Radiotherapy for bladder cancer includes both radical and palliative treatments. Radical radiotherapy targets muscle-invasive or locally advanced bladder cancer with the goal of curing it, while palliative radiotherapy is used to alleviate symptoms in advanced stages of the disease. The treatment involves using high-energy radiation to precisely target cancer cells, often in combination with chemotherapy or other therapies.
Types of Radiotherapy for Bladder Cancer
Radiotherapy for bladder cancer can be delivered in different forms, depending on the stage and goals of treatment. Radical radiotherapy is used to treat muscle-invasive or locally advanced bladder cancer, aiming for a cure. It often involves high doses of radiation combined with chemotherapy or other therapies. On the other hand, palliative radiotherapy is employed in advanced stages to manage symptoms like pain or bleeding, with a focus on improving quality of life rather than curing the disease. The radiation is precisely targeted to the tumor area, minimizing damage to surrounding healthy tissue.
How Effective is Radiotherapy for Bladder Cancer?
Radiotherapy for bladder cancer is effective in treating both muscle-invasive and locally advanced forms of the disease, especially when combined with chemotherapy. Radical radiotherapy can offer a potential cure for some patients, particularly those who are not candidates for surgery. In cases where the cancer is more advanced, palliative radiotherapy can help manage symptoms such as pain or bleeding, improving quality of life. However, its effectiveness can vary depending on factors like the stage of cancer, the patient’s overall health, and whether the radiation is used alone or in combination with other treatments.
A study by Rödel et al. published in 2002 in the Journal of Clinical Oncology evaluated the long-term outcomes of combined radiotherapy (RT) and radiochemotherapy (RCT) for bladder cancer patients seeking bladder preservation. The study included 415 patients, with 72% achieving complete response (CR) after treatment. At 10 years, 64% of those who had CR maintained local control, and 42% had disease-specific survival. RCT proved more effective than RT alone, with a 10-year disease-specific survival of 45% after salvage cystectomy for local failure. Early tumor stage and complete TUR were key factors predicting CR and survival. Over 80% of survivors preserved their bladder.
Success Rates of Radiotherapy for Bladder Cancer
Radiotherapy for bladder cancer has varying success rates depending on the stage of cancer. For early-stage bladder cancer, especially when treated with radical radiotherapy, the success rate can be relatively high, with a significant chance of cure, especially when combined with chemotherapy. Radical radiotherapy aims to treat muscle-invasive or locally advanced bladder cancer, aiming for long-term remission.
In advanced bladder cancer, the goal of radiotherapy shifts toward palliative care, focusing on symptom management and improving quality of life. While the treatment may not cure the cancer in advanced stages, it can provide significant relief from symptoms like pain, bleeding, and obstruction, contributing to a better quality of life.
A study by Hsieh et al. published in 2011 in BMC Radiation Oncology reviewed the use of intensity-modulated radiotherapy (IMRT) and helical tomotherapy (HT) for treating elderly bladder cancer patients. The study involved 19 patients, with median survival of 21 months. The 2-year overall survival (OS) rates were 26.3% for IMRT and 37.5% for HT. Disease-free survival was higher for HT (83.3%) compared to IMRT (58.3%). IMRT and HT showed superior organ-sparing capabilities over conventional 2D pelvic radiation therapy (2DRT). The T category and RT completion time (within 8 weeks) significantly influenced OS rates.
The Procedure and Preparation Steps for Radiotherapy in Bladder Cancer Treatment
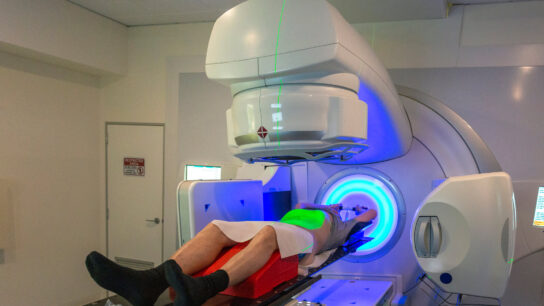
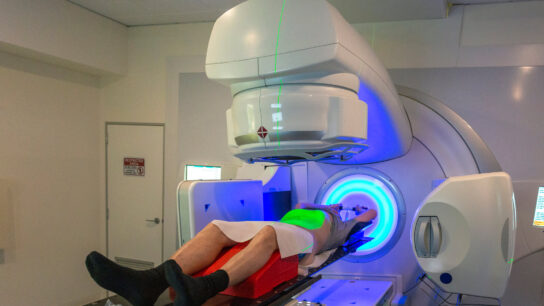
Radiotherapy for bladder cancer involves a well-coordinated preparation and planning process to ensure accurate treatment delivery. Prior to the treatment, patients must follow specific instructions for preparing their bladder and rectum, such as either filling or emptying the bladder to ensure consistent positioning. This preparation is crucial during the CT simulation, where detailed images are taken to map out the treatment area. In some cases, additional MRI scans may be required to help refine the treatment plan. Once the plan is established, patients attend daily radiation sessions, with regular check-ins to confirm correct positioning, and the process aims to minimize side effects by targeting the bladder and surrounding areas precisely.
source: www.cancertherapyadvisor.com
What are the Side Effects of Radiotherapy for Bladder Cancer?
