Mohammad Jad Moussa, Oncology Fellow at MD Anderson Cancer Center, posted on X about recent paper by him as first author, titled “Histopathologic Progression and Metastatic Relapse Outcomes in Small Cell Neuroendocrine Carcinomas of the Urinary Tract” published on Wiley.
Authors: Mohammad Jad Moussa, Georges C. Tabet, Arlene O. Siefker-Radtke, Lianchun Xiao, Nathaniel R. Wilson, Jianjun Gao, Christopher J. Logothetis, Petros Grivas, Byron Lee, Amishi Y. Shah, Pavlos Msaouel, Roger Li, Leticia Campos Clemente, Jianping Zhao, Nizar M. Tannir, Ashish M. Kamat, Donna E. Hansel, Charles C. Guo, Matthew T. Campbell, Omar Alhalabi
“OUR LATEST Original Research in Cancer Medicine on Small Cell Neuroendocrine Carcinoma of the Urinary Tract (SCNEC-URO) – What drives post-surgical relapse in this aggressive disease?
At GU24, we tackled how SCNEC-URO, with its reserved prognosis (vs. UC) and distinct histology often co-exisitng with UC, poses challenges in targeting the leading cellular component in progression and relapse. With a wealth of new therapies in the GU field (EV, TDXd, etc.), we need to investigate small cell biology for optimal trials.
Herein, we analyze an institutional definitive-surgery cohort (n = 224) of patients with cT1-T4NxM0 SCNEC-URO, referred to as ‘Cohort A’. Spanning from 1985 to 2021 – this represents one of the largest single-center series reported in the literature.
We aimed to:
- Characterize 1st sites of post-surgical relapse, distant vs. local (Cohort A)
- Assess prognostic impact of histology at resection & other clinical variables in relapse (Cohort A)
- Describe SCNEC histologies in mets. biopsies (Cohort B, exploratory)
We followed Cohort A: from diagnosis/TUR to neoCTx receipt status to surgical resection to post-surgical follow-up (metastatic relapse status).
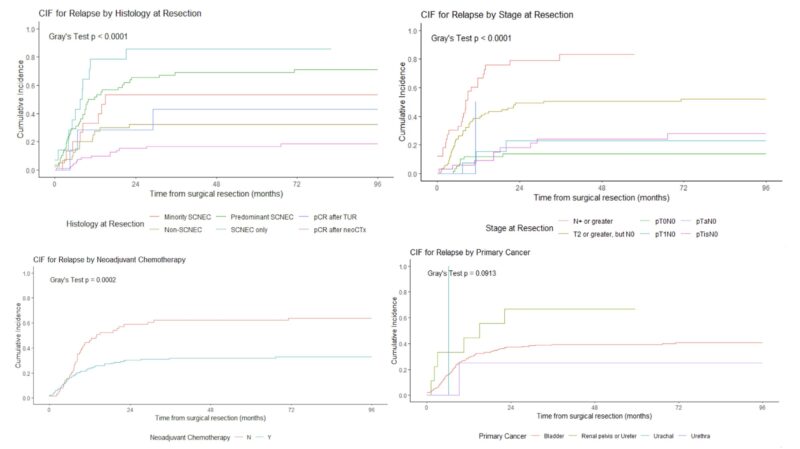
By correlating histological and clinical outcomes, we can understand how histology at resection (e.g., achieving pCR, remaining small cell disease, remaining non-small components, etc.) would affect relapse risk on the right.
Patients with pCR after neoCTx had the lowest 5-year CIF of 16.5% (Upper Left). CIF relapse rates gradually increased with the rising small cell contribution amount, ranging from 53.3% for minority SCNEC to 69% for predominant SCNEC, and 85.7% for pure remaining small cell disease.
An increasing relapse risk was also observed for path staging, as seen in the MSKCC series.
We now have our hypothesis that histology at resection impacts relapse risk. To explore this ‘holistically’ in our multivariable regression model (prognostic factors of post-surgical relapse), we designed this DAG to account for our ‘suspected’ confounders (red circles).
Our multivariable analysis adjusting for neoCTx, clinical stage at diagnosis (T3/4, N0/N+ vs. T1/T2, N0), and pathologic stage (pN+ vs. pN0) demonstrated that any SCNEC histology at resection (vs. pCR) was associated with relapse risk (HR = 3.69, p=0.0001).
Next question: What were the post-surgical relapse sites? Most documented sites of relapse were distant (71%), mostly liver, lung and bone, while a minority only had locoregional recurrence (13%). Limited efficacy of tailored control strategies like adjuvant radiation therapy in this disease setting?
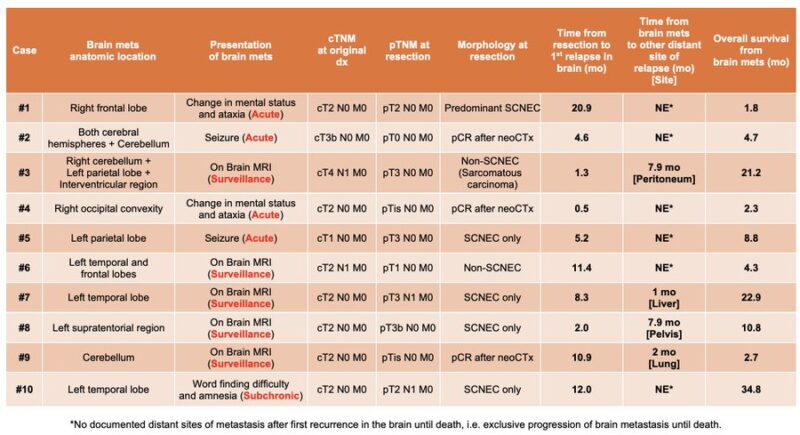
Most importantly, ~11% of pts had an EXCLUSIVE first release in the brain, without concomitant extracranial spread. Median relapse time from surgery 6.8 mo. 9/10 within 1 yr of surgery. Brain mets % notably >> than known incidence in UC (~1%). -> Baseline MRI of the brain NEEDED to rule out distant spread and surveillance brain imaging crucial every 3–4 months after surgery for the first 2 years!
We conclude with our Précis (Condensed Abstract) and Take Home Messages, accessible for all in the paper for our patient advocates and the public, highlighting the insights behind our findings.”
