Breast cancer treatment has evolved significantly, with a growing emphasis on minimizing surgical interventions while maintaining oncologic safety. Sentinel lymph node biopsy (SLNB) has long been the standard approach for staging the axilla in clinically node-negative early-stage breast cancer, replacing more invasive axillary lymph node dissection (ALND). However, as evidence supporting de-escalation strategies grows, researchers have questioned whether SLNB is necessary for all patients, particularly those with small, low-risk tumors. The INSEMA (Intergroup Sentinel Mamma) trial aimed to address this by evaluating whether omitting SLNB impacts long-term invasive disease–free survival (IDFS) and patient outcomes, providing critical insights into the future of breast cancer surgery.
Title: Axillary Surgery in Breast Cancer — Primary Results of the INSEMA Trial
Authors:
Toralf Reimer, Ph.D., Angrit Stachs, Ph.D., Kristina Veselinovic, M.D., Thorsten Kühn, Ph.D., Jörg Heil, Ph.D., Silke Polata, M.D., Frederik Marmé, Ph.D., Thomas Müller, Ph.D, Guido Hildebrandt, Ph.D., David Krug, Ph.D., Beyhan Ataseven, Ph.D., Roland Reitsamer, Ph.D., Sylvia Ruth, M.D., Carsten Denkert, Ph.D., Inga Bekes, Ph.D., Dirk-Michael Zahm, M.D., Marc Thill, Ph.D., Michael Golatta, Ph.D., Johannes Holtschmidt, M.D., Michael Knauer, Ph.D., Valentina Nekljudova, Ph.D., Sibylle Loibl, Ph.D, and Bernd Gerber, Ph.D.
Published in NEJM, March 2025
Background
Axillary lymph node evaluation has been a fundamental component of early-stage breast cancer management, playing a critical role in staging and guiding decisions about adjuvant therapy. Traditionally, axillary lymph node dissection (ALND) was the gold standard for assessing nodal involvement, but it was associated with significant morbidity, including lymphedema, pain, restricted arm mobility, and sensory nerve damage. To reduce these complications, sentinel lymph node biopsy (SLNB) was introduced as a less invasive alternative, effectively identifying nodal metastases while minimizing postoperative morbidity.
SLNB has since become the standard of care for clinically node-negative breast cancer. However, with advancements in systemic therapy and improved imaging modalities, the necessity of SLNB in all patients has been questioned. Studies such as the ACOSOG Z0011 trial have demonstrated that for certain patients with limited sentinel node metastases, omitting ALND does not compromise survival outcomes. This has led to a broader discussion about whether SLNB itself can be omitted in selected patients with early-stage, small, clinically node-negative tumors, especially given the minimal impact of axillary surgery on overall survival in the modern era of breast cancer treatment.
The INSEMA (Intergroup Sentinel Mamma) trial was designed to evaluate whether skipping SLNB in patients with small, node-negative breast cancer would affect long-term outcomes. Specifically, it aimed to determine whether omitting SLNB compromises invasive disease–free survival (IDFS), while also assessing the impact on axillary recurrence rates, overall survival, and quality of life. Given the potential to reduce surgical interventions without affecting oncologic safety, the results of this trial could significantly influence future breast cancer treatment guidelines.
