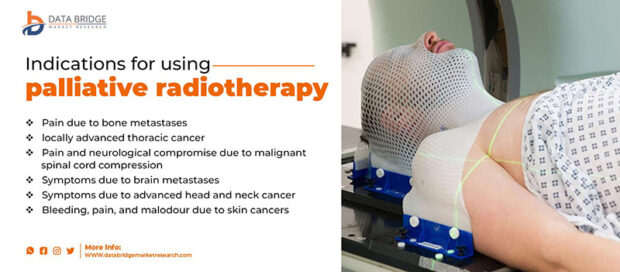
Palliative radiotherapy (PR) plays a key role in relieving symptoms and improving life expectancy after palliative radiotherapy for patients with advanced cancer. It helps manage pain from bone metastases, neurological symptoms from brain or spinal cord metastases, and other issues like airway obstruction. While not curative, PR can sometimes extend life expectancy, particularly in advanced disease. The psychological impact can be significant, offering hope and relief. Studies suggest symptom relief and potential for longer survival in some patients. However, longer courses of PR may delay hospice enrollment, and both radiation duration and hospice time tend to decrease over the years.
What Is Palliative Radiotherapy?
How Does Palliative Radiotherapy Impact Life Expectancy?
Palliative radiotherapy (PR) can indirectly impact life expectancy by improving symptoms such as pain, difficulty breathing, and neurological issues. While its primary goal is not to cure cancer, symptom management can enhance overall well-being, potentially enabling patients to live longer. For example, alleviating pain from bone metastases can improve mobility and reduce the burden on the body, allowing patients to maintain a higher level of function. Similarly, treating symptoms like dyspnea or spinal cord compression can improve quality of life and possibly lead to better outcomes in some cases.
While the duration of survival varies among patients, effective symptom management through PR has been shown to provide a better quality of life, which in some cases results in extended survival beyond initial expectations. These findings highlight the importance of personalized treatment planning, as shorter, well-targeted radiation schedules may contribute to improved symptom control, allowing for longer and more comfortable lives for patients with advanced cancer
Jones et al. (2014), published in A Cancer Journal for Clinicians, highlighted the benefits of palliative radiotherapy for patients with advanced or metastatic cancer, particularly in relieving pain from bone metastases, neurologic symptoms from MESCC, and brain metastases. Radiotherapy can provide pain relief, often within a few weeks of completion, especially for bone metastases. While prognostic models help predict survival, the role of radiotherapy for patients near the end of life remains complex, balancing clinical benefits with the challenges of short survival.
Factors That Influence Life Expectancy After Palliative Radiotherapy
Life expectancy after palliative radiotherapy (PR) is influenced by several factors, including cancer type, tumor location, the extent of metastasis, patient health, age, and overall response to treatment.
Cancer type plays a significant role in determining the outcome of palliative radiotherapy. For example, patients with breast and lung cancers tend to have slightly longer courses of radiation, but they often experience shorter stays in hospice care. Conversely, prostate cancer patients may have different patterns of disease spread, influencing the need for PR (from the study on factors affecting radiation duration and hospice length).
The location of the tumor also affects the effectiveness of PR. Tumors in areas like the brain or spinal cord may require more specific radiation treatments. In some cases, like brain metastases, shorter radiation regimens have been shown to be effective in managing symptoms without significantly impacting survival (from a study of whole-brain radiotherapy and lung metastasis treatment).
The extent of metastasis is another key determinant. The more advanced the metastasis, the more likely a patient will experience limited benefits from longer radiation courses, which may not significantly impact life expectancy. However, for patients with bone metastases, symptom control through palliative radiotherapy can still provide relief and improve quality of life, potentially leading to prolonged survival (from various studies on palliative radiotherapy in advanced cancer).
