Cervical cancer treatment has progressed remarkably over the past two decades, largely due to innovations in radiation delivery techniques. Image-guided adaptive brachytherapy (IGABT), promoted through the work of the GEC-ESTRO GYN working group, has played a pivotal role in improving local control while minimizing treatment-related toxicity. Building on the clinical success of EMBRACE I and the retrospective RetroEMBRACE studies, which showed 3-year local control rates of 93–100% and morbidity rates under 6%, the EMBRACE II study was launched to further refine radiotherapy protocols for patients with locally advanced cervical cancer (LACC). Its goals include improving efficacy, standardizing modern radiation techniques across centers, and reducing acute and late toxicities.
Presented at ESTRO 2025 by Dr. Mayuri Charnalia, one of the notable contributions from the EMBRACE II trial focused on identifying risk factors for acute gastrointestinal (GI) toxicity during external beam radiotherapy (EBRT) and concurrent chemotherapy in LACC.
Although technological improvements such as IMRT and VMAT have allowed for more precise dose delivery, GI toxicity remains a frequent and limiting side effect. This substudy aimed to isolate patient- and treatment-related predictors to inform safer planning strategies.
Methods
This prospective, multicenter analysis was based on patients enrolled in EMBRACE II between 2016 and 2021. All participants underwent a modern, standardized treatment approach including:
- Image-guided IMRT or VMAT, with daily cone-beam CT image guidance
- MRI-guided adaptive brachytherapy (IC/IS)
- Concurrent chemotherapy, typically weekly cisplatin for up to 5 cycles
- Simultaneous integrated boost (SIB) to involved lymph nodes: 45 Gy in 25 fractions to the pelvis, with positive nodes boosted to 55–65 Gy EQD2₁₀
To assess early toxicity attributable to EBRT, physician-assessed acute GI symptoms were recorded using CTCAE v3 at the 4th week of treatment (RT4W). Toxicities included:
- Diarrhea (grade ≥2)
- Abdominal pain or cramping (grade ≥2)
- Proctitis (grade ≥2)
- Fecal urgency (inability to defer defecation >15 minutes)
Statistical analysis involved univariate and multivariable logistic regression to identify predictors of grade ≥2 GI toxicity. Continuous variables were assessed for correlation using Pearson coefficients, and backward stepwise regression was performed using the Akaike Information Criterion (AIC) for model optimization.
Study Design
Out of the full EMBRACE II cohort, 1,334 patients with complete GI toxicity data at RT4W were included in this analysis. Potential predictors were grouped as:
Patients- related factors: age, body mass index (BMI), smoking status, comorbidities, history of abdominal/pelvic surgery, and baseline GI symptoms
Treatment-related factors:
- Bowel V40Gy – volume of bowel receiving ≥40 Gy
- Body V50Gy – body volume receiving ≥50 Gy from nodal boosts
- Para-aortic nodal boosting
- Elective para-aortic irradiation
Because of moderate intercorrelation (Pearson r = 0.40), only the most predictive of these—body V50Gy—was retained in multivariable models to avoid redundancy.
Results
The incidence of moderate-to-severe GI toxicity by the fourth treatment week was substantial
- Diarrhea (G≥2): 16% (n = 212)
- Abdominal pain/cramping (G≥2): 6% (n = 85)
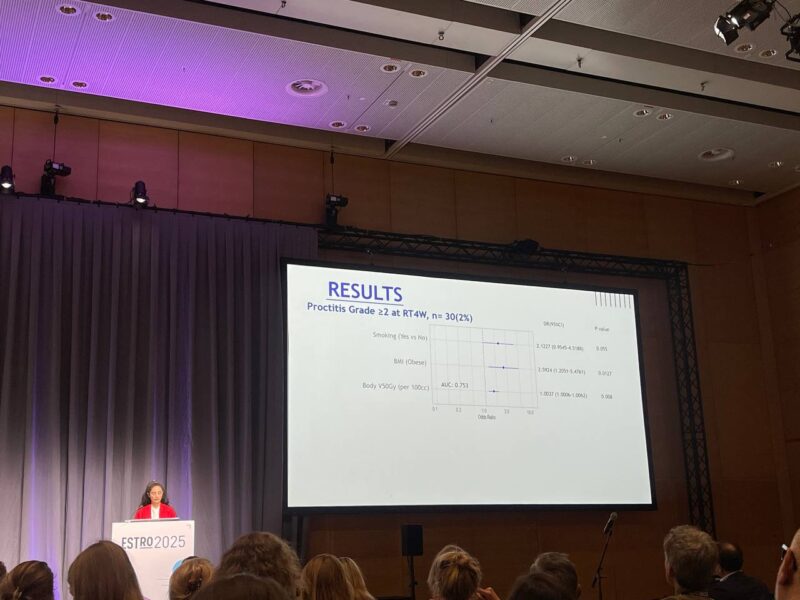
- Proctitis (G≥2): 2% (n = 30)
- Fecal urgency: 25% (n = 332)
Key predictors of GI toxicity included
- Body V50Gy was the strongest dosimetric predictor, significantly associated with both diarrhea and proctitis.
- Bowel V40Gy was also a significant factor, indicating that larger bowel volumes exposed to ≥40 Gy increase risk.
- Treatment strategies involving elective para-aortic irradiation and nodal boosting were correlated with higher body V50Gy and contributed to toxicity.
- In contrast, tumor stage was not predictive of acute GI toxicity, highlighting that radiation dose distribution outweighs tumor burden as a driver of side effects.
Key Takeaway Messages
• Bowel V50Gy is better associated with acute GI toxicity compared to V40Gy and V15Gy
• Larger target volume and nodal boost is associated with higher risk of acute diarrhea and proctitis
• Para-aortic irradiation is associated with greater risk of acute abdominal pain compared to without
• Elective elective para-aortic irradiation is associated with risk of acute fecal urgency
• Baseline GI symptoms and smoking, age, pre-existing comorbidities, previous pelvic/abdominal surgery indicate a high risk of acute GI toxicity
• Tumour tumour size was not associated with acute GI tox
Read ESTRO 2025 Updates on OncoDaily.