Retinoblastoma is a rare eye cancer that usually develops in children before 5 years of age. It forms in the retina, the light-sensitive tissue at the back of the eye that allows us to see. Retinoblastoma may affect one eye (unilateral) or both eyes (bilateral). In about two-thirds of cases, only one eye is involved.
With early diagnosis and modern treatment, survival in developed countries exceeds 95%, making early detection extremely important.
Prevalence and Demographics
Globally, retinoblastoma affects approximately 1 in 15,000–20,000 children, with an estimated 8,600 to 9,000 new cases each year. Around 90% of cases occur in low- and middle-income countries, largely due to higher birth rates and larger young populations.
In developed countries such as the United States and Europe, retinoblastoma accounts for about 3% of childhood cancers, while in some developing regions it may represent more than 10% of pediatric cancers. The overall sex distribution is relatively balanced, although slight male predominance has been reported in certain age groups.

Types of Retinoblastoma: Heritable and Sporadic
Retinoblastoma occurs in two main forms: heritable and sporadic.
Heritable Retinoblastoma
Heritable retinoblastoma is caused by a germline mutation in the RB1 gene. This means the mutation is present in all cells of the body and may be passed from parent to child. Children with this form often develop tumors in both eyes and are typically diagnosed at a younger age.
Because the RB1 mutation exists throughout the body, these children have an increased lifetime risk of developing other cancers, including bone tumors (osteosarcoma), soft tissue sarcomas, melanoma, and certain brain tumors. A small number may develop tumors in the pineal gland, sometimes referred to as trilateral retinoblastoma.
Screening for Cancer in Children with Hereditary Retinoblastoma
Children with a known RB1 mutation or family history require close monitoring. Eye examinations usually begin soon after birth and are performed every one to two months during infancy, becoming less frequent over time. After five years of age, visits often transition to annual examinations.
Brain MRI is commonly recommended during early childhood to monitor for rare pineal tumors. MRI is preferred over CT scans because it avoids radiation exposure. Families should also remain alert for unexplained lumps, persistent pain, or unusual symptoms that require medical evaluation.
Prenatal Testing
Families with a known RB1 mutation may consider genetic counseling. Preimplantation genetic testing (PGT), performed alongside IVF, allows embryos to be tested for a known RB1 mutation before implantation.
During pregnancy, testing can be performed using chorionic villus sampling (CVS) in the first trimester or amniocentesis in the second trimester. These procedures carry small risks and should be discussed with a specialist.
Sporadic Retinoblastoma
Most cases of retinoblastoma are sporadic. In these children, mutations in the RB1 gene occur only in retinal cells after conception and are not inherited from a parent.
Sporadic retinoblastoma typically affects one eye and is usually diagnosed slightly later than hereditary disease, often around two years of age. Because the mutation is not present in all body cells, these children generally do not have the same increased risk of secondary cancers and do not pass the condition to future children.
Even in unilateral cases, genetic testing is recommended to determine whether a germline mutation is present.
Symptoms
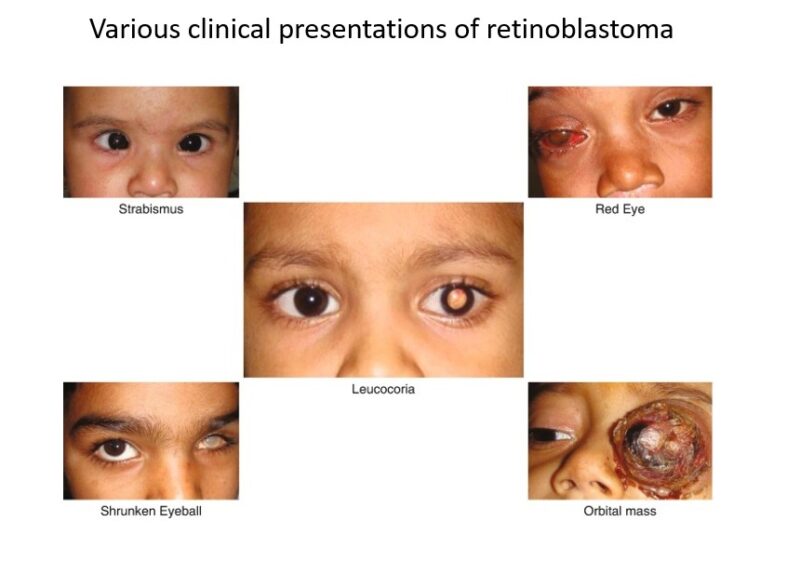
The most common sign of retinoblastoma is leukocoria, which appears as a white reflection in the pupil. Parents often notice this in flash photographs. Another frequent symptom is strabismus, where one eye does not align properly with the other.
