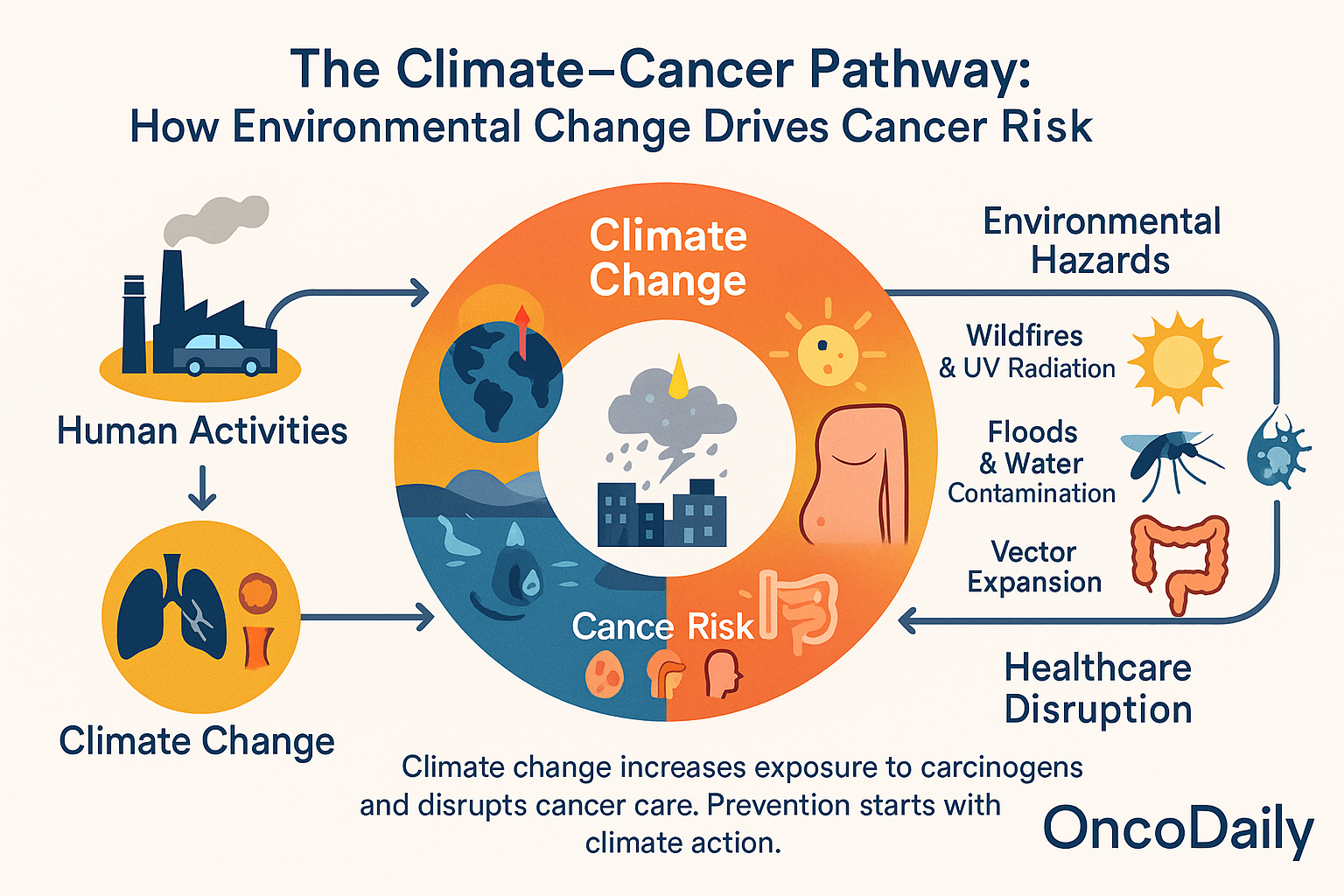
Climate change is increasingly recognized as a significant factor influencing global health, including cancer patterns. Rising temperatures, air pollution, and extreme weather events linked to climate change are altering exposure to cancer risk factors and disrupting healthcare systems essential for cancer prevention, diagnosis, and treatment. Recent studies, such as those focused on the Middle East and North Africa, reveal that higher ambient temperatures correlate with increased incidence and mortality rates of cancers like breast, ovarian, uterine, and cervical cancers among women. Additionally, climate-driven factors such as wildfires and fossil fuel combustion release carcinogens that elevate risks for lung, skin, and gastrointestinal cancers.

