Imagine a treatment so precise that it delivers powerful radiation directly to a tumor while barely affecting the healthy tissue around it. Brachytherapy is a highly targeted form of internal radiation therapy, placing tiny radioactive sources exactly where they are needed most. Unlike traditional radiation that comes from outside the body, this method works from within, allowing for stronger, more effective doses with fewer side effects. Whether used alone or alongside other treatments, brachytherapy provides an efficient way to fight cancer while helping patients maintain their quality of life.
What Is Brachytherapy?
Brachytherapy is a type of internal radiation therapy where tiny radioactive sources are placed directly inside or near a tumor. This precise placement allows for high-dose radiation to target cancer cells while minimizing exposure to surrounding healthy tissues. By delivering radiation from within, brachytherapy ensures a more focused and effective treatment, reducing side effects and preserving nearby organs.
How Does Brachytherapy Work?
Brachytherapy works by placing tiny radioactive sources, such as seeds, wires, or discs, directly inside or near the tumor. These sources emit radiation over a set period, delivering high doses precisely to cancer cells while sparing healthy tissue. Depending on the type of cancer and treatment plan, the radiation may be delivered temporarily or permanently. Temporary brachytherapy involves placing the radioactive material for a short time before removal, while permanent brachytherapy leaves tiny seeds in place, gradually releasing radiation until they become inactive. This targeted approach ensures effective cancer treatment with minimal side effects.
What Are the Main Types of Brachytherapy?
Brachytherapy comes in two main types: high-dose-rate (HDR) and low-dose-rate (LDR), each tailored to different cancers and treatment goals. HDR brachytherapy delivers a powerful dose of radiation in a short time, often in multiple sessions. A small, temporary radioactive source is placed inside or near the tumor and then removed after treatment. It’s commonly used for cervical, breast, and prostate cancers, offering an effective option with shorter treatment durations and quicker recovery.
LDR brachytherapy involves implanting tiny radioactive seeds that slowly release radiation over days or weeks. These seeds may stay in the body permanently, gradually losing their radioactivity over time. LDR is frequently used for prostate cancer, where the seeds provide continuous treatment with minimal disruption to daily life. Both approaches precisely target tumors while reducing radiation exposure to surrounding healthy tissue, making brachytherapy a valuable option for many patients.
High-Dose-Rate (HDR) Brachytherapy
HDR brachytherapy delivers high doses of radiation in a short amount of time by temporarily placing a small, highly radioactive source inside or near the tumor. This is done through thin tubes or applicators, allowing precise targeting of cancer cells while protecting healthy tissues. The radiation source is removed after each session, meaning no radioactivity remains in the body. This treatment is commonly used for cervical, breast, prostate, and lung cancers. Since HDR brachytherapy is usually performed on an outpatient basis, patients can return home the same day. It offers shorter treatment times, fewer sessions, and faster recovery compared to other radiation therapies, making it a convenient and effective option.
Low-Dose-Rate (LDR) Brachytherapy
LDR brachytherapy involves placing tiny radioactive sources, such as seeds, inside or near the tumor, where they slowly release radiation over days, weeks, or even permanently. These seeds gradually lose their radioactivity and remain in the body without causing harm.
This approach is commonly used for prostate cancer, as well as some gynecologic and head and neck cancers. It provides continuous radiation treatment without requiring daily hospital visits. Since the radiation is delivered in a controlled, low-dose manner, surrounding healthy tissues are less affected, leading to fewer side effects. LDR brachytherapy is a well-tolerated, effective option that allows patients to resume normal activities quickly.
What Types of Cancer Are Treated with Brachytherapy?
Brachytherapy is highly effective in treating several cancers, including prostate, cervical, breast, and some head and neck cancers.
Prostate cancer
Prostate cancer is one of the most common uses for brachytherapy, particularly LDR, where radioactive seeds provide continuous, localized radiation. Crook et al. (2022, Int J Radiat Oncol Biol Phys) reported a prospective phase 2 trial (NCT00450411) on salvage low-dose-rate brachytherapy (LDR-BT) for local failure of prostate cancer after EBRT. With a median 6.7-year follow-up of 92 analyzable patients, the 10-year overall survival was 70%. Ten-year failure rates were local 5%, distant 19%, and biochemical 46%. Five-year freedom from biochemical failure was 68%.