Children may also show signs of poor vision, clumsiness, eye redness, or swelling. Less common symptoms include eye pain, changes in iris color, or an enlarged pupil. In advanced cases, the eye may appear larger or cloudy. If cancer spreads beyond the eye, symptoms such as headaches, vomiting, weight loss, or bone pain may occur, although this is rare in countries with early diagnosis.
Prompt medical evaluation is essential if any of these symptoms are observed.
Causes
Retinoblastoma develops due to mutations in the RB1 gene, a tumor suppressor gene that regulates cell growth. Normally, RB1 helps control the cell cycle and prevents uncontrolled cell division. When both copies of the gene are inactivated, retinal cells can grow rapidly and form tumors.
In hereditary cases, one mutation is inherited and the second develops later. In sporadic cases, both mutations occur only within retinal cells. There is no strong evidence linking environmental exposures to the development of retinoblastoma.
Diagnosis
Diagnosis involves clinical examination and imaging.
Clinical Examination
- Physical Examination: Evaluation for leukocoria, strabismus, and other abnormalities.
- Examination Under Anesthesia: Allows detailed retinal assessment in young children.
- Examination: Tumors typically appear as white or cream-colored retinal masses.
Imaging Tests
- Ultrasound: Confirms the presence of an intraocular mass and detects calcifications.
- MRI: Preferred imaging method to assess optic nerve involvement and extraocular spread. MRI is favored over CT to avoid radiation exposure.
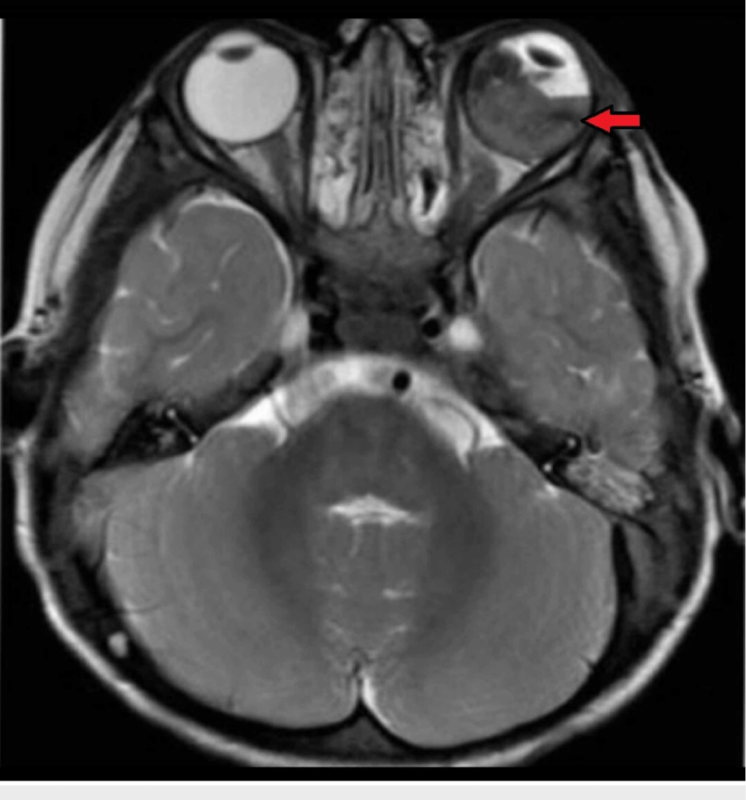
Axial T2-weighted MRI of the brain and orbit showing retinoblastoma in the left eye along with retinal detachment (red arrow)
- CT Scan: Rarely used today because of radiation risks, especially in hereditary cases.
