Ablation therapy is a type of minimally invasive cancer treatment that works by destroying cancer cells in place, rather than surgically removing them. Instead of cutting out a tumor, doctors use special tools to deliver energy—such as extreme heat, cold, or electrical pulses—directly to the cancerous tissue. This energy damages the cancer cells, causing them to break down and die over time, while sparing as much of the surrounding healthy tissue as possible.
In this article, we’ll explore the main types of ablation therapy, explain how they work, discuss when and why they are used, and cover their benefits, risks, and what patients can expect before, during, and after treatment. Whether you’re a patient or simply want to understand this evolving approach to cancer care, this guide will provide a clear and accessible overview.
How Does Ablation Therapy Work?
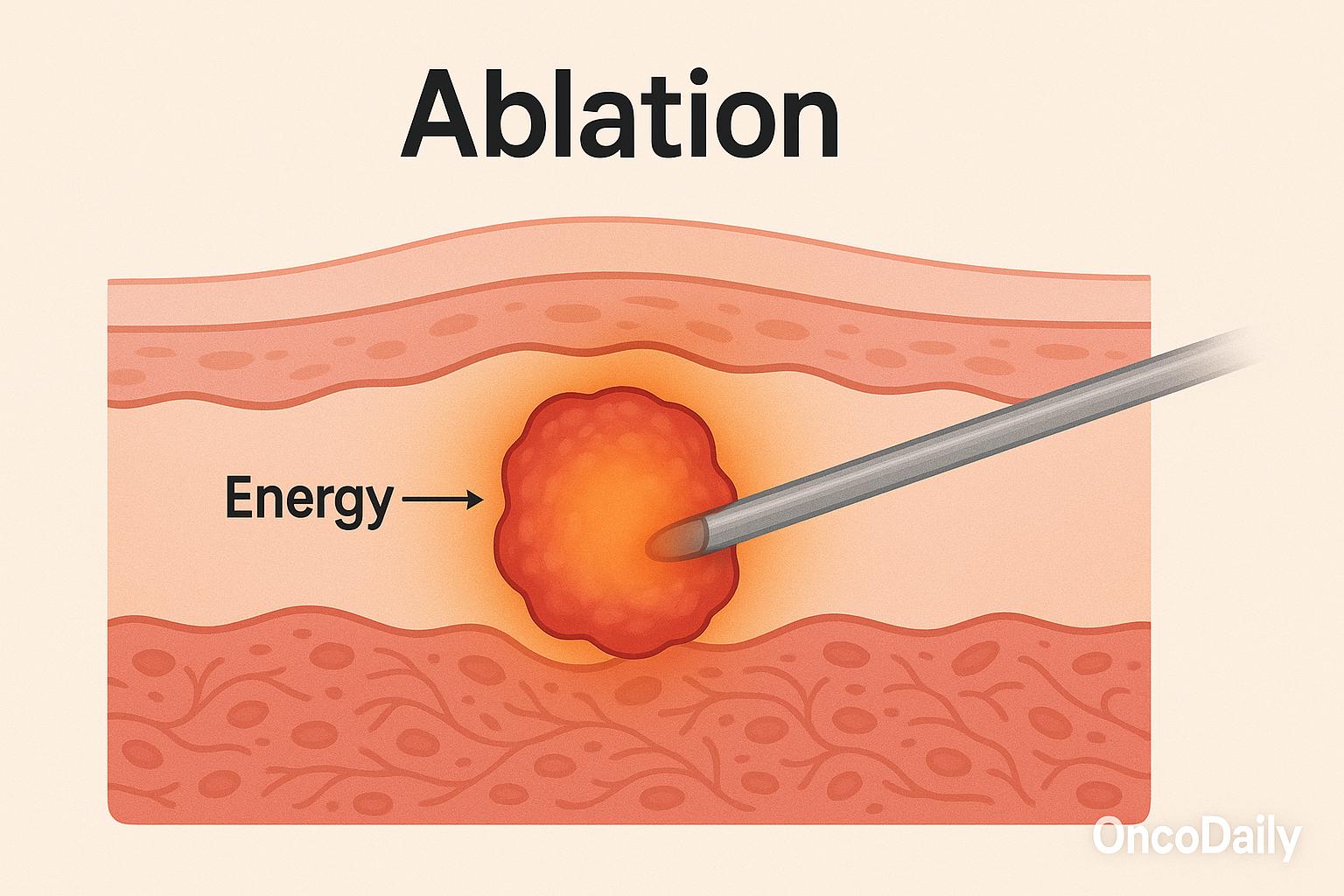
Ablation therapy works by directly targeting the tumor, focusing energy precisely where it’s needed. To ensure accuracy, the procedure is almost always done under real-time imaging guidance—such as CT scans, ultrasound, or MRI. These imaging tools allow doctors to visualize the exact location of the tumor and guide a thin needle or probe into place. Once the probe reaches the tumor, it delivers heat (as in radiofrequency or microwave ablation), cold (as in cryoablation), or other forms of energy, depending on the type of ablation used. The goal is to destroy the cancer cells locally, while doing as little harm as possible to the surrounding healthy tissue.