Cervical cancer
Han et al. (2024, Int J Radiat Oncol Biol Phys) found that while brachytherapy use for stage IB2-IVA cervical cancer (treated with EBRT) declined in the early 2000s, it improved to 76% by 2018-2020. Brachytherapy was linked to better survival outcomes, independently lowering cervical cancer mortality (HR 0.70) and overall mortality (HR 0.72).
Breast cancer
Patients may receive brachytherapy as part of accelerated partial breast irradiation (APBI), allowing for shorter treatment durations and reduced exposure to surrounding tissues. Research has shown that APBI with brachytherapy achieves similar long-term outcomes to whole-breast radiation, with fewer side effects.
Strnad et al. (2023, Lancet Oncol) reported 10-year results of a phase 3 trial comparing accelerated partial breast irradiation (APBI) via multicatheter brachytherapy to whole-breast irradiation after breast-conserving surgery for early breast cancer. 1 The 10-year local recurrence rate was 3.51% in the APBI group and 1.58% in the whole-breast irradiation group (difference 1.93%, p=0.074). 2 APBI was associated with significantly fewer grade 3 late side-effects (1% vs 4%, p=0.021). 1 The authors concluded APBI is a valuable alternative with comparable efficacy and fewer late side-effects.
Head and neck cancers
Head and neck cancers such as those affecting the tongue and lips, can also benefit from brachytherapy, especially when surgery is not an option. It provides highly localized treatment, reducing damage to critical structures.
Consuegra et al. (2025, Head Neck) reported long-term outcomes of adjuvant high-dose rate (HDR) brachytherapy alone or combined with EBRT/chemoradiation in 152 resected head and neck cancer (HNC) patients. At a median 8.1-year follow-up, the 5-year local control rate was 85.5%, and the 5-year overall survival rate was 62.2%. Grade ≥3 adverse events occurred in 26.3% of patients. The study suggests adjuvant HDR brachytherapy is a feasible option with comparable outcomes to standard chemoradiation
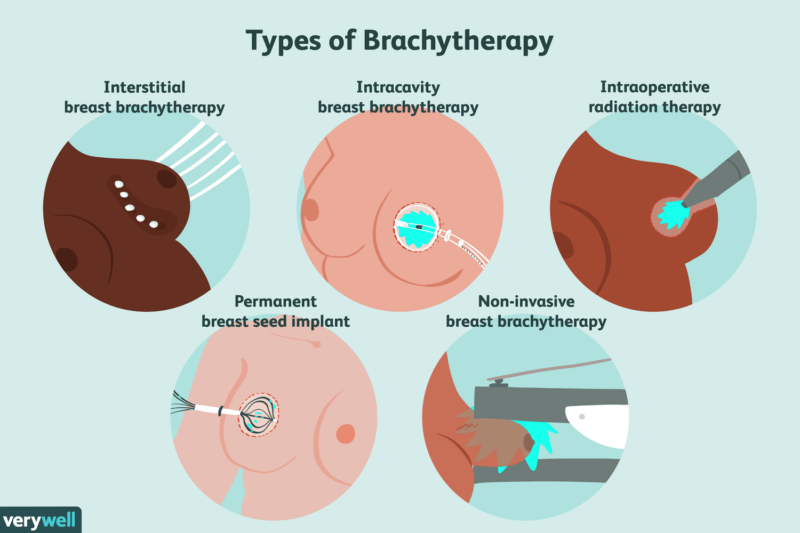
source: www.verywellhealth.com
What to Expect During Brachytherapy?
Before Treatment
Before the procedure, doctors use imaging scans like CT, MRI, or ultrasound to carefully plan where to place the radioactive sources. Depending on the type of treatment, anesthesia or sedation may be used for comfort. The medical team explains the process and answers any concerns, like whether radiation will stay in the body permanently or if the procedure will be painful.
During Treatment
Once positioned, the treatment begins. In HDR brachytherapy, thin tubes or applicators are placed near or inside the tumor, delivering radiation for a few minutes before removal. LDR brachytherapy involves implanting tiny radioactive seeds that release radiation gradually over time. The radiation itself cannot be felt, and the procedure is designed to be quick and effective. HDR sessions are usually outpatient, while LDR may require a short hospital stay.
