Brachytherapy for prostate cancer is a type of internal radiation therapy where a radioactive source is placed directly into or near the prostate gland. This targeted approach delivers a high dose of radiation to the tumor while minimizing damage to surrounding healthy tissues such as the bladder and rectum. It is typically used for localized prostate cancer and may be offered alone or alongside external beam radiation therapy, depending on the stage and risk level of the disease.
The procedure is often performed on an outpatient basis and is generally well tolerated. Patients may experience side effects such as urinary urgency, frequency, mild discomfort, or erectile dysfunction, but these are usually manageable and tend to improve over time.
Brachytherapy offers excellent outcomes for carefully selected patients, especially those with low- to intermediate-risk prostate cancer. Its precision and minimally invasive nature help preserve prostate function and reduce the risk of long-term complications, making it an effective and convenient treatment option.
Types of Brachytherapy for Prostate Cancer
Brachytherapy is a highly effective form of internal radiation therapy for prostate cancer, particularly for patients with localized or low- to intermediate-risk disease. It involves placing radioactive sources directly into or near the prostate gland, allowing for the delivery of a high and precise dose of radiation to the tumor while sparing surrounding healthy tissues such as the bladder and rectum. This targeted approach minimizes side effects and preserves important functions.
Brachytherapy offers excellent cancer control and is often chosen for its ability to maintain urinary and sexual function better than some other treatment options. It is especially beneficial for patients seeking a minimally invasive therapy with a shorter recovery time. Clinical studies have shown that prostate brachytherapy provides long-term disease control with a favorable safety profile, making it a strong alternative to surgery or external beam radiation therapy in appropriate cases.
The treatment is typically performed on an outpatient basis, with procedures lasting a few hours and minimal downtime. This makes it convenient for patients while offering effective tumor control. Brachytherapy is particularly valuable for those who are not ideal candidates for surgery or prefer a less invasive option that preserves quality of life.
How Effective Is Brachytherapy For Prostate Cancer?
Brachytherapy has emerged as a highly effective treatment option for localized prostate cancer, offering excellent long-term outcomes with minimal side effects.
Efficacy and Outcomes
- High Cure Rates: Studies have demonstrated impressive long-term survival rates. For instance, at 15 years post-treatment, the overall survival rate was 81%, with a prostate cancer-specific survival rate of 95% PubMed. © 2021 The Authors BJU International © 2021 BJU International.
- Biochemical Control: A study involving 149 men treated with Iodine-125 low-dose-rate (LDR) brachytherapy reported a 98% biochemical control rate at 7 years PMC. ©2023 Feb
- Local Control: Research indicates that high-dose-rate (HDR) brachytherapy provides a 5-year biochemical disease-free survival rate exceeding 97%, with a median nadir PSA of 0.08 ng/mL Translational Andrology and Urology. ©2018 June
Advantages Over Other Treatments
- Minimized Side Effects: Brachytherapy delivers a high dose of radiation directly to the prostate, reducing exposure to surrounding healthy tissues and minimizing side effects such as incontinence and erectile dysfunction .Legacy Health ©
- Shorter Treatment Duration: Unlike external beam radiation therapy, which may require daily sessions over several weeks, brachytherapy typically involves a single outpatient procedure, allowing for a quicker return to daily activities.
- Cost-Effectiveness: Due to its shorter treatment course and reduced need for follow-up care, brachytherapy is often more cost-effective compared to other radiation therapies .PMC ©2020 Nov
The Procedure and Preparation Steps for Brachytherapy in Prostate Cancer Treatment
Before prostate cancer brachytherapy, doctors use advanced imaging techniques such as transrectal ultrasound, CT, or MRI to carefully map the size, shape, and position of the prostate. This imaging helps create a personalized treatment plan to accurately position the radioactive sources and ensure optimal dose delivery while protecting surrounding organs like the bladder and rectum. The medical team thoroughly explains the procedure, answers any questions, and discusses what to expect during and after treatment, including whether the radiation will remain in the body and any potential side effects.
During the procedure, thin needles or applicators are inserted into the prostate to deliver the radioactive material. In High-Dose-Rate (HDR) brachytherapy, the radiation source is temporarily placed inside the applicators for a few minutes, then removed. The treatment is typically done under spinal or general anesthesia and may be completed in one or a few outpatient sessions. Patients usually go home the same day and can resume normal activities within a short period.
