occasion in the past 30 days) or heavy drinking (eight or more [females] or 15 or more [males] drinks per week) according to America’s Health Ranking.
I know that this sparked conversation within my own friend group this weekend around reducing alcohol consumption. How can we support/create social interventions to help individuals drink less to support their health and reduce their cancer risk?
Potential Ideas floating through my mind:
1. Mocktail Recipes and low alcohol alternatives – I am thankful our rural grocery store carries NA Blue Moon (my favorite), it would be great for gas stations and stores to carry a variety of NA alternatives.
2. Tracking – I always to back to Marathon Kids and the intrinsic motivation model. A tracker that would allow individuals to keep track of the amount of alcohol consumed or sober days would allow for an better picture of their individual consumption.
3. Social Network – It is hard to be the only one not drinking. I think becoming a community champion or support in your community and friend group would be a powerful start in terms of reducing alcohol consumption.”
“The Advisory emphasizes that the risk of cancer increases with the amount of alcohol consumed. For certain cancers, such as those of the breast, mouth, and throat, evidence indicates that even consuming around one or fewer drinks per day can elevate risk. Let’s start with education and public awareness!”
“Of all the pillars of Lifestyle Medicine, reducing risky substances is an area where much progress can still be made. Living in an alcohol rich environment poses a challenge for many but it is encouraging to see all the progress towards reductions in use, including among young people!”