After Treatment
Most HDR patients go home the same day, while LDR patients may stay briefly for monitoring. Some mild swelling, discomfort, or fatigue may occur but usually fades quickly. If permanent seeds were implanted, doctors provide simple guidelines, such as temporary precautions around small children and pregnant women. Follow-up visits help track progress and ensure the treatment is working as expected.
Brachytherapy Side Effects: What Should You Expect?
Brachytherapy is designed to target cancer with high precision, minimizing damage to healthy tissues and reducing side effects compared to external radiation therapy. However, some side effects may still occur, varying based on the treatment area, radiation dose, and individual factors. Most patients tolerate brachytherapy well and find that any side effects are manageable, especially compared to other cancer treatments.
Short-Term Side Effects of Brachytherapy
Short-term effects of brachytherapy are usually mild and depend on the area being treated. Some patients experience localized pain, swelling, or discomfort at the treatment site, which typically fades within days or weeks. If applicators or implants are used, there may be temporary irritation or tenderness. Fatigue is also common, especially if brachytherapy is combined with other treatments. For prostate cancer, urinary symptoms like frequency or urgency may occur, while gynecologic or breast treatments might cause mild soreness. Most side effects are manageable with rest, hydration, and medication if needed, and doctors provide guidance to ensure a smooth recovery.
Managing Short-Term Side Effects
Managing discomfort after brachytherapy is usually simple with the right care. Over-the-counter pain relievers like ibuprofen or acetaminophen can help with mild pain or swelling, but it’s always best to check with a doctor before taking any medication. Keeping the treatment area clean and dry reduces the risk of irritation or infection, especially for procedures involving applicators or implants. Wearing loose, comfortable clothing can prevent unnecessary pressure on sensitive areas. Staying hydrated and following a balanced diet support healing, while light activities like walking can help with fatigue. If discomfort persists or new symptoms appear, consulting a healthcare provider ensures proper symptom relief and a smoother recovery.
Long-Term Side Effects of Brachytherapy
While brachytherapy is highly effective with minimal side effects, some patients may experience late effects months or even years after treatment. These are typically less common but can occur depending on the location of the treatment and individual factors.
One potential late effect is tissue fibrosis, where the treated area may develop scar tissue, leading to stiffness or reduced flexibility. This can sometimes affect the function of organs nearby, depending on where the radiation was applied. For example, in prostate cancer treatment, patients might experience changes in urinary function, such as difficulty or discomfort when urinating, due to scarring in the bladder or urethra.
In cases of breast cancer, brachytherapy can sometimes cause changes in breast tissue, such as firmness or a slight change in shape. Similarly, for gynecological cancers, radiation might lead to vaginal dryness or narrowing, which can affect sexual health and comfort.
Reducing the Risk of Long-Term Side Effects
To minimize long-term risks after brachytherapy, it’s important to stay on top of regular follow-up appointments with your healthcare provider. These check-ups help monitor any changes in tissue or organ function, allowing for early detection of potential late effects and adjustments to your care plan if needed.
Adopting a healthy lifestyle is also key. A balanced diet rich in fruits, vegetables, and lean proteins supports healing and overall health. Regular physical activity can improve circulation, reduce fatigue, and aid in recovery. Avoiding smoking and limiting alcohol consumption will further support your body’s healing process.
Following your post-treatment care plan is equally important. Adhering to any prescribed medications or therapies and incorporating recommended exercises, such as pelvic floor exercises for certain cancers, can ensure the best recovery. By staying proactive with your care and maintaining a healthy lifestyle, you can minimize long-term risks and continue leading a fulfilling life after treatment.
What Are the Signs Brachytherapy Is Working?
Indicators of treatment effectiveness after brachytherapy include a reduction in tumor size, stabilization of the disease, and resolution of symptoms. A decrease in the size of the tumor, observed through follow-up imaging like CT scans or MRIs, often indicates that the treatment is working and the cancer is responding to the radiation. If the disease is stabilized, it means the cancer is no longer growing or spreading, which is a positive sign of effective treatment.
Resolution of symptoms, such as pain or discomfort, also signals the success of the treatment, particularly when symptoms linked to the tumor are relieved. For instance, if a patient with prostate cancer experiences fewer urinary symptoms after treatment, it can be a sign that the tumor has shrunk and pressure on surrounding tissues has lessened.