For Low-Dose-Rate (LDR) brachytherapy, tiny radioactive seeds are permanently implanted into the prostate, where they release radiation gradually over several weeks. This approach may require a short hospital stay or be performed on an outpatient basis. While the seeds remain in the body, the radiation levels are low and decrease over time. Patients may be advised to follow temporary safety precautions, such as avoiding prolonged close contact with young children or pregnant women.
Most side effects are mild and short-lived, such as urinary urgency, frequency, or discomfort. Fatigue may occur but usually improves within days. After the procedure, follow-up appointments are scheduled to monitor the effectiveness of the treatment, check PSA levels, and address any ongoing symptoms. Brachytherapy offers a targeted and well-tolerated option for managing localized prostate cancer, with the goal of maintaining quality of life while achieving excellent cancer control.
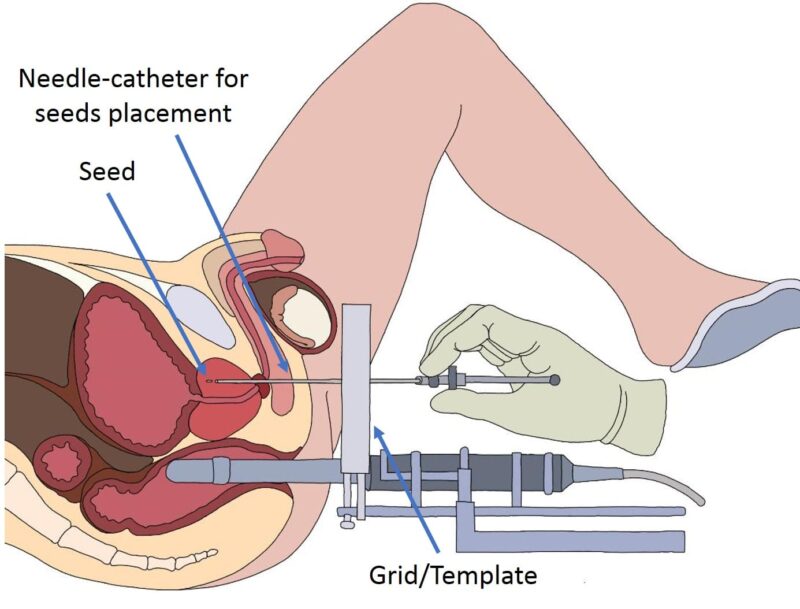
source: www.prostatherapy.com
Brachytherapy Side Effects: What Should You Expect?
Brachytherapy is a highly effective treatment for localized prostate cancer, offering excellent long-term cancer control with a focused delivery of radiation directly to the prostate. Because the radiation is confined to a small area, damage to surrounding organs like the bladder and rectum is minimized. Most patients tolerate the procedure well, but like all treatments, brachytherapy can come with side effects—usually mild to moderate in severity.
In the short term, patients may experience urinary symptoms such as increased frequency, urgency, a burning sensation during urination, or difficulty starting the flow. These symptoms typically develop within the first few weeks after treatment and gradually improve over time. Mild rectal irritation, such as occasional discomfort or minor bleeding, may also occur. Some patients report temporary fatigue during the recovery phase, especially after High-Dose-Rate (HDR) brachytherapy sessions.
To help manage these symptoms, doctors may recommend medications like alpha-blockers to relax the bladder and reduce urinary discomfort. Staying hydrated, avoiding caffeine, and limiting alcohol intake can also help ease bladder irritation.
Long-term side effects are less common but can include persistent urinary difficulties, erectile dysfunction, or, more rarely, rectal bleeding or scarring. For Low-Dose-Rate (LDR) brachytherapy, patients with permanent radioactive seeds may be advised to follow short-term precautions around pregnant women or small children until radiation levels subside.
Most patients experience a gradual return to normal urinary and sexual function within months after treatment. Regular follow-up visits allow the care team to monitor PSA levels, assess side effects, and ensure the treatment is working as expected. With its targeted precision and organ-sparing approach, prostate brachytherapy offers high success rates and a good quality of life for many men facing early-stage prostate cancer.
