What is Parathyroid Cancer?
Parathyroid cancer is a rare endocrine malignancy that originates in the parathyroid glands, which are small, pea-sized glands located near the thyroid gland in the neck. These glands are responsible for regulating calcium levels in the blood through the secretion of parathyroid hormone (PTH). Parathyroid cancer is characterized by the uncontrolled growth of malignant cells within one or more of these glands, leading to hypercalcemia, a condition marked by elevated calcium levels in the blood. Parathyroid cancer typically presents with symptoms of hyperparathyroidism, such as hypercalcemia, which can lead to severe complications including bone pain, fractures, kidney stones, and neurological issues.
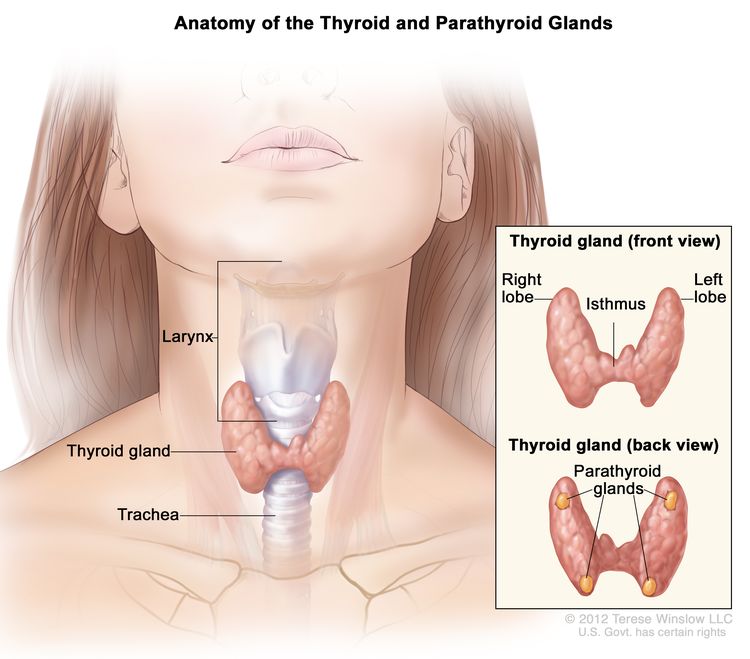
The image is taken from the National Cancer Institute website.
Prevalence and Epidemiology
Parathyroid cancer is extremely rare, accounting for approximately 0.005% of all cancers and 0.5% to 1% of all cases of hyperparathyroidism. The annual incidence is estimated to be around 3.5 to 5.7 cases per 10 million people. It affects men and women equally and is most commonly diagnosed in individuals over the age of 30, with a higher prevalence in those in their 40s and 50s.
Causes and Risk Factors
The exact cause of parathyroid cancer is unknown, but several risk factors have been identified. These include:
- Genetic Mutations: Mutations in the CDC73 gene (encodes a tumor suppressor protein involved in regulating cell growth and division, and its mutations can lead to cancer by allowing uncontrolled cell proliferation) are strongly associated with parathyroid cancer. Conditions such as hyperparathyroidism-jaw tumor (HPT-JT) syndrome and familial isolated hyperparathyroidism (FIHP) are linked to an increased risk of developing parathyroid cancer.
- Radiation Exposure: Exposure to radiation, particularly therapeutic radiation to the head and neck region, has been associated with an increased risk of parathyroid cancer.
- Age and Gender: Parathyroid cancer is more common in individuals over the age of 40, and there is a slightly higher incidence in males compared to females.
- Inherited Conditions: Multiple endocrine neoplasia type 1 (MEN1) and type 2 (MEN2) are hereditary conditions that increase the risk of developing parathyroid tumors, although MEN-related tumors are typically benign.
Symptoms
The symptoms of parathyroid cancer are primarily caused by hypercalcemia and can affect various parts of the body. Common symptoms include:
- General Symptoms: Fatigue, weakness, nausea, vomiting, loss of appetite, weight loss, and increased thirst and urination.
- Bone-Related Symptoms: Bone pain, fractures, and osteoporosis due to the excessive release of calcium from bones.