Radiotherapy for bladder cancer can lead to both early and late side effects, affecting various organs. These side effects can vary in intensity depending on the individual and the specifics of the treatment. Below is an overview of common early effects, late effects, and organ-specific issues that may arise.
Early Effects
One of the most common early side effects of radiotherapy is fatigue, where patients may feel unusually tired. This fatigue can worsen as treatment progresses but generally improves 1-2 months after treatment ends. Appetite changes are also frequent, often due to treatment or medications, making patients less hungry. Cramping and diarrhea are also common, especially in the latter weeks of treatment when the radiation may impact the bowel.
Late Effects
Late effects can develop after the treatment concludes and may persist for weeks or months. Continued fatigue and digestive discomfort, such as ongoing diarrhea or bowel issues, may occur. It’s important to understand that these effects often take time to improve and require patience as the body heals. Some late effects, such as bladder discomfort, may take even longer to subside.
Organ-Specific Effects
Radiotherapy can cause issues in organs directly impacted by the treatment. For the bladder, patients may experience painful or frequent urination, and in some cases, a burning sensation when urinating. Sexual function can also be affected, with changes in both desire and ability to engage in sexual activity. It’s crucial for patients to discuss these organ-specific side effects with their healthcare team to manage them effectively.
What Should Patients Expect During Radiation Treatment?
Radiotherapy for bladder cancer begins with a CT simulation to map the treatment area. During each session, patients are positioned on the treatment table, and a Cone Beam CT scan confirms alignment. The session lasts around 20 minutes, with total hospital time of 30-60 minutes. Radiotherapy for bladder cancer is painless, but side effects like fatigue, appetite changes, and digestive discomfort may occur. Regular check-ins with the radiation oncologist help monitor progress and manage side effects.
How Long Does It Take to See Results?
The time it takes to see results from radiotherapy for bladder cancer can vary depending on the individual and the specifics of the treatment. While some patients may begin to notice improvements during the course of treatment, significant changes often take longer to become apparent. Typically, any reduction in symptoms related to bladder cancer may take a few weeks after the treatment ends to become noticeable. It’s important for patients to continue following their healthcare team’s guidance. Regular follow-up appointments are essential to assess the effectiveness of the treatment. Full results may take several months to fully manifest.
What Are the Costs of Radiotherapy for Bladder Cancer?
The cost of radiotherapy for bladder cancer can vary depending on factors like the type of treatment, location, and healthcare facility. It typically includes expenses for the initial simulation, the radiation treatments, and any necessary follow-up care. Other factors, such as whether the patient is receiving additional treatments like chemotherapy, can also influence the overall cost. To get a more accurate estimate, patients should reach out to their healthcare provider or insurance company, as they can provide detailed information based on the individual’s specific needs and circumstances.
A study by Golla et al., published in 2022 in Urologic Oncology: Seminars and Original Investigations, compared the 2- and 5-year costs of trimodal therapy (TMT) versus radical cystectomy (RC) for muscle-invasive bladder cancer using the SEER-Medicare database. The study found that TMT had significantly higher costs than RC, with median costs of $372,839 vs. $191,363 at 2 years and $424,570 vs. $253,651 at 5 years. The increased costs for TMT were largely driven by higher outpatient expenses, including radiology, medications, and lab services, while RC incurred higher inpatient costs. This highlights the need for cost-containment strategies in TMT to optimize future care.
Know Your Doctor, Read Special Article by OncoDaily on Who is a Radiation Oncologist?
How Does Radiotherapy Compare to Other Treatments for Bladder Cancer?
Radiotherapy for bladder cancer is one of several treatment options. It can be used alone or in combination with surgery and chemotherapy, depending on the stage and nature of the cancer. Here’s how radiotherapy compares to these other treatments.
Radiotherapy for Bladder Cancer vs. Surgery
Surgery for bladder cancer may involve removing part or all of the bladder, depending on the cancer’s stage and location. While surgery can offer a more direct way to remove the tumor, it is more invasive and can lead to significant changes in the patient’s body, such as the need for a new way to store and pass urine. On the other hand, radiotherapy for bladder cancer is less invasive and helps to preserve bladder function, though it may come with side effects such as bladder irritation and changes in bowel function.