Comparison: Brachytherapy vs. External Radiation Therapy
Brachytherapy and external radiation therapy are both effective, but they differ in several ways.
Precision
Brachytherapy is highly targeted. It places radioactive sources directly inside or near the tumor, delivering radiation to the tumor while sparing healthy tissue. External radiation therapy, on the other hand, uses radiation beams from outside the body, which can affect both the tumor and surrounding healthy tissues.
Treatment Duration
Brachytherapy typically requires fewer sessions and is usually done in one or a few visits. HDR brachytherapy, for example, can be completed in just a few minutes. External radiation therapy generally involves daily treatments over several weeks, making it more time-consuming.
Side Effects
Brachytherapy tends to have fewer side effects because the radiation is more focused on the tumor. Some patients may experience mild pain, swelling, or irritation, but these are usually temporary. External radiation can cause more widespread side effects, such as skin irritation, fatigue, or damage to nearby organs, especially if the treatment area is large.
Michalski et al. (2023, J Clin Oncol) found that adding EBRT to brachytherapy (COMBO) did not improve 5-year freedom from progression (FFP) compared to brachytherapy (BT) alone for intermediate-risk prostate cancer (FFP-ASTRO: 85.6% vs 82.7%; FFP-Phoenix: 88.0% vs 85.5%). However, COMBO significantly increased late grade 2+ (42.8% vs 25.8%, P < .0001) and grade 3+ (8.2% vs 3.8%, P = .006) genitourinary/gastrointestinal toxicities. The authors suggest BT alone is a standard treatment option for this group.
Effectiveness
Both treatments are highly effective, but brachytherapy is often preferred for cancers that are localized, like prostate, cervical, or breast cancer, because it targets the tumor precisely. External radiation therapy is better for larger or more widespread tumors. In some cases, both treatments may be used together for better results.
Gerard et al. (2023, Lancet Gastroenterol Hepatol) found that a contact x-ray brachytherapy boost with neoadjuvant chemoradiotherapy significantly improved 3-year organ preservation rates (81% vs 59%, p=0.0026) for early rectal cancer compared to an external beam radiotherapy boost. This benefit was more pronounced for tumors <3 cm (97% vs 63%, p=0.012). While early grade 2-3 adverse events were similar, late grade 1-2 rectal bleeding was more frequent in the brachytherapy boost group. The authors suggest this approach is a valuable organ preservation option.
Read OncoDaily’s Special Article About Radiation Oncologists
Innovations in Brachytherapy
Recent advancements in brachytherapy are improving its precision and effectiveness, making it a more powerful tool in cancer treatment.
Real-time Imaging
The use of MRI, CT, and ultrasound in brachytherapy is revolutionizing treatment by providing real-time images during the procedure. This allows doctors to place radioactive sources with pinpoint accuracy, reducing complications and ensuring radiation is delivered precisely to the tumor, sparing healthy tissues.
New Isotopes
New isotopes with better radiation delivery profiles, longer half-lives, and reduced side effects are enhancing brachytherapy. These advanced materials allow for more effective and efficient treatment, improving tumor control while minimizing risks to surrounding tissues.
3D-Printed Applicators
The development of 3D-printed patient-specific applicators is a game-changer. These custom-made tools are designed to fit each patient’s anatomy perfectly, optimizing radiation delivery and improving treatment precision. This ensures that the radiation dose is accurately targeted to the tumor.
Artificial Intelligence
AI is transforming brachytherapy by streamlining treatment planning. It helps optimize dose distribution, reducing preparation times and improving overall treatment efficiency. AI can analyze complex data quickly, ensuring the best treatment plan for each patient.
Brachytherapy and Immunotherapy
Emerging studies suggest that brachytherapy might stimulate immune responses, enhancing the body’s ability to fight cancer. When combined with immunotherapy, brachytherapy may work synergistically to boost treatment effectiveness and reduce the risk of recurrence.
How Much Does Brachytherapy Cost?
The cost of brachytherapy can vary widely, typically ranging from $5,000 to $20,000 depending on several factors. The price is influenced by the type of brachytherapy being used (HDR or LDR), the type of cancer being treated, the healthcare facility, and the geographic location. For example, HDR brachytherapy may cost less than LDR because it requires fewer sessions.