- Kidney-Related Symptoms: Kidney stones, kidney pain, and potential kidney failure due to high calcium levels.
- Gastrointestinal Symptoms: Abdominal pain, constipation, and indigestion.
- Neurological Symptoms: Confusion, difficulty thinking clearly, depression, and insomnia.
- Other Symptoms: A lump in the neck, hoarseness, and difficulty swallowing.
Diagnosis
Diagnosing parathyroid cancer can be challenging due to its rarity and the similarity of its symptoms to those of benign parathyroid conditions. The diagnostic process typically involves:
- Health History and Physical Exam: A thorough review of the patient’s medical history and a physical examination to check for lumps in the neck and other signs of hyperparathyroidism and hypercalcemia.
- Blood Tests: Measurement of calcium and PTH levels in the blood. Elevated levels of calcium (greater than 14 mg/dL) and PTH (5 to 10 times higher than normal) may indicate parathyroid cancer.
- Imaging Tests: Ultrasound, CT scans, and sestamibi (Technetium 99m) scans are used to locate abnormal parathyroid glands and assess the extent of the disease.
- Biopsy: In some cases, a biopsy may be performed to confirm the diagnosis, although distinguishing between benign and malignant parathyroid tumors can be difficult.
Treatment
The primary treatment for parathyroid cancer is surgery, intending to completely remove the tumor. Treatment options include:
Surgery
- En Bloc Resection: This is the primary and most effective surgical approach for parathyroid cancer. It involves removing the entire tumor along with surrounding tissues as one unit (en bloc) to ensure clear surgical margins and complete removal of the cancer. This may include removing part of the thyroid gland, muscles, and lymph nodes near the tumor.
- Neck Dissection (Lymphadenectomy): If imaging tests or examination during surgery suggest that the cancer has spread to lymph nodes in the neck, a neck dissection may be performed to remove those lymph nodes.
- Debulking Surgery: In cases where the entire tumor cannot be removed due to its extent or location, debulking surgery may be performed to remove as much of the cancerous tissue as possible. This can help reduce symptoms caused by excess parathyroid hormone and calcium levels.
Radiation Therapy
Radiation therapy alone is generally not effective for treating parathyroid cancer, as these tumors are not very radiosensitive. However, it may be used in the following situations:
- After surgery (adjuvant radiation therapy) to kill any remaining cancer cells and reduce the risk of recurrence, especially if surgical margins were positive for cancer cells.
- For unresectable or recurrent disease that cannot be surgically removed.
- To treat bone metastases and provide palliative relief from symptoms.
Chemotherapy
Chemotherapy has limited effectiveness in Parathyroid cancer and may be used in cases of metastatic or recurrent disease where surgery is not an option. Various chemotherapy drugs and combinations have been tested with varying success rates.
Treatment for Hypercalcemia
Controlling high calcium levels (hypercalcemia) caused by excess parathyroid hormone is a crucial part of treatment. Options include:
- Intravenous fluids to increase calcium excretion
- Bisphosphonates like pamidronate or zoledronic acid to inhibit bone resorption
- Calcitonin to reduce calcium levels
- Calcimimetics like cinacalcet to lower parathyroid hormone levels
- Denosumab to inhibit bone resorption
- Gallium nitrate
- Hemodialysis for severe, refractory hypercalcemia
The treatment approach is individualized based on the extent of the disease, the patient’s overall health, and the goals of care. Surgery remains the only potentially curative option, while other treatments aim to control symptoms and disease progression. Close monitoring is required, as recurrence rates are high even after initial surgical treatment.
Prognosis
The prognosis for parathyroid cancer varies widely and depends on several factors, including the stage at diagnosis, the completeness of surgical resection, and the presence of hypercalcemia. The 5-year survival rate* ranges from 50% to 80%, while the 10-year survival rate ranges from 15% to 66%. Early diagnosis and complete surgical removal of the tumor are critical for improving prognosis. Recurrence is common, and the disease often returns within 2 to 5 years after the initial surgery. Hypercalcemia, if not adequately managed, is a significant cause of morbidity and mortality in patients with parathyroid cancer.
