Brachytherapy for cervical cancer is a key treatment option, which is the fourth most common cancer among women worldwide. In the United States alone, the National Cancer Institute reported approximately 14,480 new diagnoses in 2021. Radiation therapy, a common and effective approach to treating this disease, can be administered externally or internally. When delivered internally, it is specifically referred to as brachytherapy.
What is Brachytherapy?
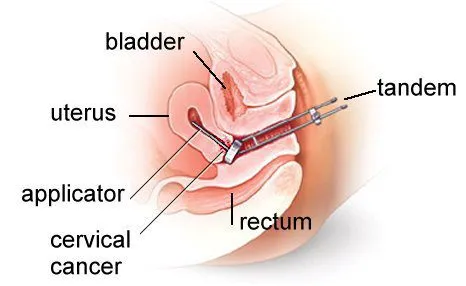
Brachytherapy is a type of internal radiation therapy where tiny radioactive sources are placed directly inside or near a tumor. This precise placement allows for high-dose radiation to target cancer cells while minimizing exposure to surrounding healthy tissues. By delivering radiation from within, brachytherapy ensures a more focused and effective treatment, reducing side effects and preserving nearby organs.
How Does Brachytherapy Work?
Brachytherapy works by placing tiny radioactive sources, such as seeds, wires, or discs, directly inside or near the tumor. These sources emit radiation over a set period, delivering high doses precisely to cancer cells while sparing healthy tissue. Depending on the type of cancer and treatment plan, the radiation may be delivered temporarily or permanently. Temporary brachytherapy involves placing the radioactive material for a short time before removal, while permanent brachytherapy leaves tiny seeds in place, gradually releasing radiation until they become inactive. This targeted approach ensures effective cancer treatment with minimal side effects.
source: www.aaro.sg
Main Types of Brachytherapy
Brachytherapy comes in two main forms: High-Dose-Rate (HDR) and Low-Dose-Rate (LDR), both designed to deliver radiation directly to tumors while sparing healthy tissue.
High-Dose-Rate (HDR) Brachytherapy
HDR uses a powerful radioactive source temporarily placed inside or near the tumor through applicators. The source is removed after each short session, with treatments often done on an outpatient basis. It’s commonly used for cervical, breast, prostate, and lung cancers. HDR offers precise targeting, shorter treatment times, and faster recovery.
Low-Dose-Rate (LDR) Brachytherapy
LDR involves implanting small radioactive seeds that release radiation slowly over time—days, weeks, or even permanently. It’s frequently used for prostate cancer, and sometimes for gynecologic or head and neck cancers. The seeds remain in the body, gradually losing activity, and allow patients to maintain normal routines with minimal disruption.
What to Expect During Brachytherapy for Cervical Cancer?
Before the procedure, doctors use imaging scans like CT, MRI, or ultrasound to carefully plan where to place the radioactive sources. Depending on the type of treatment, anesthesia or sedation may be used for comfort. The medical team explains the process and answers any concerns, like whether radiation will stay in the body permanently or if the procedure will be painful.
Once positioned, the treatment begins. In HDR brachytherapy, thin tubes or applicators are placed near or inside the tumor, delivering radiation for a few minutes before removal. LDR brachytherapy involves implanting tiny radioactive seeds that release radiation gradually over time. The radiation itself cannot be felt, and the procedure is designed to be quick and effective. HDR sessions are usually outpatient, while LDR may require a short hospital stay.
Most HDR patients go home the same day, while LDR patients may stay briefly for monitoring. Some mild swelling, discomfort, or fatigue may occur but usually fades quickly. If permanent seeds were implanted, doctors provide simple guidelines, such as temporary precautions around small children and pregnant women. Follow-up visits help track progress and ensure the treatment is working as expected.
How Effective Is Brachytherapy For Cervical Cancer?
Studies show that adding brachytherapy to EBRT significantly improves outcomes:
- A 2017 study found that tumor remission occurred in 92.5% of patients who received both EBRT and brachytherapy, compared to 73.3% with EBRT alone.
- Five-year survival rates were also higher (68.5% vs. 35.4%).
- In a 2021 study of patients with metastatic cervical cancer, brachytherapy significantly improved overall survival.
Brachytherapy For Cervical Cancer Side Effects: What Should You Expect?
Short-Term Side Effects
Most short-term side effects of brachytherapy are localized to the pelvic area, particularly the cervix and vagina. Common symptoms include vaginal or vulvar irritation, discharge, and pelvic discomfort. In addition, patients may experience general side effects from radiation, such as fatigue, nausea or vomiting, diarrhea, bladder irritation, and low blood counts.