How Long Does It Take to See Results?
The timeline for seeing results from prostate cancer brachytherapy can vary depending on the type of brachytherapy used and individual tumor characteristics. Unlike treatments with immediate visible outcomes, the effects of brachytherapy unfold gradually as the radiation continues to act on cancer cells over time.
For both High-Dose-Rate (HDR) and Low-Dose-Rate (LDR) brachytherapy, prostate-specific antigen (PSA) levels are the main way to track treatment response. A steady decline in PSA is expected over several months, and in some cases, it may take up to two years or more for PSA to reach its lowest point, known as the PSA nadir. This slow drop is normal and reflects the ongoing effect of radiation on the prostate tissue.
In terms of symptom relief, some men notice improvements in urinary symptoms or discomfort within weeks or months following the procedure. However, others may experience temporary increases in urinary frequency, urgency, or mild discomfort during the early post-treatment period before things start to improve.
For most patients with localized prostate cancer, brachytherapy offers excellent long-term control, and treatment success is typically confirmed through routine PSA monitoring during follow-up visits. These check-ups are essential to ensure that the cancer is responding appropriately and to address any side effects or concerns that arise during the healing process.
Communication with the care team is important, especially if there are changes in urinary or sexual function, or if new symptoms develop. With its high precision and durable outcomes, brachytherapy continues to be a trusted and effective treatment for many men with prostate cancer.
How Much Does Brachytherapy Cost?
The cost of brachytherapy for prostate cancer can vary significantly depending on a range of factors, including the type of brachytherapy used (High-Dose-Rate or Low-Dose-Rate), the patient’s geographic location, and whether the treatment is delivered in a public or private healthcare facility.
In the United States, the total cost for prostate brachytherapy typically ranges from $10,000 to $40,000. This amount generally includes the procedure itself, pre-treatment imaging and planning (such as MRI or ultrasound), anesthesia, follow-up appointments, and any additional supportive care or medications. If brachytherapy is combined with external beam radiation therapy (EBRT) or hormone therapy, the overall cost can be higher.
In Europe, costs are usually lower, ranging from €5,000 to €20,000, depending on the country, the type of facility (public vs. private), and the scope of the treatment plan. In many European countries with universal healthcare systems, a significant portion of the cost may be covered by national health insurance, leaving patients with little to no out-of-pocket expenses.
In countries such as India, Thailand, or other parts of Southeast Asia, the cost of prostate brachytherapy can be considerably more affordable, typically ranging from $3,000 to $8,000. These lower costs are due to reduced overheads and more affordable healthcare infrastructure, making them attractive options for medical tourism.
Additional expenses may include pre-treatment diagnostics, laboratory tests, medications to manage side effects, and follow-up imaging. In most cases, insurance coverage can significantly reduce out-of-pocket costs, especially in countries where brachytherapy is recognized as a standard treatment for localized prostate cancer. Because individual costs can vary widely, it’s important for patients to consult with their healthcare provider and insurance company to get a clear estimate of what is covered and what they may be responsible for. Financial counseling services offered at many cancer centers can also help navigate insurance and payment options.
How Does Brachytherapy Compare to Other Treatments for Prostate Cancer?
Brachytherapy is a well-established treatment for localized prostate cancer, offering precise radiation delivery directly to the prostate gland. Its effectiveness and suitability depend on various factors, including the cancer’s stage, the patient’s overall health, and personal preferences.
Chen et al. (2017) in JAMA Oncology compared quality of life (QOL) after prostate cancer treatments vs. active surveillance in 1141 men. At 3 months, radical prostatectomy (RP) worsened sexual dysfunction and urinary incontinence compared to active surveillance (AS). 1 External beam radiotherapy (EBRT) and brachytherapy (BT) worsened short-term urinary obstruction/irritation, and EBRT worsened short-term bowel symptoms vs. AS. By 24 months, mean QOL scores between treatment groups and AS were not significantly different in most domains. Conclusion: Treatments have distinct short-term adverse effect patterns over 2 years.