*The survival rate is the percentage of people who are still alive after a certain period of time following a diagnosis or treatment for a disease.

A section of a right hemithyroidectomy specimen reveals a classic intrathyroidal parathyroid adenoma, surrounded by a rim of thyroid tissue encircling the tumor. The image is taken from a paper by Sadacharan et al. (2015).
Patient Survivorship
Survivorship care is an essential aspect of managing parathyroid cancer. It involves regular follow-up visits to monitor for recurrence, manage long-term side effects, and address any ongoing health issues. Key components of survivorship care include:
- Regular Monitoring: Blood tests to check calcium and PTH levels, and imaging tests to detect any signs of recurrence.
- Management of Long-Term Side Effects: Addressing issues such as hypocalcemia, bone health, and potential complications from surgery.
- Supportive Care: Providing emotional and psychological support, as well as resources for managing the impact of cancer on daily life.
Problems During and After Treatment and How to Manage Them
- Hypocalcemia: Hypocalcemia, or low calcium levels in the blood, is common in the first few days after parathyroid surgery. Symptoms include tingling or numbness in the fingers or around the mouth, and in severe cases, muscle spasms or tetany. Management involves calcium and vitamin D supplementation. Patients may need to take oral calcium supplements, and in severe cases, intravenous calcium may be required. Monitoring serum calcium levels regularly is essential to adjust the dosage of supplements.
- Surgical Complications: Surgery for parathyroid cancer can lead to several complications. Bleeding is a potential risk, especially given the proximity of the parathyroid glands to large blood vessels. Hematomas, or blood clots under the skin, can occur but are usually minor and resolve on their own. In rare cases, a second operation may be needed to stop bleeding and remove the clot. Infection at the surgical site is uncommon but can be managed with antibiotics if it occurs. Scarring, including hypertrophic or keloid scars, may develop, particularly in patients with a predisposition to such conditions. Proper wound care and, in some cases, steroid injections can help manage scarring.
- Recurrent Laryngeal Nerve Injury: Damage to the recurrent laryngeal nerve during surgery can cause hoarseness, voice changes, and difficulty swallowing. This nerve controls the vocal cords and is at risk during parathyroid surgery due to its proximity to the glands. Most cases of nerve injury are temporary, but permanent damage can occur. Voice therapy with a speech-language pathologist can help improve voice function and coping strategies. In severe cases, surgical interventions such as vocal cord injections or medialization thyroplasty may be necessary.
- Hungry Bone Syndrome: Hungry bone syndrome occurs when the bones rapidly take up calcium from the blood after the removal of a hyperactive parathyroid gland, leading to severe hypocalcemia. This condition is more common in patients with long-standing hyperparathyroidism and significant bone disease. Management involves aggressive calcium and vitamin D supplementation, and in some cases, intravenous calcium infusions may be required. Regular monitoring of calcium levels is crucial to adjust treatment and prevent complications.
- Emotional and Psychological Support: A cancer diagnosis and treatment can have a significant emotional and psychological impact. Patients may experience anxiety, depression, and fear of recurrence. Supportive care includes counseling and mental health support to help patients cope with these challenges. Support groups and connecting with other patients and survivors can provide emotional support and shared experiences. Educational resources about the disease, treatment options, and survivorship care are also beneficial.
Conclusion
Parathyroid cancer is a rare but serious condition that requires a comprehensive approach to diagnosis, treatment, and survivorship care. Early detection and complete surgical removal of the tumor are critical for improving prognosis. Managing hypercalcemia and addressing the emotional and psychological impact of the disease are also essential components of care. By staying informed and working closely with their healthcare team, patients with parathyroid cancer can achieve better outcomes and maintain a good quality of life.
Sources
- Parathyroid Cancer – National Cancer Institute
- Parathyroid Cancer – American Society of Clinical Oncology
- Parathyroid Cancer Treatment – Canadian Cancer Society
- Parathyroid Cancer: A Review – Cancers
- Parathyroid carcinoma: Current management and outcomes – A systematic review – American Journal of Otolaryngology
- Parathyroid Cancer – American Association for Cancer Research