Most ablation procedures are performed percutaneously, meaning the probe is inserted through the skin with no need for large surgical incisions. These treatments are typically carried out by interventional radiologists, specialists trained to perform minimally invasive procedures using imaging guidance. In some cases, especially for tumors that are hard to reach or close to vital structures, ablation may also be done during laparoscopic or open surgery. This precise, focused approach makes ablation a valuable option for treating small tumors and managing cancer in patients who may not tolerate major surgery.
Types of Ablation Therapy
There are several different types of ablation therapy, each using a specific kind of energy to destroy cancer cells. The choice depends on the tumor’s size, location, and type, as well as the patient’s overall condition. Below are the most commonly used techniques:
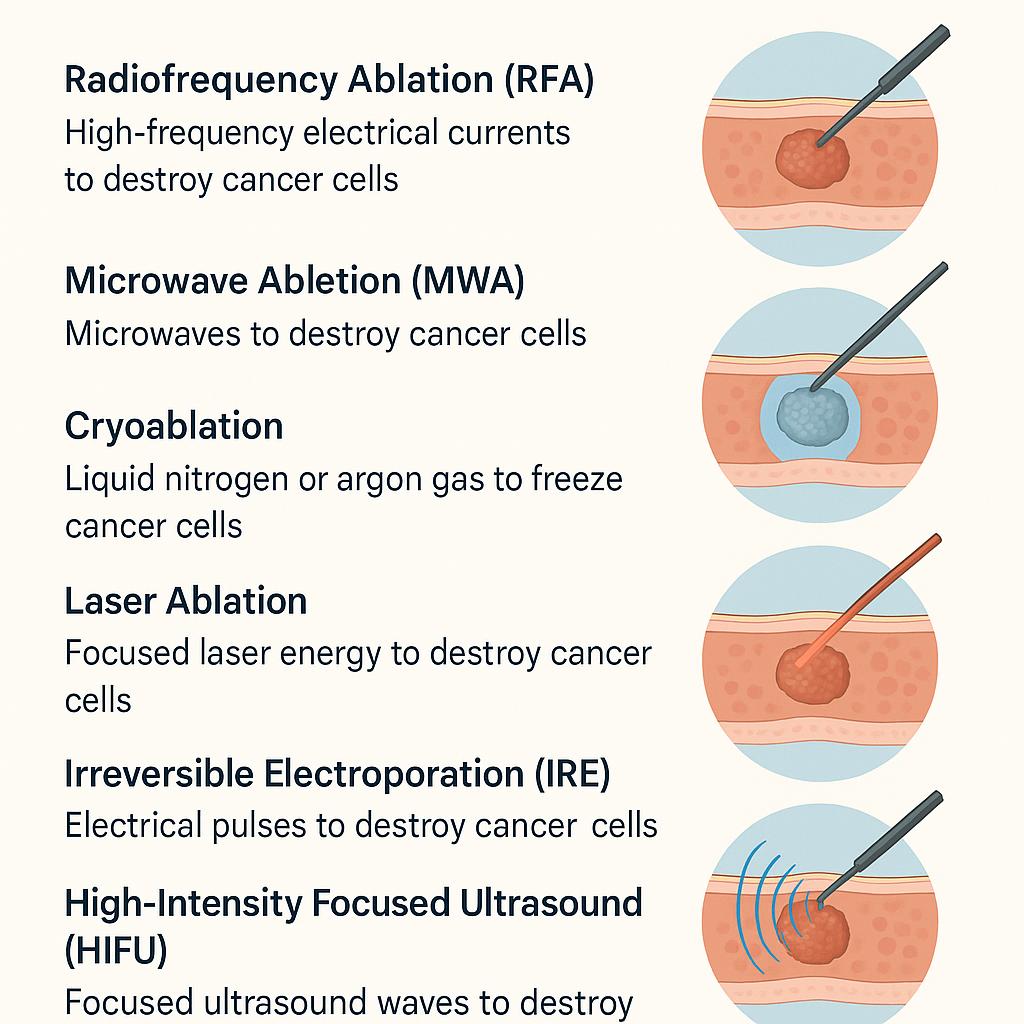
Radiofrequency Ablation (RFA) is one of the most established methods. It works by sending high-frequency electrical currents through a needle-like probe, creating heat that destroys cancer cells. RFA is commonly used for tumors in the liver, kidneys, and lungs, especially when surgery isn’t an option. Microwave Ablation (MWA) operates on a similar principle but uses microwaves instead of electrical currents to produce heat. It can often heat tissue more rapidly and effectively than RFA, making it a good option for larger tumorsor areas where time is critical.