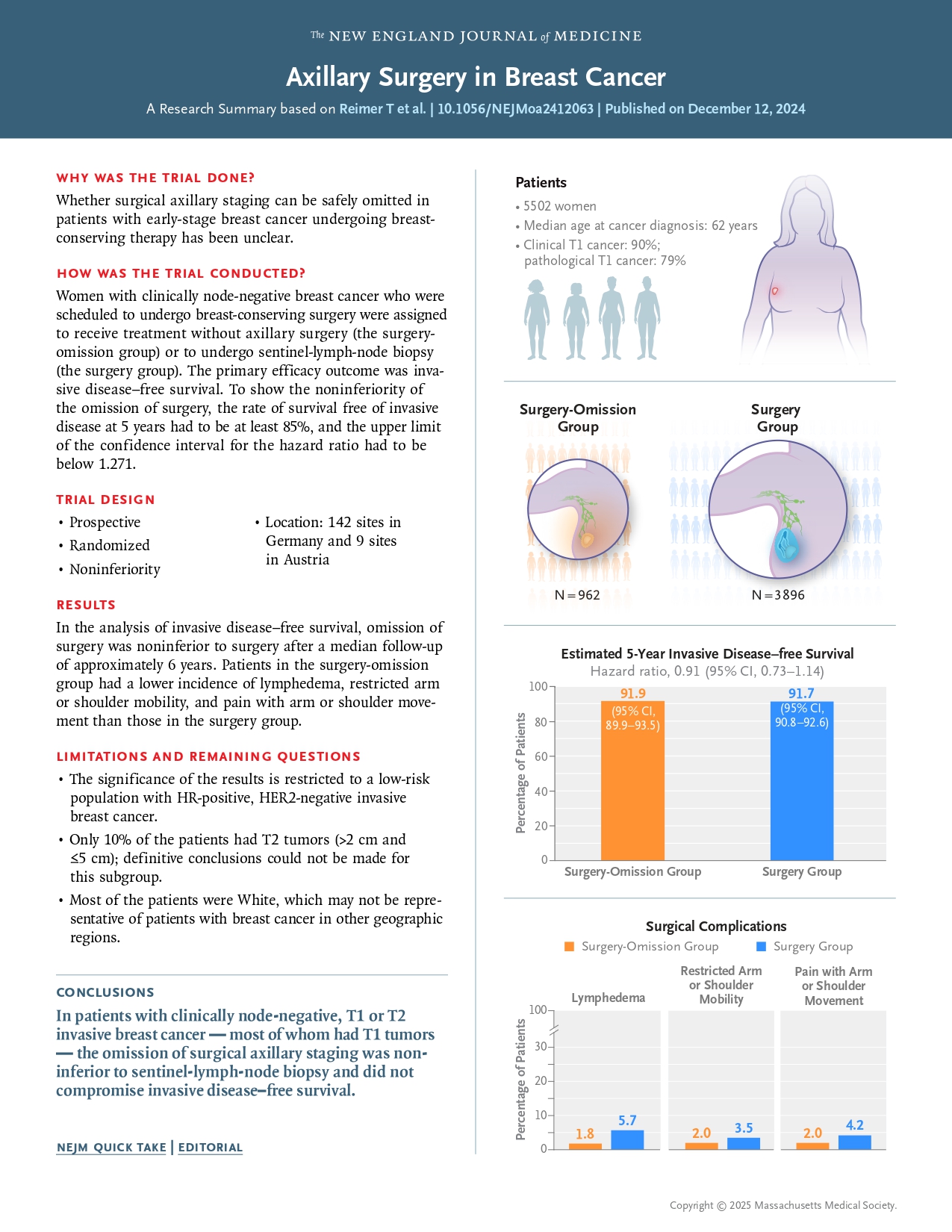
Study design and methods of INSEMA trial
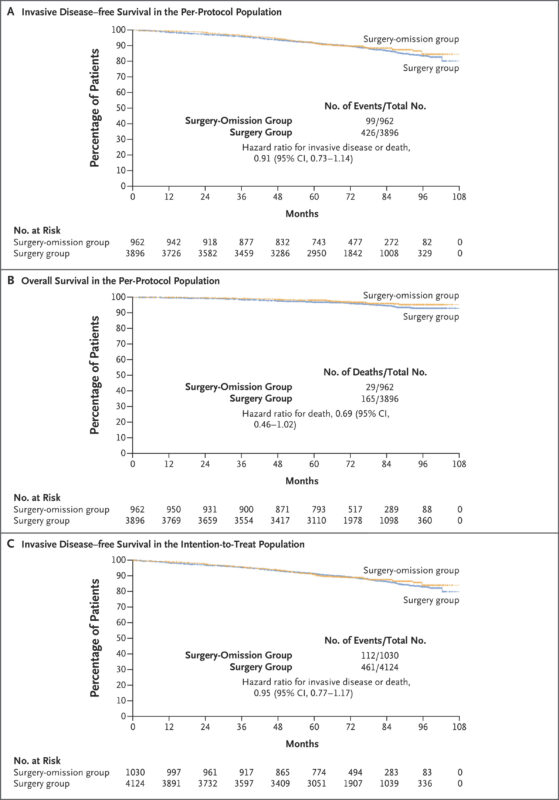
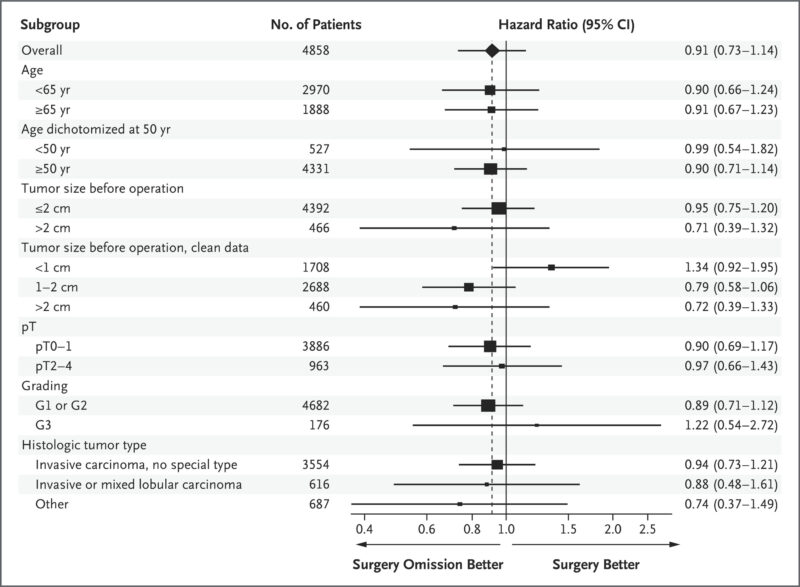
The INSEMA trial was a prospective, randomized, noninferiority study involving patients with clinically node-negative invasive breast cancer staged as T1 or T2 (tumor size ≤5 cm) scheduled for breast-conserving surgery. A total of 5,502 eligible patients were randomized in a 1:4 ratio: 962 patients were assigned to the surgery-omission group (no axillary surgery), and 3,896 to the surgery group (undergoing SLNB). The primary endpoint was the 5-year IDFS rate, with noninferiority defined by a 5-year IDFS rate of at least 85% and an upper confidence limit for the hazard ratio (HR) for invasive disease or death below 1.271.
Results of INSEMA trial
The INSEMA trial’s findings suggest that for selected patients with early-stage, clinically node-negative breast cancer, omitting SLNB does not adversely affect 5-year invasive disease–free survival and offers benefits in reducing surgical morbidity. These results support a more individualized approach to axillary management, potentially sparing patients from unnecessary procedures without compromising oncological outcomes
Survival and Recurrence Outcomes
- The 5-year IDFS rate was 91.9% (95% CI: 89.9–93.5) in the surgery-omission group and 91.7% (95% CI: 90.8–92.6) in the surgery group.
- The HR for invasive disease or death was 0.91 (95% CI: 0.73–1.14), meeting the pre-specified noninferiority criteria.