- Fundus Photography: Documents tumor appearance and monitors response to treatment.
Additional Diagnostic Tests
- Fluorescein Angiography
- Optical Coherence Tomography (OCT)
Genetic Testing
All children with retinoblastoma should undergo RB1 genetic testing to determine whether the disease is hereditary.
Biopsy
Biopsy is generally avoided due to the risk of spreading tumor cells.
Importance of Early Detection
Early detection significantly improves survival and the likelihood of preserving vision. Parents are often the first to notice leukocoria. Routine pediatric checkups also play an important role in identifying early signs. Rapid referral to a pediatric ophthalmologist is critical.
Treatment
Treatment depends on tumor size, location, and genetic type.
Standard Treatment Modalities
- Chemotherapy
- Systemic Chemotherapy: Shrinks tumors using vincristine, etoposide, and carboplatin.
Intra-Arterial Chemotherapy (IAC): Delivers chemotherapy directly to the ophthalmic artery. This method has significantly improved eye salvage rates while reducing systemic toxicity.
Intravitreal Chemotherapy: Used for vitreous seeding.
Local Therapies
- Cryotherapy
- Laser therapy (thermotherapy)
- Brachytherapy
Enucleation
Removal of the eye is performed when tumors are very large or vision cannot be preserved. When done early, it is highly effective at curing intraocular disease.
Recent Advances
Research is ongoing into targeted therapies, immunotherapy approaches (including GD2-targeted antibodies), and novel drug delivery systems such as suprachoroidal injections and nanoparticle-based treatments. These remain investigational in 2026.
Multidisciplinary Approach
Care involves pediatric oncologists, ophthalmologists, radiation specialists, and genetic counselors. Treatment plans are individualized.
Prognosis
In high-income countries, survival approaches 100% for intraocular disease. Prognosis depends on stage at diagnosis and whether cancer has spread outside the eye.
Three staging systems are commonly used:
- International Classification for Intraocular Retinoblastoma
- Reese-Ellsworth classification
- TNM staging system
Lower-stage disease is associated with better outcomes and higher likelihood of preserving vision.
Watch the survival story of Rubi
Patient’s Survivorship
Survivors of retinoblastoma, particularly those with hereditary disease, may face long-term health risks. These include second primary cancers, especially in individuals who received radiation therapy. Vision impairment is common depending on tumor location and treatment type.
Some children may experience cataracts or other treatment-related effects. Psychological support may also be necessary, as vision changes and cancer treatment can affect emotional well-being and social development.
Lifelong follow-up care is recommended. Children who undergo enucleation require properly fitted prosthetic eyes that are adjusted as they grow. Protective eyewear and regular specialist visits remain important parts of long-term care.
Watch the video, in which Carol L. Shields, MD, Co-Director of the Wills Eye Oncology Service in Philadelphia discusses Retinoblastoma
References and Useful Resources
Clinicaltrials.gov – a huge database of clinical trials, useful for patients and families to find past, ongoing, and upcoming clinical trials.
Cancer.Net – Comprehensive information for people with cancer, families, and caregivers, from the American Society of Clinical Oncology (ASCO)
Cancer.Gov – More comprehensive overview on the treatment of retinoblastoma by NCI
Chop.edu – Children’s Hospital of Philadelphia
Cancer.org – American Cancer Society
Oncodaily.com – Online platform where you can find anything related to cancer such as everyday news, blogs, videos, podcasts, etc.