Krishnan et al. (2012), published in Proceedings of the American Society for Radiation Oncology 54th Annual Meeting, studied factors predicting prognosis in metastatic cancer patients receiving palliative radiation therapy (PRT). The retrospective review of 862 patients found that factors such as cancer type, age, presence of liver metastases, performance status, prior hospitalizations, and number of previous chemotherapy and PRT courses were significantly associated with time to death
Cancer Type and Stage
Different cancers respond to palliative radiotherapy (PR) in varying ways. For instance, lung cancer and breast cancer patients may require longer radiation courses but often have shorter stays in hospice, indicating the complexity of managing advanced stages. Bone metastases commonly respond well to shorter radiation regimens, with symptom relief like pain reduction leading to better quality of life and potential for prolonged survival. However, advanced cancer stages, where metastasis has spread widely, may limit the effectiveness of longer radiation treatments, reducing overall life expectancy. The cancer stage significantly influences the impact of PR, with earlier stages showing more promising responses than advanced, widely metastatic cancers.
Patient Health and Age
A patient’s general health and age play crucial roles in determining life expectancy after palliative radiotherapy (PR). Healthier individuals tend to respond better to treatment, experience fewer complications, and may benefit from longer survival. In contrast, older patients or those with multiple comorbidities may face challenges in treatment response, leading to less improvement in life expectancy. These factors underscore the importance of assessing overall health before prescribing PR to optimize treatment outcomes.
Response to Treatment
A patient’s response to palliative radiotherapy (PR) significantly influences their life expectancy. When symptoms such as pain, difficulty breathing, or neurological issues improve significantly, patients often experience better overall well-being, which may contribute to longer survival. For example, in cases of bone metastases, effective pain relief through PR can enhance mobility and reduce the physical burden, allowing patients to maintain a higher level of function. This improvement in quality of life can lead to extended survival.
Conversely, when treatment is less effective, symptom management may not be as substantial, and patients may not experience the same improvements in their condition. In such cases, the lack of symptom relief can shorten life expectancy and worsen the patient’s quality of life. Therefore, a positive response to PR, including symptom improvement, can result in not only better comfort but also potentially longer survival.
Prognostic Tools and Life Expectancy Estimates
Doctors use various prognostic tools to estimate life expectancy in patients receiving palliative radiotherapy. One key tool is the performance status scale, such as the Karnofsky Performance Scale (KPS), which evaluates a patient’s overall ability to perform daily activities and functions. A lower KPS score often correlates with a poorer prognosis and can help guide treatment decisions, including the use of palliative radiotherapy.
Imaging scans, such as CT, MRI, and PET scans, are also used to assess the extent of disease spread and tumor response, providing valuable insights into how well a patient might respond to treatment. Additionally, blood tests and biomarkers can be used to track a patient’s response to therapy, offering more precise estimates of how the treatment is affecting their condition. For example, markers like lactate dehydrogenase and white blood cell counts can help identify patients at higher risk for poor outcomes, influencing decisions about palliative care and radiotherapy. These tools, along with careful monitoring, help doctors refine life expectancy estimates and adjust treatment plans accordingly.
Can Palliative Radiotherapy Extend Life?
How to Manage Expectations for Life Expectancy After Palliative Radiotherapy?
Managing expectations for life expectancy after palliative radiotherapy involves understanding that the primary focus of the treatment is symptom relief and improved quality of life rather than extending survival. Patients and families should have open discussions with healthcare providers about prognosis, emphasizing the importance of shared decision-making to align treatment goals with personal values and preferences. Healthcare providers can offer guidance on expected outcomes based on factors such as cancer type, disease stage, and response to treatment.
Emotional support is also essential when dealing with uncertain survival outcomes. Recognizing the limits of prognostic tools and focusing on the benefits of symptom control can help patients and families cope with uncertainty. Accessing psychological support services or counseling can provide additional assistance in handling the emotional impact of advanced cancer. This approach helps to create realistic expectations while prioritizing comfort and well-being.
How Does Palliative Radiotherapy Improve Quality of Life?