Insurance coverage also plays a major role. Many insurance plans, including Medicare, cover brachytherapy for approved cancer treatments, but the patient’s out-of-pocket costs can vary depending on the plan and any deductibles or copayments.
Stanberry et al. (2025, Nature) reviewed economic evaluations of low-dose-rate brachytherapy (LDR-BT) for localized and locally advanced prostate cancer (PCa). Among 14 included studies, LDR-BT was often the most cost-effective radiation therapy (in 75% of relevant studies), more so than radical prostatectomy (in 67%), and sometimes more than active surveillance (in 60%). LDR-BT was consistently more cost-effective than high-dose-rate brachytherapy (in 100% of comparisons) and was the least costly active treatment in 50% of studies. The authors conclude LDR-BT offers significant cost advantages in PCa care.
Recovery of the Body After Brachytherapy
After brachytherapy, recovery generally involves a few important steps to ensure healing and monitor for any side effects. In the first few days, patients are typically advised to rest and avoid strenuous activities. Light activities like walking may be okay, but heavy lifting, exercise, or strenuous movements should be avoided until the doctor clears you.
Side effects can vary depending on the area treated. For prostate cancer, common side effects may include urinary discomfort, bowel issues, or mild fatigue. For other cancers, such as cervical or breast cancer, there may be localized pain, swelling, or skin irritation. Managing these side effects often includes pain relief medication, staying hydrated, and following proper hygiene to avoid infections.
Patients should watch for signs that require medical attention, such as severe pain, heavy bleeding, fever, or difficulty breathing, as these could indicate complications. Any unusual symptoms should be reported to the healthcare team immediately.
Written by Nare Hovhannisyan, MD
FAQ
Can brachytherapy be used as a standalone treatment?
Yes, brachytherapy can be used alone, especially for localized cancers like prostate or cervical cancer. It may also be combined with other treatments, such as surgery or external radiation, depending on the case.
What precautions should patients take after brachytherapy?
Patients should avoid heavy lifting and strenuous activities for a few weeks. It's also important to follow hygiene practices, manage side effects like pain, and attend follow-up appointments for monitoring.
How does brachytherapy affect fertility?
Brachytherapy can impact fertility, especially in men (e.g., prostate cancer treatment) or women (e.g., cervical cancer treatment), as it may damage reproductive organs. Patients should discuss fertility preservation options before starting treatment if concerned.
Can brachytherapy be repeated if cancer returns?
Yes, in some cases, brachytherapy can be repeated if cancer returns, but this depends on the tumor's location, size, and previous treatments. A doctor will evaluate the best course of action for each individual situation.
What side effects should patients expect after brachytherapy?
Common side effects of brachytherapy include fatigue, urinary problems (e.g., frequent urination or discomfort), and pain or swelling at the treatment site. Some patients may also experience changes in bowel habits, sexual dysfunction, or skin irritation. These side effects usually improve over time, but patients should inform their healthcare provider of any persistent or severe symptoms.
How long does it take to recover from brachytherapy?
Recovery times vary depending on the individual and the area being treated. Most patients can resume normal activities within a few weeks, though some may need more time to recover fully. Regular follow-up visits will help monitor the recovery process and manage any lingering side effects.
Is brachytherapy safe?
Brachytherapy is generally considered safe, but like any medical treatment, it carries some risks. The treatment involves radiation, so there are potential side effects and complications, such as tissue damage or infection. However, when performed by a skilled medical team, the risks are minimized, and the benefits outweigh the potential downsides for many patients
How does brachytherapy differ from external radiation therapy?
Brachytherapy involves placing a radioactive source directly inside or very close to the tumor, delivering concentrated radiation to the affected area. External radiation therapy, on the other hand, involves directing radiation from outside the body to the cancer site. Brachytherapy allows for a more targeted treatment, often resulting in fewer side effects compared to external radiation.
Can brachytherapy be used for all types of cancer?
Brachytherapy is not suitable for all cancers. It is most commonly used for localized cancers, such as prostate, cervical, breast, and some head and neck cancers. It is not typically used for cancers that have spread or for those located in hard-to-reach areas.