Mark Lewis shared on X:
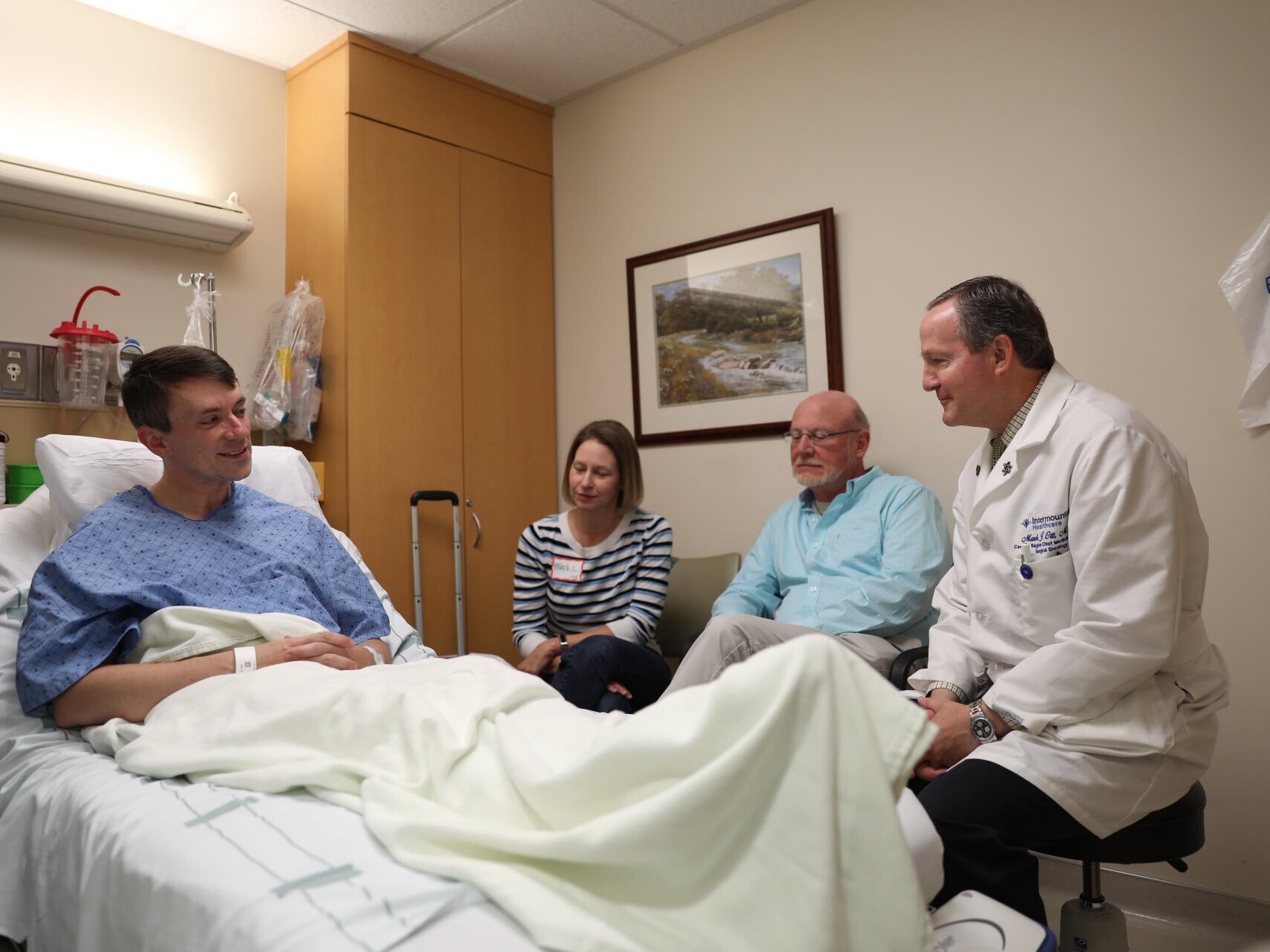
“7 years ago today these men saved my life.
Performing the Whipple procedure over a harrowing 6 1/2 hours they removed a tumor from the head of my pancreas and prevented it from metastasizing to my liver. I will be forever thankful.
And yet that gratitude is increasingly tinged by survivor’s guilt One perk of being a patient-physician is knowing which doctors you would — hypothetically or in actuality — entrust with your life But I realize my privilege extends far beyond cherry-picking the best surgeons.
As a GI (Gastrointestinal) oncologist a huge part of my practice is devoted to pancreatic cancer. There, I see patients with both adenocarcinoma and neuroendocrine tumors (mine was the latter). But of the former about 80% are inoperable when we meet and many of those will never make it to the OR (Operating Room).
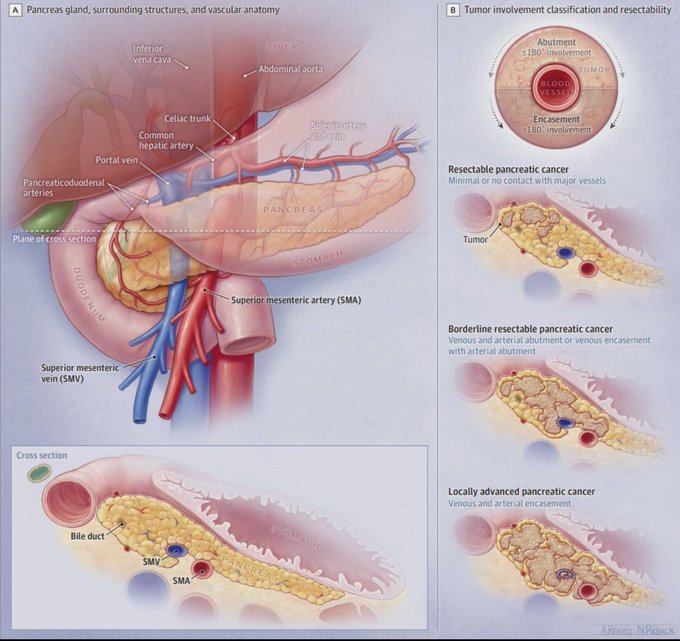
Pancreatic cancer is fearsome indeed, starting with its site of origin. Just as realtors proclaim the importance of location, so the pancreas occupies some of the most high-value anatomy in the body. The organ is buried deep like a secret and it’s no small feat to unearth it safely.