This topic explores how shifting environments due to climate change influence cancer epidemiology through multiple pathways: increased exposure to carcinogens, disruption of healthcare delivery, and biological effects of heat and pollution at the cellular level. It also examines geographic variations in cancer risk linked to climate factors and the compounding effects of environmental toxins and healthcare access challenges.
This article focuses on the mechanisms connecting climate change and cancer, evidence from recent research, and the urgent need for integrating climate resilience into public health and cancer control strategies.
How Is Climate Change Influencing Cancer Risk?
Pollution: The Unseen Carcinogen
Climate change amplifies air pollution through increased wildfires, fossil fuel combustion, and dust storms. These events release a cocktail of carcinogens including benzene, formaldehyde, and polycyclic aromatic hydrocarbons (PAHs) into the air. Chronic exposure to these pollutants is linked to higher rates of lung, bladder, and gastrointestinal cancers. Wildfire smoke, in particular, can travel vast distances, affecting populations far from the source and compounding cancer risk.
Heatwaves and Temperature Extremes: More Than Just Discomfort
Rising temperatures do more than cause heatstroke. Extreme heat increases the formation of ground-level ozone and other pollutants, which are associated with elevated cancer risks. Heatwaves also strain healthcare systems, making cancer care less accessible during critical periods. For patients undergoing chemotherapy or radiation, disruptions in treatment can have life-threatening consequences.
Ultraviolet Radiation: A Growing Skin Cancer Threat
Ozone depletion and altered cloud cover due to climate change can increase exposure to ultraviolet (UV) radiation. This raises the risk of melanoma and other skin cancers, particularly in regions unaccustomed to high UV levels. As sun exposure patterns shift, so too does the global burden of skin cancer.
Water and Food Insecurity: Hidden Pathways to Cancer
Floods and droughts, both intensified by climate change, can contaminate water supplies with heavy metals, pesticides, and industrial chemicals many of which are known carcinogens. Food insecurity may force populations to rely on preserved or processed foods, which can carry additional cancer risks due to additives and contaminants.
Vector-Borne Diseases: Indirect Cancer Risks
Climate-driven shifts in the range of insects such as mosquitoes can increase the transmission of viruses linked to cancer, including human papillomavirus (HPV) and hepatitis B and C. These infections are major causes of cervical, liver, and other cancers, especially in regions with limited access to vaccination and screening.
Who Is Most at Risk? Disparities and Vulnerabilities
Low- and middle-income countries often lack the resources to adapt to environmental changes or manage disruptions in cancer care, which leads to higher mortality rates. Urban populations are more exposed to air pollution and heat islands, further compounding cancer risks. Rural and marginalized communities may be cut off from care during disasters, which exacerbates existing health inequities. Additionally, children and the elderly are more sensitive to environmental toxins and disruptions in healthcare. Recent studies in the Middle East and North Africa show that higher temperatures are linked to increased incidence and mortality of breast, ovarian, uterine, and cervical cancers, particularly among women.
Are Certain Cancers on the Rise?
The evidence that certain cancers are on the rise in connection with climate change and environmental factors comes from multiple authoritative sources, combining epidemiological data, regional studies, and global cancer registries.
Lung and Respiratory Cancers: Impact of Pollution and Wildfires
A 2025 report highlights that climate change-fueled natural disasters such as wildfires and hurricanes increase exposure to lung carcinogens like polycyclic aromatic hydrocarbons (PAHs). For example, Hurricane Harvey in 2017 caused refinery damage that released carcinogens, increasing lung cancer risk in affected populations. Patients with lung cancer also face worsened outcomes when treatment is disrupted by such disasters. This shows both increased incidence and mortality linked indirectly to climate-related pollution and healthcare interruptions.
Rising Cancer Incidence in India and Globally
According to the National Cancer Registry Programme (NCRP) of India and Global Cancer Observatory (GLOBOCAN) data, cancer incidence is increasing steadily. India alone saw an estimated 1.46 million new cancer cases in 2022, projected to rise by 12.8% by 2025. Lung cancer accounted for approximately 103,371 cases in 2022, ranking among the top five cancers for both males and females. Globally, GLOBOCAN estimated 19.3 million new cancer cases in 2020, with projections rising sharply by 2040 due to demographic and environmental factors.
Breast and Women’s Cancers: Temperature Correlation in MENA Region
A 2022 study in the Middle East and North Africa (MENA) region found a statistically significant correlation between rising ambient temperatures and increased prevalence and mortality of breast, ovarian, cervical, and uterine cancers. The prevalence of these cancers rose by approximately 173 to 280 cases per 100,000 people for every additional degree Celsius increase in temperature, underscoring climate change as a risk amplifier for hormone-related cancers in women.