A 2001 study by Shelley, Barber, Wilt, and Mason, published in The Cochrane Library (Issue 4), compared overall survival rates between radical cystectomy and radical radiotherapy for bladder cancer in muscle-invasive cases. The study included three randomized trials with 439 patients, 221 assigned to surgery and 218 to radiotherapy for bladder cancer. The results showed a higher overall survival for surgery, with 45% at 3 years and 36% at 5 years, compared to 28% and 20% for radiotherapy for bladder cancer, respectively. Analysis favored surgery with significant odds ratios at both 3 and 5 years.
Radiotherapy for Bladder Cancer vs. Chemotherapy
Chemotherapy is sometimes used alongside radiotherapy, especially in cases of more advanced bladder cancer. While chemotherapy works by using drugs to kill cancer cells throughout the body, radiotherapy targets specific areas, minimizing damage to surrounding tissues. The two treatments together can improve outcomes by targeting the cancer from different angles. However, chemotherapy can have its own side effects, such as nausea, fatigue, and a lowered immune response, while radiotherapy tends to have more localized effects, particularly related to the bladder and surrounding organs. The choice of treatment depends on the cancer’s characteristics, the patient’s overall health, and the goals of treatment.
A 2012 phase 3 trial by James et al., published in NEJM, evaluated the effectiveness of chemoradiotherapy versus radiotherapy alone for muscle-invasive bladder cancer. The study involved 360 patients, with results showing 67% locoregional disease-free survival at 2 years in the chemoradiotherapy group compared to 54% in the radiotherapy group. The chemoradiotherapy group had a 48% overall survival at 5 years, versus 35% for radiotherapy alone. While adverse events were slightly higher in the chemoradiotherapy group during treatment, they were similar during follow-up.
How Does Radiotherapy Affect Sexual Health and Fertility?
Radiotherapy for bladder cancer can have an impact on both sexual health and fertility. These effects vary for men and women, with each group experiencing unique challenges. It’s important for patients to be informed and discuss these potential effects with their healthcare team before beginning treatment.
Men’s Sexual Health and Fertility
Radiotherapy may affect erectile function, leading to difficulties in achieving or maintaining an erection. This can be temporary or long-lasting, depending on the area treated and the dose of radiation. Fertility may also be impacted, as radiotherapy can reduce sperm production, leading to lower chances of conception. Men considering fatherhood after treatment should discuss sperm banking options with their healthcare team before starting radiotherapy to preserve fertility.
Women’s Sexual Health and Fertility
Radiotherapy in women can cause vaginal narrowing, dryness, and painful intercourse. It may also affect fertility by damaging the ovaries, potentially leading to infertility. Women should discuss fertility preservation options, like egg freezing, with their healthcare team before starting treatment. Early discussions are crucial for managing fertility and sexual health post-treatment.
A 2011 study by Rodrigues et al., published in Archives of Gynecology and Obstetrics, assessed the impact of pelvic radiotherapy on 199 women. It found higher rates of fatigue, strength loss, diarrhea, vaginal discharge, and skin erythema in radiotherapy patients. These women also had higher levels of stress and lower sexual function and social support satisfaction, though relationship satisfaction was unaffected. The study highlights the need for interventions to address the negative effects of pelvic radiotherapy on female sexuality.
Can All Bladder Cancer Patients Receive Radiotherapy?
Not all bladder cancer patients are candidates for radiotherapy. The decision to use radiotherapy depends on factors like the stage of cancer, the location of the tumor, and the patient’s overall health. Radiotherapy is often considered for patients with muscle-invasive bladder cancer, particularly when surgery is not an option or as part of a combined treatment approach with chemotherapy. For those with early-stage bladder cancer or non-invasive types, surgery or other treatments may be more appropriate. Additionally, some patients may not be eligible for radiotherapy due to pre-existing health conditions, making it essential to evaluate each patient’s individual case.
What Research is Being Done on Radiotherapy for Bladder Cancer?
Retrospective study by Swintonm et al. (2023), published in the Journal of Clinical Oncology, analyzed 287 patients with nonmetastatic clinically node-positive bladder cancer (cN+ M0 BCa). The median overall survival (OS) was 1.55 years. Radical treatments, including radical cystectomy (RC) or radical radiotherapy (RT), significantly improved OS (HR, 0.32; P < .001) compared to palliative care. There was no significant difference in OS or progression-free survival (PFS) between RC and RT, supporting bladder-sparing trimodal therapy (TMT) as a viable alternative to surgery for cN+ M0 BCa patients.
How Can Patients Support Their Health During Radiotherapy?
During radiotherapy for bladder cancer, patients can support their health by eating a balanced diet, staying hydrated, and resting well. Following instructions like maintaining bladder fullness or an empty rectum is essential. Light exercise, such as walking, can help manage fatigue, but overexertion should be avoided. Managing stress and reporting side effects to the healthcare team ensures timely care and support. Regular monitoring helps address any issues promptly. In this resource, you can find support groups for bladder cancer to help patients connect with others and receive emotional support during treatment.
Written by Aren Karapetyan, MD