Brachytherapy vs. Surgery (Radical Prostatectomy)
Surgery involves the complete removal of the prostate gland and is often recommended for younger patients with localized cancer. Brachytherapy, on the other hand, is less invasive and typically associated with a quicker recovery. Studies have shown comparable long-term cancer control between the two treatments. However, surgery may carry a higher risk of urinary incontinence and erectile dysfunction, while brachytherapy patients might experience urinary irritation or bowel issues in the short term.
Chen et al. (2017) in JAMA Oncology compared quality of life (QOL) after prostate cancer treatments vs. active surveillance in 1141 men. At 3 months, radical prostatectomy (RP) worsened sexual dysfunction and urinary incontinence compared to active surveillance (AS). External beam radiotherapy (EBRT) and brachytherapy (BT) worsened short-term urinary obstruction/irritation, and EBRT worsened short-term bowel symptoms vs. AS. By 24 months, mean QOL scores between treatment groups and AS were not significantly different in most domains.Treatments have distinct short-term adverse effect patterns over 2 years.
Brachytherapy vs. External Beam Radiation Therapy (EBRT)
EBRT delivers radiation from outside the body over several weeks, whereas brachytherapy places radioactive sources directly into the prostate, allowing for higher radiation doses in a shorter period. Research indicates that brachytherapy may offer better long-term control for certain risk groups. For instance, a study found that the 10-year freedom from salvage therapy was 93.2% for brachytherapy compared to 72.2% for external radiation . Additionally, brachytherapy tends to spare surrounding healthy tissues more effectively, potentially reducing side effects.
Brachytherapy vs. Hormone Therapy
Hormone therapy aims to reduce testosterone levels, slowing the growth of prostate cancer cells. It’s often used in combination with other treatments for advanced or high-risk prostate cancer. While hormone therapy can be effective, it doesn’t provide a curative approach when used alone. Brachytherapy offers a localized treatment option with curative intent for many patients. Combining brachytherapy with hormone therapy may improve outcomes in certain cases, but the benefits should be weighed against potential side effects .
Brachytherapy vs. Active Surveillance
Active surveillance involves closely monitoring prostate cancer without immediate treatment, suitable for men with low-risk, slow-growing tumors. Brachytherapy becomes a consideration when there’s evidence of cancer progression or if the patient prefers active treatment. It offers a balance between effective cancer control and preserving quality of life, especially for those seeking a less invasive option.
Read OncoDaily’s Special Article About Brachytherapy
Can All Prostate Cancer Patients Receive Brachytherapy?
Not all prostate cancer patients are suitable candidates for brachytherapy. The decision to use this treatment depends on several factors, including the cancer’s stage, Gleason score, PSA levels, prostate size, and the patient’s overall health. Brachytherapy is most effective for patients with localized prostate cancer, particularly those with low to intermediate-risk profiles. It is often used for early-stage prostate cancer that is less likely to spread beyond the prostate.
The European Association of Urology (EAU), the European Society for Radiotherapy and Oncology (ESTRO), and the International Society of Geriatric Oncology (SIOG) suggest that brachytherapy is a viable option for men with localized prostate cancer who meet these criteria.
In the United States, the American Society of Clinical Oncology (ASCO) and Cancer Care Ontario recommend brachytherapy as a suitable treatment for low-risk prostate cancer patients. However, brachytherapy may not be suitable for men with advanced prostate cancer that has spread beyond the prostate, those with large prostates over 60 cubic centimeters, or those with significant urinary symptoms. It is also generally not recommended for men who have previously received pelvic radiation therapy or those with certain anatomical challenges, such as a large median lobe of the prostate.
If brachytherapy is not suitable, other treatment options, such as external beam radiation therapy (EBRT), hormone therapy, or surgery, may be considered. The decision-making process for treatment should involve a multidisciplinary medical team that carefully evaluates all factors specific to the patient. Patients should discuss the available treatment options, potential benefits, and associated risks with their healthcare providers to determine the best approach for their individual needs.
How Does Brachytherapy Affect Sexual Health and Fertility?
Prostate brachytherapy can affect sexual health and fertility due to its proximity to reproductive organs. Patients may experience erectile dysfunction, reduced libido, or discomfort during intercourse. Fertility can also be impacted, especially if radiation exposure involves the testes. It’s important for patients to discuss potential side effects with their healthcare team and explore options for managing these concerns. Supportive care, including counseling, physical therapy, and medical interventions, can help address these issues and improve quality of life.