Palliative radiotherapy improves quality of life by alleviating tumor-related symptoms such as pain, difficulty breathing, and neurological deficits. For example, treating bone metastases can reduce pain and improve mobility, while addressing spinal cord compression or airway obstruction can enhance breathing and overall comfort. By targeting specific symptoms, palliative radiotherapy helps patients maintain physical function and experience less distress, contributing to better overall well-being even in advanced stages of cancer. This symptom relief allows patients to focus on spending meaningful time with loved ones and engaging in daily activities with reduced discomfort.
Learn more about palliative radiotherapy in OncoDaily’s special article
What Are the Risks and Side Effects of Palliative Radiotherapy?
The risks and side effects of palliative radiotherapy vary depending on the treatment area and individual patient factors. Common side effects include fatigue, skin irritation, nausea, and, in some cases, localized pain or swelling. For example, treating bone metastases may cause temporary discomfort at the treatment site, while radiation targeting the head or neck can lead to difficulty swallowing or dry mouth.
Managing these effects often involves personalized care plans. Patients are advised to rest frequently to address fatigue and use gentle skincare routines to minimize irritation. Eating smaller, nutritious meals may help manage nausea, and consulting healthcare providers about medications for symptom relief is crucial. Patients should immediately report severe or persistent side effects, as timely interventions can prevent complications and enhance comfort during treatment.
Short-Term Side Effects
Common short-term side effects of palliative radiotherapy include fatigue, nausea, and localized skin irritation. Fatigue often occurs as the body responds to radiation, and patients are encouraged to rest and conserve energy. Nausea may result from radiation to areas near the stomach or abdomen and can be managed with prescribed anti-nausea medications and light, frequent meals. Skin irritation, such as redness or soreness at the treatment site, can be addressed by using mild skincare products, avoiding tight clothing, and protecting the area from sun exposure. Patients should consult their healthcare team for tailored advice and promptly report severe or worsening symptoms.
Radiation therapy is a crucial cancer treatment, but it comes with the risk of acute and long-term toxicity. Acute toxicity, such as inflammation and discomfort, usually occurs during or shortly after treatment, while long-term effects, including organ dysfunction or fibrosis, may develop months or even years later. Careful assessment and follow-up are vital for detecting and managing these complications. This paper, published by Pushpendra Singh PhD, Alka Mishra M.Tech, and Santosh Kumar Mishra PhD in 2024 in Médecine Palliative, explores these challenges and highlights the importance of vigilance, patient education, and collaboration among healthcare providers to optimize treatment outcomes and manage side effects.
Long-Term Side Effects
Long-term effects of palliative radiotherapy can include tissue changes, such as fibrosis or scarring, which may impact function depending on the treated area. Bone density loss, particularly in areas exposed to radiation, may increase the risk of fractures. Although rare, there is a potential risk of secondary cancers developing years after treatment due to radiation exposure. Patients can mitigate these risks by maintaining regular follow-ups with their healthcare providers, who can monitor for late side effects and provide interventions as needed. Lifestyle adjustments, such as a balanced diet, exercise, and avoiding smoking, can also support long-term health and reduce complications.
How Long After Palliative Radiotherapy Do Symptoms Improve?
Symptom relief after palliative radiotherapy varies by cancer type. For bone metastases, pain relief often starts within 1–2 weeks and improves over several weeks. Lung cancer symptoms like cough or breathing difficulty may improve within days to weeks. Patient-reported outcomes, physical assessments, and imaging scans help monitor effectiveness, and regular follow-ups are essential for symptom management.
Zeng et al. (2011) in Supportive Cancer compared pain and functional interference outcomes in patients with bone metastases treated with palliative radiotherapy. They found significant improvements at 3 and 6 months, regardless of metastasis site. Dose fractionation did not significantly affect the response, with a single 8 Gy fraction providing equal benefits for both spine and non-spine metastases.
What Support Is Available After Palliative Radiotherapy?
After palliative radiotherapy, patients have access to various forms of support aimed at improving their emotional, psychological, and physical well-being. Follow-up care with palliative teams helps monitor symptom relief and manage any side effects. Counseling services are available to address psychological and emotional challenges, providing patients and families with coping strategies. Support groups offer opportunities for patients to share experiences and gain comfort from others facing similar situations. Healthcare providers often emphasize the importance of holistic care, including pain management, nutritional support, and assistance with mobility, to enhance the patient’s quality of life after treatment.