Managing Short-Term Side Effects
These symptoms can often be managed with medications to relieve pain, nausea, or bowel discomfort. It’s important to get plenty of rest, stay hydrated, and avoid potential irritants like perfumed soaps or tight-fitting undergarments. If you’re experiencing stomach upset, eating bland or gentle foods can help reduce discomfort.
Long-Term Risks and Complications
Like other forms of cancer treatment, brachytherapy may lead to long-term side effects that appear months or even years after treatment. These may include vaginal stenosis, which is the narrowing and scarring of the vaginal canal, as well as vaginal dryness. Some patients may develop rectal stenosis or radiation cystitis, which is irritation of the bladder. In certain cases, lymphedema—or swelling in the legs caused by lymph fluid buildup—can also occur.
How Does Brachytherapy for Cervical Cancer Affect Sexual Health and Fertility?
Brachytherapy for cervical cancer can affect both sexual health and fertility, but the extent varies depending on the type of treatment, dose, and individual response.
Sexual Health
Brachytherapy may cause vaginal dryness, narrowing (stenosis), or tissue scarring due to radiation. These changes can lead to discomfort or pain during intercourse. Some women also experience decreased libido or emotional changes related to body image and intimacy. To help manage these effects, doctors often recommend vaginal dilators, lubricants, or pelvic floor therapy. Open communication with a partner and support from a counselor or sexual health specialist can also be helpful.
Zomkowski et al. (2016) in Archives of Gynecology and Obstetrics evaluated the short-term impact of high-dose rate brachytherapy on quality of life and sexual function in 20 gynecological cancer patients. They found a significant worsening in loss of appetite (p=0.002) and diarrhea (p=0.045), while constipation improved (p=0.013). Regarding sexual function, only lubrication significantly decreased (p=0.046) among the nine women who were sexually active before and after treatment.
Fertility
Fertility is often affected because radiation to the pelvic area can damage the ovaries, uterus, or both. In many cases, especially when brachytherapy is combined with external beam radiation, the ability to become pregnant naturally is lost. For younger women who wish to preserve fertility, options like egg or embryo freezing (before treatment) can be discussed, although fertility preservation is more challenging once treatment has started.
Read OncoDaily’s Special Article About Brachytherapy
How Much Does Brachytherapy Cost For Cervical Cancer?
The cost of brachytherapy for cervical cancer can vary widely depending on several factors, including geographic location. In the United States, a full course of treatment, which often includes multiple insertions and imaging, typically ranges from $10,000 to over $40,000. In Europe, costs range from €5,000 to €25,000, depending on the country and healthcare system. In India and Southeast Asia, prices are significantly lower, typically between $1,000 and $5,000 due to lower medical costs. In the Middle East and Africa, prices vary widely, with private hospitals generally being more expensive than public facilities.
Several factors influence the cost, such as whether the treatment is done in a public or private hospital, whether high-dose rate (HDR) or low-dose rate (LDR) brachytherapy is used, and the number of sessions, which is usually three to five for cervical cancer. Additional costs may include anesthesia, operating room time, hospitalization, and the use of imaging like MRI or CT scans. Insurance coverage or national cancer programs also vary by country and can significantly affect out-of-pocket expenses.
For example, in the U.S., a typical HDR brachytherapy plan for cervical cancer involving three to five fractions may cost about $5,000 to $8,000 per session, totaling around $20,000 to $35,000. Fortunately, brachytherapy is usually covered by insurance and national health systems when medically indicated, though out-of-pocket costs will depend on the specific insurance policies or co-payment structures in each country.
Recovery of the Body After Brachytherapy for Cervical Cancer
Recovery after brachytherapy for cervical cancer typically involves a gradual return to normal activities while allowing the body time to heal. In the first few days following treatment, rest is important. Patients are generally encouraged to avoid strenuous activities such as heavy lifting, vigorous exercise, or sexual intercourse until cleared by their healthcare provider. Light walking is usually acceptable and can help maintain circulation and energy levels.
Common side effects may include pelvic discomfort or cramping, mild vaginal bleeding or discharge, and fatigue. Some patients might also notice changes in urination or bowel habits, such as increased urgency, constipation, or diarrhea. These symptoms are often temporary and manageable. Pain relief medications can help ease discomfort, while staying hydrated and eating a balanced diet may support bowel and bladder function. Maintaining proper hygiene is also important to reduce the risk of infections, especially in the vaginal or urinary areas.
It’s essential to monitor for any signs of complications during recovery. These may include heavy or prolonged vaginal bleeding, a high fever, foul-smelling discharge, severe pelvic or abdominal pain, or difficulty urinating or passing stools. If any of these symptoms occur, patients should contact their healthcare team promptly. Regular follow-up appointments will help ensure that healing is progressing well and allow for early intervention if any issues arise.