United States Cancer Trends: Increasing Incidence
The American Cancer Society’s 2025 report projects about 2,041,910 new cancer cases in the US, with invasive breast cancer expected to rise by about 1% annually since the mid-2000s. Lung cancer remains a leading cause of cancer death, with environmental factors such as air pollution and smoking contributing. The rising trend in breast cancer incidence, particularly among women under 50, is partially attributed to changing environmental and lifestyle risk factors.
Can Climate Change Disrupt Cancer Diagnosis and Treatment?
Climate change is increasing the frequency and severity of extreme weather events such as hurricanes, floods, heatwaves, and wildfires. These disasters pose significant challenges to healthcare infrastructure, particularly for cancer diagnosis and treatment, which require timely, continuous, and often complex care.
- Hospital and Clinic Damage: Flooding and storms can physically damage healthcare facilities, destroying diagnostic equipment like MRI and CT scanners, radiation therapy machines, and laboratory infrastructure. For example, Hurricane Katrina in 2005 led to the closure of several cancer treatment centers in New Orleans for months, delaying care for thousands of patients.
- Power Outages and Equipment Failures: Extreme weather often causes prolonged power outages, disrupting refrigeration of chemotherapy drugs and radiation equipment operation. Without reliable electricity, hospitals cannot maintain sterile environments or operate life-saving devices, forcing cancellations or postponements of treatments.
- Supply Chain Interruptions: Disasters can sever transportation routes, delaying or preventing delivery of essential medications, including chemotherapy agents, immunotherapies, and pain management drugs. This can lead to treatment interruptions that reduce effectiveness and increase the risk of cancer progression.
- Delayed or Missed Appointments: Patients may be unable to travel due to damaged roads, public transport shutdowns, or evacuation orders. This results in missed screenings, biopsies, and follow-up visits, causing cancers to be diagnosed at later, less treatable stages.
- Healthcare Workforce Strain: Medical staff themselves may be affected by disasters—displaced, injured, or overwhelmed leading to staffing shortages that further limit patient care capacity.
The cumulative effect of these disruptions can lead to increased cancer morbidity and mortality, as early detection and continuous treatment are critical for favorable outcomes.
Access Gaps and Inequities: Who Bears the Brunt?
The impact of climate-related healthcare disruptions is not evenly distributed. Vulnerable populations, particularly those in rural, remote, and low-resource settings, face amplified challenges:
- Rural and Isolated Areas: In many regions, cancer care is already centralized in urban centers. When disasters strike, transportation links such as roads and bridges may be damaged or destroyed, making it impossible for rural patients to reach oncology clinics or hospitals. Limited local healthcare infrastructure means few alternatives exist, resulting in prolonged treatment delays or abandonment.
- Socioeconomic Barriers: Low-income patients may lack private transportation or resources to relocate temporarily, compounding access problems during and after extreme weather events.
- Marginalized Communities: Ethnic minorities and socially disadvantaged groups often live in areas more prone to environmental hazards and have less access to quality healthcare, intensifying disparities in cancer outcomes.
What Does Science Say? Emerging Evidence
Recent scientific studies provide growing evidence that climate change is influencing cancer incidence and mortality across different regions.
Middle East & North Africa (MENA)
A 2025 study published in Frontiers in Public Health by researchers from the American University in Cairo analyzed data from 17 MENA countries over two decades. They found a strong correlation between rising ambient temperatures and increased rates of breast, ovarian, uterine, and cervical cancers among women. Specifically, each 1°C increase in temperature corresponded to an additional 173–280 cancer cases and 171–332 deaths per 100,000 women, highlighting climate change as a significant risk amplifier in this region.
North America
Environmental health reports and regional studies indicate that the increasing frequency of wildfires and heat waves both driven by climate change are linked to spikes in lung and skin cancers. Wildfire smoke contains carcinogenic particulate matter and polycyclic aromatic hydrocarbons (PAHs), while heatwaves elevate ground-level ozone, exacerbating respiratory and skin cancer risks.
Asia
Research from urban centers in China and India shows a rise in gastrointestinal and respiratory cancers associated with worsening air pollution from rapid urbanization and industrial emissions. Climate change intensifies heat and smog, worsening air quality and increasing exposure to carcinogens.
Feedback Loops: Pollution, Climate, and Cancer
The burning of fossil fuels fuels both climate change and air pollution, creating a vicious cycle. As temperatures rise, wildfires and smog events become more frequent, increasing carcinogen exposure and further accelerating climate change. This feedback loop underscores the urgent need for integrated policies targeting emissions reduction to mitigate both cancer and climate risks.