Cryoablation takes a very different approach—rather than heating the tumor, it freezes it. This is done by inserting a probe that circulates liquid nitrogen or argon gas, forming ice crystals inside the cancer cells and destroying them. Cryoablation is frequently used for prostate, kidney, and lung cancers and can be visually monitored during the procedure with imaging to assess the ice ball’s extent. Laser Ablation uses focused laser energy to heat and destroy cancer cells. It is sometimes used for brain tumors and other sensitive areas where precise control is essential.
Irreversible Electroporation (IRE) is a newer technique that doesn’t rely on temperature at all. Instead, it uses short bursts of electrical pulses to disrupt cancer cell membranes, causing them to die while sparing nearby blood vessels and other critical structures. This makes IRE particularly useful near delicate tissues. High-Intensity Focused Ultrasound (HIFU) is a non-invasive method that focuses ultrasound waves to heat and destroy targeted tissue deep within the body. It is still under investigation for many cancers but is already being used in select cases, such as prostate cancer.
Each of these techniques has its strengths and limitations, and doctors carefully evaluate which approach is best suited for each individual case.
When Is Ablation Therapy Used?
Ablation therapy is most often used for early-stage tumors, particularly those that are less than 3 to 5 centimeters in size. These tumors may be located in organs such as the liver, kidneys, or lungs, and are often treated with ablation when surgical removal is not possible—either because of their location or because the patient has other health issues that make surgery too risky. It’s also a valuable option for patients with comorbidities—such as heart or lung disease—who might not tolerate major surgery or anesthesia well. Since ablation is minimally invasive, it offers a safer alternative for individuals who are otherwise not good candidates for traditional surgical approaches.
Another growing use of ablation is in oligometastatic disease, where the cancer has spread but only to a limited number of sites. For example, ablation can be used to target a few metastatic tumors in the liver or lung, helping to control disease without the need for systemic therapy alone. In some cases, ablation is used palliatively, not to cure the cancer, but to relieve symptoms. For example, it can help reduce pain, bleeding, or pressure caused by tumors pressing on other organs or tissues. In this setting, ablation may greatly improve comfort and quality of life, even when the disease is advanced.
Benefits of Ablation Therapy
Ablation therapy offers several advantages, especially for patients who may not be ideal candidates for traditional surgery. One of the most significant benefits is that it is minimally invasive, usually performed through a small incision or needle puncture. This means that patients often experience shorter recovery times, less postoperative pain, and fewer complications compared to major surgery.
Many ablation procedures are done on an outpatient basis or require only a brief hospital stay, allowing patients to return home and resume normal activities much sooner. This makes the treatment particularly attractive to older adults or individuals with other medical conditions who may face higher risks with conventional surgery or general anesthesia. Another advantage is that ablation can often preserve organ function, which is especially important when treating tumors in organs like the liver, kidneys, or lungs. By targeting only the tumor and sparing surrounding healthy tissue, ablation helps maintain the overall health of the organ.
Ablation is also a repeatable procedure. If a tumor recurs or if new lesions appear in the same area, the treatment can often be performed again without significantly increasing risk. This flexibility makes it a valuable tool in long-term cancer management, particularly for those with chronic or slowly progressing disease.
Risks and Limitations
While ablation therapy offers many benefits, it’s important to understand that it’s not suitable for all patients or all types of cancer. One of the main limitations is tumor size and location—ablation is generally most effective for small tumors(typically less than 3–5 cm) that are clearly visible and accessible using imaging guidance. Tumors that are large, located near critical blood vessels, nerves, or other sensitive structures may be harder to treat safely with ablation.
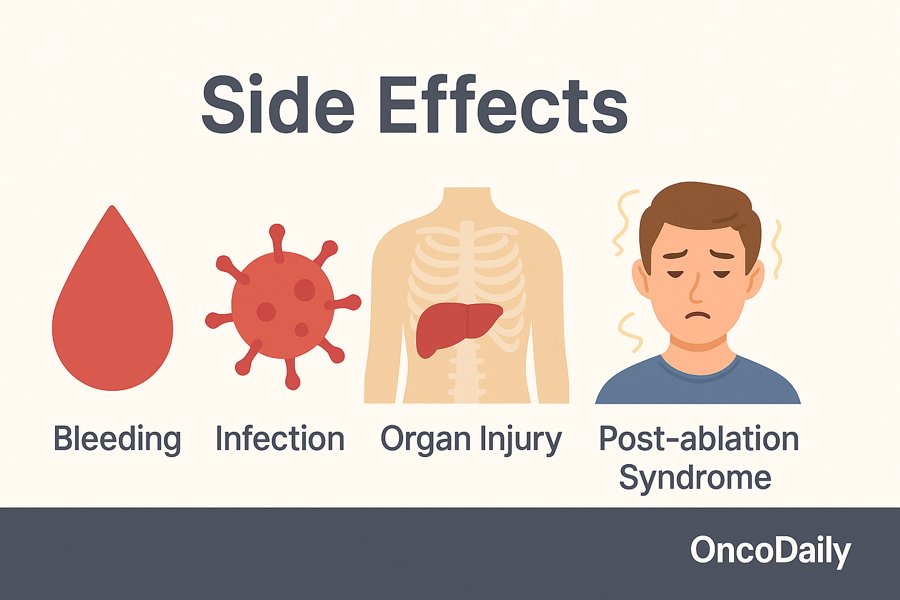
As with any procedure, there are potential side effects and complications. These may include bleeding, infection, or unintended injury to nearby organs or tissues. Some patients experience a temporary condition known as post-ablation syndrome, which causes flu-like symptoms such as fever, fatigue, and muscle aches for a few days after treatment. Another consideration is the risk of tumor recurrence. If the entire tumor is not successfully destroyed—particularly around the edges or margins—it may grow back. This is why precise imaging and experienced technique are so critical in achieving the best results.