Sexual Health
Erectile dysfunction (ED) is a potential side effect of prostate brachytherapy. Approximately 50% of patients may develop ED within five years of treatment . However, many men maintain sexual function without pharmacologic support, and the use of medications like sildenafil can improve erectile function in some cases. Ejaculatory function is often preserved, but some men may experience a reduction in ejaculate volume and a decrease in orgasm intensity.
Cesaretti et al. (2007) published in BJU International evaluated the effect of low-dose rate prostate brachytherapy on sexual health over ≥7 years in men with optimal pre-treatment function. Of 131 men with optimal baseline function, 40% used pharmacological intervention at last follow-up. Age at implantation was highly predictive of erectile function (EF). Men aged 50–59 had current EF ≥2 in 92%, compared to 64% (60–69 years) and 58% (70–78 years) (P=0.01). A current IIEF-5 score ≥16 also correlated highly with age: 64% (50–59), 27% (60–69), and 19% (70–78) (P<0.001). Patients aged <60 years with optimal pre-treatment EF have a very high probability of long-term EF.
Fertility
Brachytherapy can lead to infertility due to damage to sperm-producing cells in the testes. Semen quality may be compromised, affecting sperm count and motility . It’s advisable for men considering fatherhood to discuss sperm banking before treatment.
Tran et al. (2015) published in Urology compared prostate cancer treatments regarding fertility. Prostatectomy causes 100% obstructive infertility. External radiotherapy doses cGy reduce sperm count; 15-35 cGy causes oligozoospermia; 35-50 cGy causes reversible azoospermia (testicular dose cGy). Brachytherapy seems less harmful with lower testicular doses ( cGy). Hormonal therapy infertility is likely reversible. Focal therapy and fertility are not well evaluated. Active surveillance best preserves fertility. Urologists should discuss infertility with younger patients, perform semen analysis if interested in future fertility, and offer cryopreservation as the only preemptive option.
Recovery After Brachytherapy for Prostate Cancer
Recovery after brachytherapy for prostate cancer typically involves a period of rest and gradual resumption of normal activities, with a focus on managing side effects and monitoring healing. In the first few days following treatment, patients are advised to avoid strenuous physical activities and heavy lifting to minimize irritation and allow the body to heal. Some men may experience mild discomfort, such as urinary irritation, frequency, or urgency, as well as temporary fatigue. These symptoms generally improve over time, but it’s important for patients to follow specific instructions provided by their healthcare team.
Common side effects of prostate brachytherapy include urinary symptoms, such as increased frequency, urgency, or a weak stream. These symptoms are typically temporary and can be managed with medications or lifestyle adjustments. Some patients may also experience rectal irritation or discomfort, including mild diarrhea or a sensation of fullness, but these symptoms usually resolve within a few weeks.
It’s normal for patients to feel more fatigued in the early stages of recovery. Ensuring proper hydration, eating a balanced diet, and getting enough rest can help maintain energy levels and support the recovery process. Patients should also take care to stay hydrated and avoid constipation, as straining can exacerbate some side effects.
While most side effects are mild and temporary, some men may experience changes in sexual function, such as erectile dysfunction or reduced libido. These issues may improve over time, but in some cases, they may persist. Patients should discuss any concerns about sexual health with their healthcare team, who can offer support and potential treatments. It’s essential to monitor for any signs of complications during recovery, such as severe pain, blood in the urine or stool, or signs of infection. If any unusual symptoms occur, patients should contact their healthcare provider immediately. Follow-up appointments are crucial to monitor the progress of recovery, address any long-term effects, and ensure that the cancer treatment is working as expected.
How Can Patients Support Their Health During Brachytherapy for Prostate Cancer?
During recovery from brachytherapy for prostate cancer, patients can take several steps to support their overall health and improve the healing process. It’s crucial to attend all follow-up appointments and adhere to the pre- and post-treatment instructions provided by the healthcare team. This ensures the treatment remains as effective and safe as possible. Patients should report any unusual symptoms, such as increased urinary discomfort, blood in the urine, or signs of infection, so that the medical team can address them promptly.