How Does Palliative Radiotherapy Affect Sexual Health and Fertility?
Long-term effects of palliative radiotherapy can include fatigue, tissue damage, and in some cases, the development of secondary cancers. Fatigue is a common side effect that may persist for months after treatment, especially in patients who have received multiple radiation fractions. Tissue damage can occur in areas like the skin, bone, or organs near the treatment site, leading to issues like fibrosis or reduced organ function. For example, radiation to the chest area in lung cancer patients can cause long-term respiratory issues. Secondary cancers, though rare, are a potential risk, particularly when high radiation doses are used. Patients with bone metastases may experience changes in bone density, increasing fracture risk.
The severity of these long-term effects varies by cancer type and the dose of radiation received. For instance, those receiving radiation for brain or spinal cord metastases may have more pronounced neurological effects.
How Can Patients Support Their Health During Radiotherapy?
During palliative radiotherapy, patients can support their health by focusing on both physical and mental well-being. Maintaining a nutritious diet is essential to support energy levels and immune function. A balanced diet helps the body recover and cope with the side effects of treatment, such as fatigue or weight loss. Staying active, within the limits of the patient’s physical condition, can help maintain strength and mobility. Even light exercise like walking or gentle stretching can improve mood and reduce fatigue.
Seeking emotional support is crucial, as treatment can take a toll on mental health. Patients should consider talking to counselors, support groups, or loved ones to help cope with stress and anxiety. Managing emotional health can improve overall quality of life and resilience during treatment. Additionally, it’s important to follow up regularly with healthcare providers to manage any physical or emotional challenges and adjust care plans as needed.
Written by Aren Karapetyan, MD
FAQ
Does Palliative Radiotherapy Cure Cancer?
No, palliative radiotherapy is not aimed at curing cancer. Its primary goal is to relieve symptoms and improve quality of life for patients with advanced cancer.
How Long Does It Take for Symptoms to Improve After Palliative Radiotherapy?
Symptom relief can begin within days to weeks, depending on the cancer type and the targeted symptoms. Pain from bone metastases, for example, may improve quickly after treatment.
What Are the Common Side Effects of Palliative Radiotherapy?
Common short-term side effects include fatigue, nausea, and localized skin irritation. These are typically temporary and can be managed with medication, rest, and skincare.
Can Palliative Radiotherapy Extend Life Expectancy?
While the primary goal is symptom management, in some cases, improved symptom control can contribute to a longer, more comfortable life. However, survival outcomes vary among patients.
How Many Sessions of Palliative Radiotherapy Will I Need?
The number of sessions depends on the cancer type and the symptoms being treated. Some patients may need only a single session, while others may require multiple treatments spread over a few days or weeks.
Can I Continue Other Treatments While Receiving Palliative Radiotherapy?
Yes, many patients continue other treatments such as chemotherapy or pain management alongside palliative radiotherapy. Treatment plans should be coordinated with your healthcare team.
What Support is Available During and After Palliative Radiotherapy?
Support is available through follow-up care with palliative care teams, counseling, and support groups. Emotional and psychological support can be crucial during and after treatment to maintain well-being.
Is Palliative Radiotherapy Painful?
Palliative radiotherapy is generally not painful. While some patients may experience temporary skin irritation or fatigue, the treatment itself is usually well-tolerated.
Can Palliative Radiotherapy Help with Breathing Problems?
Yes, palliative radiotherapy can help alleviate symptoms like difficulty breathing, especially in cases of lung cancer or metastasis to the chest, improving comfort and quality of life.
How Do I Know If Palliative Radiotherapy Is Working?
Your healthcare team will monitor your symptoms regularly to assess the effectiveness of palliative radiotherapy. Improvement in symptoms like pain reduction or better mobility is a sign that the treatment is working.