Innovations in Brachytherapy For Cervical Cancer
Aghili et al. (2024) published in the Asian Pacific Journal of Cancer Prevention investigated the efficiency and safety of shortening brachytherapy duration to one week compared to three weeks in 49 locally advanced cervical cancer patients. The study found no significant difference in complete response rates, with 96.1% in the short-course group and 95.6% in the conventional group (p > 0.05). Furthermore, no difference in acute toxicity was observed between the groups, suggesting short-course brachytherapy is non-inferior and could reduce overall treatment time and costs.
Lu et al. (2024) published in Radiation Oncology evaluated the efficacy and safety of 3D-printed brachytherapy versus free-hand implantation in 50 cervical cancer patients. They found that 3D-printed brachytherapy significantly improved safety, especially for large tumors, by providing more precise dose distribution and reducing radiation to critical organs. Notably, the 3D-printed group had a significantly lower incidence of radiation enteritis (29.2%) compared to the free-hand group (88%, p<0.001). Short-term therapeutic response and overall survival were comparable between the two groups.
How Can Patients Support Their Health During Brachytherapy?
During brachytherapy for cervical cancer, patients can take several steps to support their overall health and well-being. It’s important to attend all scheduled appointments, follow pre- and post-treatment instructions, and report any unusual symptoms. Staying in close communication with the care team helps ensure the treatment is as safe and effective as possible.
Side effects like fatigue, vaginal discomfort, or mild bladder and bowel irritation may occur. Drinking plenty of fluids, eating light and nourishing meals, and using recommended creams or medications can help manage these symptoms. In some cases, using a vaginal dilator may be advised to maintain vaginal health after treatment.
Getting enough rest and focusing on a balanced diet with fruits, vegetables, lean proteins, and whole grains supports recovery. Staying hydrated and avoiding alcohol or smoking can also make a positive difference. Emotional well-being matters too. Brachytherapy can be overwhelming, and it helps to talk to a counselor, join a support group, or simply share thoughts and feelings with someone trusted.
Gentle movement like walking or stretching can improve energy levels and mood, as long as it’s approved by the care team. Throughout the process, patients should feel empowered to ask questions about any concerns, including pain, fertility, or intimacy. Advocating for one’s needs can make a big difference in how supported and informed a patient feels during treatment.
Written by Nare Hovhannisyan, MD
FAQ
How many sessions of brachytherapy do you need for cervical cancer?
The number of sessions a person requires depends on their cancer and the type of brachytherapy. They may require two treatments per day for 2–5 days or one treatment per week for 2–5 weeks.
Does brachytherapy cure cervical cancer?
Yes, brachytherapy can cure cervical cancer
How does brachytherapy affect fertility?
Brachytherapy can impact fertility, especially in men (e.g., prostate cancer treatment) or women (e.g., cervical cancer treatment), as it may damage reproductive organs. Patients should discuss fertility preservation options before starting treatment if concerned.
How does brachytherapy work for cervical cancer?
Brachytherapy delivers high doses of radiation directly to the tumor inside the cervix through an applicator, which minimizes damage to surrounding healthy tissues and improves treatment effectiveness.
How long does a brachytherapy session last?
The procedure typically takes 20–30 minutes for HDR brachytherapy. The time may vary depending on the type of therapy, imaging needed, and the number of sessions.
Can I go home after brachytherapy treatment?
For HDR brachytherapy, patients usually return home the same day after the procedure, as it is an outpatient treatment. For LDR brachytherapy, a hospital stay may be required for 1–3 days, depending on the type and extent of treatment.
Is brachytherapy the only treatment for cervical cancer?
No, brachytherapy is often used as part of a combination treatment plan. It's usually combined with external beam radiation therapy (EBRT) and sometimes chemotherapy. Surgery may also be considered, depending on the stage and type of cancer
Is brachytherapy effective for all stages of cervical cancer?
Brachytherapy is most effective for locally advanced cervical cancer (stages IB2 to IVA), especially in cases where the tumor has not spread extensively outside the pelvis. It may also be used as a treatment option in recurrent cancer.
How long after brachytherapy will I start feeling better?
Recovery varies from person to person. Most patients feel some fatigue and discomfort for a few weeks after treatment. It’s common to feel better within a few weeks to a couple of months as your body adjusts. Side effects like vaginal discharge or cramping typically subside after treatment.
Is brachytherapy painful?
Brachytherapy itself is usually not painful, as local anesthesia or sedation is used during the procedure to minimize discomfort. However, you may experience some post-treatment cramping or vaginal discomfort afterward, which can typically be managed with pain relief as advised by your doctor.