What Can Be Done? Solutions and Strategies
Building climate-resilient health systems involves several key strategies. First, it is essential to strengthen hospitals and clinics so they can withstand extreme weather events, ensuring that critical infrastructure remains operational during disasters. Preparedness is also crucial; developing comprehensive emergency plans helps maintain the continuity of cancer care and other essential health services when disruptions occur. Additionally, real-time surveillance systems should be established to monitor environmental exposures and track cancer trends, enabling timely responses to emerging threats.
Reducing pollution and emissions requires a multifaceted approach. Policy measures should focus on enforcing stricter air quality standards and investing in clean energy sources to minimize harmful emissions. At the community level, promoting the development of urban green spaces and reducing reliance on polluting vehicles can significantly improve air quality and public health.
Public awareness and education play a vital role in prevention and adaptation. Communities should be educated about ways to reduce exposure to environmental carcinogens, empowering individuals to make informed choices. Adaptation strategies, such as encouraging the use of sunscreen to protect against harmful UV radiation and promoting water filtration to ensure safe drinking water, help individuals adopt protective behaviors that reduce health risks associated with environmental changes. Cancer and climate change know no borders. International cooperation is essential to share data, resources, and strategies for both mitigation and adaptation.
Conclusion: The Urgency of Action
The intersection of cancer and climate change is a rapidly evolving field that demands immediate attention. As shifting environments alter exposure to carcinogens and disrupt healthcare, the global community must act to protect vulnerable populations and adapt cancer control strategies for a warming world. By understanding these complex links and taking proactive steps, we can help ensure a healthier future for all.
In this article, readers have discovered how the multiple ways climate change can influence
cancer risk and patterns, examining how environmental shifts may alter exposure to carcinogens, increase UV radiation, and exacerbate air pollution. It discusses which populations such as low-income communities, marginalized groups, and those in climate-vulnerable regions and which cancer types are most affected, including skin, lung, and gastrointestinal cancers. The piece also highlights how climate-related disruptions, such as extreme weather events and infrastructure damage, threaten the continuity and accessibility of cancer care.
Drawing on the latest scientific findings, it underscores the emerging connections between climate and cancer, and offers practical solutions to address these challenges. These include integrating climate resilience into healthcare systems, advancing targeted research, and implementing policies that prioritize both environmental sustainability and public health. The future of cancer prevention and care depends on our ability to adapt to a changing planet. The time to act is now.
Written by Marine Marashlian
FAQ
What is climate change?
Climate change refers to significant changes in global temperatures and weather patterns over time, primarily caused by human activities increasing greenhouse gas levels in the atmosphere.
Why is a degree or two change in average global temperature important?
Even small increases in average global temperature can lead to severe impacts such as more frequent extreme weather events, rising sea levels, and disruptions to ecosystems and human societies.
How does climate change affect people’s health?
Climate change affects health by increasing heat-related illnesses, worsening air quality (e.g., ozone pollution), expanding the range of disease-carrying insects, and causing extreme weather events that threaten lives and mental health.
How does climate change impact human health?
It increases risks of heat-related illnesses, respiratory diseases due to air pollution, vector-borne diseases like Lyme disease and West Nile virus, food and water insecurity, and mental health issues caused by extreme weather and displacement.
Who is most vulnerable to health effects from climate change?
Vulnerable groups include children, older adults, pregnant women, people with pre-existing health conditions, low-income communities, and those living in urban heat islands or rural areas with limited healthcare access.
How does climate change contribute to cancer risk?
Climate change increases exposure to environmental toxins, ultraviolet radiation, air pollution, and infectious agents, all of which can raise the risk of cancers such as lung, skin, and gastrointestinal cancers.
Which cancers are most affected by climate change?
Lung cancer (due to air pollution), skin cancer (due to increased UV radiation), and gastrointestinal cancers (due to disruptions in food and water supply) are expected to increase with climate change.
How does air pollution linked to climate change affect cancer rates?
Particulate matter from pollution is estimated to cause up to 15% of new lung cancer cases worldwide, with worsening air quality from climate impacts exacerbating this risk.
Can disruptions in food supply from climate change influence cancer?
Yes, changes in food availability and nutrition, such as reduced fruit and vegetable consumption, may increase nutrition-related cancers, contributing to hundreds of thousands of climate-related cancer deaths by 2050.
How might climate change affect cancer care and outcomes?
Extreme weather and climate disruptions can impair healthcare infrastructure and delivery, complicating cancer diagnosis, treatment, and care, potentially worsening cancer outcomes globally.