Finally, while ablation can be highly effective for early-stage or localized disease, it is usually not curative for advanced or widely metastatic cancers. In these cases, ablation is often used as a palliative treatment or as part of a larger strategy to prolong survival and improve quality of life, rather than to eliminate cancer completely. Understanding these risks and limitations helps patients and their care teams make informed decisions about whether ablation therapy is the right option.
What to Expect During the Procedure
Ablation therapy is typically performed in a hospital or specialized outpatient setting and is guided by imaging, most often CT scans, ultrasound, or MRI. These imaging tools help the doctor pinpoint the exact location of the tumor to guide the placement of the treatment probe with precision.
The procedure usually involves local anesthesia to numb the area, and in some cases, sedation is given to help the patient relax. For deeper or more complex procedures, such as those near the lungs or liver, general anesthesia may be used to ensure comfort and safety. Once the patient is properly positioned and anesthetized, the doctor inserts a thin probe or needle through the skin and into the tumor. The energy—whether heat, cold, or electrical pulses—is then delivered through the probe to destroy the cancer cells. The entire treatment generally lasts between 30 to 90 minutes, depending on the size, number, and location of the tumors being treated.
After the procedure, most patients are monitored for a short time and then go home the same day or after an overnight stay, depending on the type of ablation and individual health needs. Recovery is usually quick, with many people resuming normal activities within a few days. Some may experience mild discomfort, fatigue, or flu-like symptoms, but these usually resolve on their own.
Outcomes and Effectiveness
Ablation therapy has become a valuable tool in the cancer treatment arsenal, particularly for achieving high local control rates, especially in small, well-defined tumors. When used in the right setting, it can destroy tumors effectively and with minimal impact on surrounding tissues. Clinical studies have shown that in carefully selected patients, ablation can lead to good progression-free survival—meaning the cancer remains stable without growing or spreading for a significant period of time.
Because ablation is typically a local treatment, it is often combined with systemic therapies such as chemotherapy or immunotherapy, which target cancer cells throughout the body. This integrated approach allows doctors to control both local and distant disease more effectively, offering patients a better chance of long-term disease management. While ablation may not be curative for everyone, especially in the case of widespread or aggressive cancers, it can play a crucial role in controlling tumors, preserving organ function, and improving quality of life. As technology and techniques continue to improve, the role of ablation therapy in personalized cancer care is expected to expand even further.
You Can Watch More on OncoDaily Youtube TV
Written by Toma Oganezova, MD
Ablation therapy is a minimally invasive procedure that destroys cancer cells using heat, cold, or electrical energy without surgical removal. Common types include radiofrequency ablation (RFA), microwave ablation (MWA), cryoablation, laser ablation, irreversible electroporation (IRE), and high-intensity focused ultrasound (HIFU). It is used for small, early-stage tumors, patients who cannot undergo surgery, or to treat a limited number of metastases (oligometastatic disease). Most procedures are done under local anesthesia or sedation. Discomfort is minimal, and recovery is usually fast. Possible risks include bleeding, infection, injury to nearby organs, and tumor recurrence if the ablation isn’t complete. When used appropriately, ablation can achieve high local tumor control rates, especially in small tumors, and is often combined with systemic therapy. Yes, one advantage of ablation is that it can be repeated in the same area if needed, making it suitable for ongoing cancer management. Most patients resume normal activities within a few days. Some may feel mild fatigue or flu-like symptoms temporarily.FAQ
What is ablation therapy?
What types of ablation are used in cancer treatment?
When is ablation therapy recommended?
Is ablation therapy painful?
What are the risks of ablation therapy?
How effective is tumor ablation?
Can ablation be repeated if the tumor returns?
What’s the recovery time after ablation?