Ashish M. Kamat, Endowed Professor of Urologic Oncology (Surgery) and Cancer Research at University of Texas MD Anderson Cancer Center, shared his recent article on X:
Impact of fellowship training on pathologic outcomes and complication rates of radical prostatectomy
Authors: Charles J. Rosser, et al.
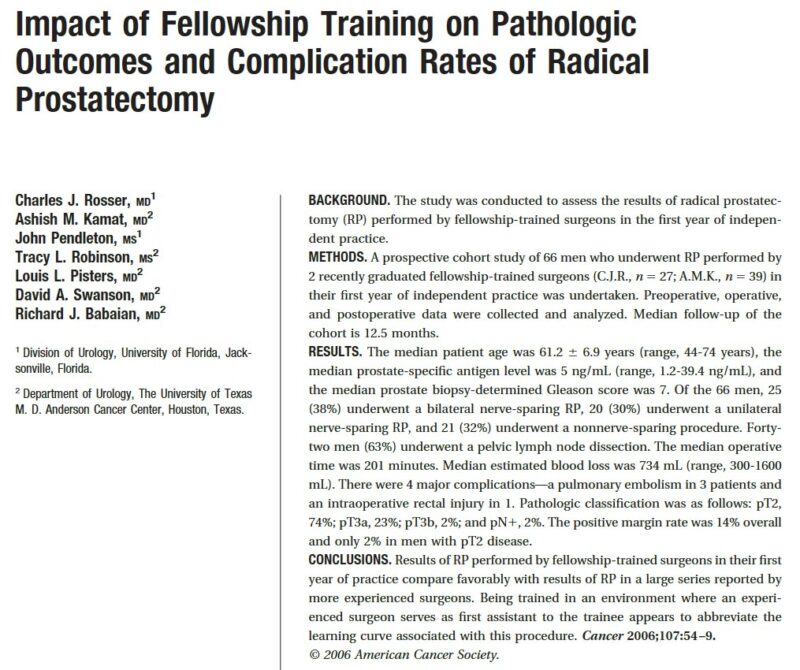
Summary of the Study:
Objective:
Assess outcomes of radical prostatectomy (RP) performed by fellowship-trained surgeons in their first year of independent practice.
Study Design:
Prospective cohort study involving 66 men with localized prostate cancer.
Conducted by two recently graduated fellowship-trained surgeons (C.J.R. and A.M.K.) from September 2003 to August 2004.
Median follow-up period: 12.5 months.
Patient Demographics:
Median age: 61.2 years (range: 44–74 years).
Median prostate-specific antigen (PSA) level: 5 ng/mL (range: 1.2–39.4 ng/mL).
Median Gleason score: 7.
Surgical Approaches:
Bilateral nerve-sparing RP: 38% of patients.
Unilateral nerve-sparing RP: 30% of patients.
Non-nerve-sparing procedures: 32% of patients.
Pelvic lymph node dissection performed in 63% of cases.
Operative Metrics:
Median operative time: 201 minutes.
Median estimated blood loss: 734 mL (range: 300–1600 mL).
Complications:
Major complications included:
Three cases of pulmonary embolism.
One intraoperative rectal injury.
Pathological Outcomes:
Pathological classifications:
- pT2 (organ-confined): 74%.
- pT3a: 23%.
- pT3b (seminal vesicle invasion): 2%.
Positive margin rate: Overall 14%; only 2% in pT2 patients.
Conclusions:
Outcomes of RP by fellowship-trained surgeons are comparable to those achieved by more experienced surgeons.
Structured training in a supportive environment may reduce the learning curve for complex procedures like RP.
Significance:
Highlights the importance of fellowship training in improving surgical proficiency and patient outcomes in urologic oncology.
More posts featuring Ashish Kamat.