Many surgeons have a saying about operating in this region, the sanitized version of which is: ‘don’t mess with the pancreas’.
One issue is just how closely related the pancreas is to the critical vessels that run across the back of the abdomen.
tl;dr: ‘Don’t cut the red wire!’
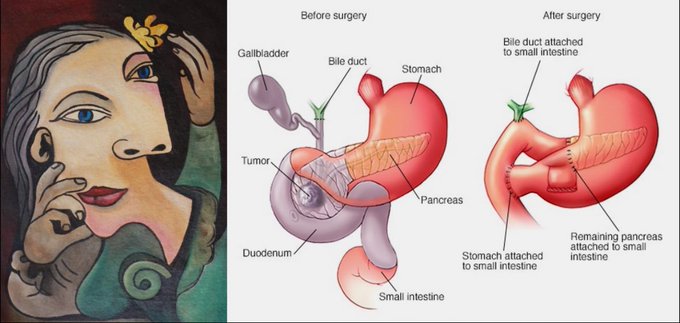
Moreover, the Whipple operation poses a whole other level of technical difficulty I say the procedure does to the gut what Picasso did to faces, rearranging viscera in a profoundly disorienting Cubist fashion (There is no ‘new normal’ after this — digestion is never the same)
In a questionable act of online exhibitionism I asked for my Whipple to be live-Tweeted by my institution’s social media team.My reasoning was that monsters are more scary in the dark so maybe having the process documented step-by-step might be helpful?
And to be honest I still have some patients decline the surgery because of how daunting it seems But the much bigger problem is how few of them are operative candidates at all The paradox of pancreatic adenocarcinoma is that it’s a systemic disease that’s only cured in the OR.
I won’t disclose any of my own patients’ health information but I can relay the story of a colleague — the late Michael Frumovitz of MD Anderson Cancer Center — who was not nearly as fortunate as I’ve been Last fall, as MD Anderson’s Chief Patient Experience officer, he invited me to speak.
It was a wonderful event, and I was honored to address the audience Always up for a tortured metaphor, I likened the embodied experience of cancer to flight. The pilot — my oncologist self — understands the principles involved, But the bird — my patient identity — just FEELS.
So: who, then, is the greater expert? It took me 11 years to become an oncologist and I’ve now practiced a further 12. And yet, absolutely nothing — NOTHING — has taught me as much about cancer as going through treatment myself.
At the time Dr. Frumovitz was undergoing chemotherapy — a taste of my own medicine I’ve so far avoided — in the hopes of rendering his cancer resectable; he even asked me to give him tips on post-op recovery. The week after my talk he learned he was inoperable. He passed away in July.
So this Whipple anniversary weighs heavily on me, realizing how lucky I am to have made it this far, and how much I owe it to my patients to try to extend the same therapeutic opportunities to them.
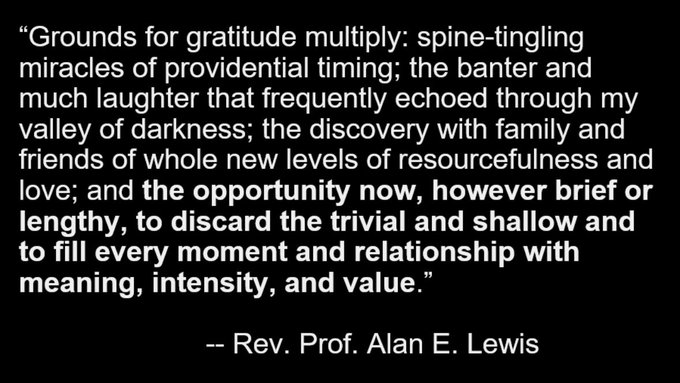
At the very least it’s a vital antidote to self-pity. Every day that I wake up, breathe without a tube down my nose, and eat without parenteral nutrition, is a good day when I can be of service to others. For as my late father wrote, the real question is: Why them? Why not me?
It soon could be. I get scanned every year to see if I will require the same chemotherapy I prescribe. The answer? Not. Yet. But in the meantime I am more and more aware of my completely unearned good luck, that I’ve been truly blessed I didn’t earn it — that’s what makes it grace.
And as for love, I wouldn’t have made it this far without my colleagues and my family, but no one more so than my wife: my best friend, concierge physician (she placed an NG tube (Nasogastric Tube:) at home!), and the woman whose vow to remain with me in sickness and in health has endured every test.
Source: Mark Lewis/X
Mark A. Lewis is the Director of Gastrointestinal Oncology at Intermountain Healthcare in Utah, the Co-Chair of adolescent and young adult (AYA) oncology in the SWOG cooperative group, and the Vice President of American Multiple Endocrine Neoplasia Support. Dr. Lewis is also a well-known patient advocate and social media influencer. His interests are neuroendocrine tumors and cancer syndromes.