- Axillary recurrence rates were 1.0% in the surgery-omission group vs. 0.3% in the surgery group.
Survival and Mortality
- Overall mortality was 1.4% in the surgery-omission group and 2.4% in the surgery group.
- Distant recurrence rates remained low in both groups.
Quality of Life Outcomes
- Patients who skipped SLNB had less arm swelling (lymphedema), less pain, and better arm mobility than those who underwent SLNB.
- Overall, functional outcomes were superior in the surgery-omission group.
Key Findings
- Skipping SLNB did not compromise 5-year IDFS, supporting the safety of omission in selected early breast cancer patients.
- The slight increase in axillary recurrence (1.0% vs. 0.3%) did not translate into a higher mortality rate.
- Quality of life was significantly better in patients who avoided axillary surgery, with less lymphedema, pain, and better arm function.
- The findings challenge the necessity of routine SLNB in clinically node-negative breast cancer patients, advocating for a more individualized treatment approach.
Key Takeaway Messages
- Omitting SLNB in patients with clinically node-negative, small invasive breast cancers did not compromise 5-year IDFS.
- The slight increase in axillary recurrence rates in the surgery-omission group did not translate into higher mortality.
- Patients who avoided axillary surgery reported better arm mobility and less lymphedema, indicating improved quality of life.
You can read the full article here