Common side effects of brachytherapy for prostate cancer include urinary symptoms like increased frequency, urgency, or a weak stream, as well as mild rectal discomfort or irritation. These side effects are usually temporary and can be managed with medications or lifestyle changes. Staying hydrated and eating a well-balanced diet with plenty of fruits, vegetables, and lean proteins helps support recovery and maintain energy levels. Avoiding alcohol and smoking is also recommended, as these can hinder the healing process and increase the risk of complications.
Getting adequate rest is essential, as the body needs time to heal from the radiation therapy. Gentle activities like light walking, stretching, or other forms of mild exercise can improve circulation, mood, and energy levels but should only be done with the approval of the healthcare provider. This can also help prevent issues like fatigue and improve overall well-being during the recovery phase.
Maintaining emotional well-being is just as important as physical recovery. The treatment process can be stressful, and many patients may experience anxiety or concerns about side effects, including changes in sexual function or urinary health. It can be helpful to talk to a counselor, join a support group, or discuss feelings with a trusted friend or family member. Patients are encouraged to ask questions about any concerns related to their treatment, potential long-term effects, or ways to manage side effects. By staying informed, staying positive, and advocating for their needs, patients can feel more supported throughout the recovery process.
Written by Nare Hovhannisyan, MD
FAQ
What is brachytherapy for prostate cancer?
Brachytherapy for prostate cancer is a form of internal radiation therapy where small radioactive seeds are implanted directly into or near the prostate tumor. This treatment delivers high doses of radiation to the cancer cells while minimizing exposure to surrounding healthy tissues.
What types of prostate cancer can be treated with brachytherapy?
Brachytherapy is most effective for localized prostate cancer, particularly in early-stage cases with a low to intermediate risk of spreading. It is commonly used for patients with tumors confined to the prostate, with a Gleason score of 7 or lower and a PSA level under 10 ng/ml.
How does brachytherapy work?
During brachytherapy, small radioactive seeds are implanted into the prostate, emitting radiation directly to the tumor site. This concentrated radiation kills cancer cells while minimizing damage to nearby healthy tissues, such as the bladder and rectum.
Is brachytherapy safe for treating prostate cancer?
Yes, brachytherapy is considered a safe and effective treatment for localized prostate cancer. It is especially beneficial for patients who want to avoid surgery or for those with prostate tumors in locations that are difficult to treat with external beam radiation.
What are the benefits of brachytherapy over traditional radiation?
Brachytherapy delivers a highly focused dose of radiation directly to the tumor, reducing the risk of side effects to surrounding healthy tissue. It typically requires fewer treatment sessions compared to external beam radiation therapy (EBRT), and it can be performed on an outpatient basis, allowing patients to recover more quickly.
How long does a brachytherapy session take for prostate cancer?
Each brachytherapy session for prostate cancer typically lasts about 1 to 2 hours. The number of sessions may vary, but most patients will have a single session that involves implanting radioactive seeds in the prostate. In some cases, multiple sessions may be required.
What are the side effects of brachytherapy for prostate cancer?
Side effects can include urinary symptoms such as increased frequency, urgency, or a weak stream. Some men may experience rectal irritation, mild discomfort, or temporary erectile dysfunction. These side effects are usually temporary and improve over time.
How should I care for myself after brachytherapy for prostate cancer?
After brachytherapy, it’s important to stay hydrated, eat a balanced diet, and follow your healthcare provider’s instructions regarding post-treatment care. You may be advised to avoid strenuous activities, heavy lifting, or sexual intercourse for a period of time. It’s also important to monitor for any signs of complications, such as severe pain or bleeding, and report them to your healthcare team.
Can I resume normal activities after brachytherapy for prostate cancer?
Most patients can resume light activities within a few days, but it’s recommended to avoid strenuous exercise, heavy lifting, or sexual activity until cleared by your healthcare provider. You should also avoid sitting for extended periods to reduce pressure on the prostate
Is brachytherapy for prostate cancer painful?
The procedure itself is generally not painful, as it is done under anesthesia. However, you may experience some mild discomfort, such as urinary irritation or pelvic tenderness, after the treatment. These symptoms are typically temporary and can be managed with medications as prescribed by your doctor.