At the heart of the 4th Scientific Meeting of the Pediatric Oncology East & Mediterranean (POEM) Group, a dedicated Retinoblastoma Workshop brought together leaders in pediatric oncology, ophthalmology, pathology, and public health. The workshop served as a powerful reminder of what is possible when science, system design, and compassion intersect—especially in addressing the needs of children with cancer in resource-constrained settings.
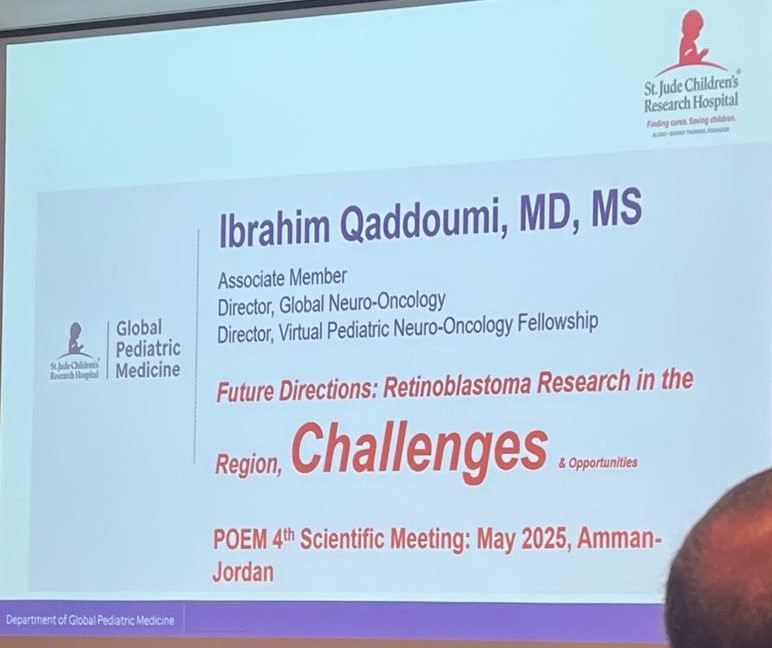
St. Jude Global: Reimagining Global Systems for Retinoblastoma Care
The session opened with a keynote by Dr. Matthew W. Wilson, Director of the St. Jude Global Retinoblastoma Program, who joined virtually. Dr. Wilson presented the vision of St. Jude Global in collaboration with the World Health Organization to close survival gaps in childhood cancer, particularly through strategic capacity building in retinoblastoma care.
He introduced the three-tiered referral model—local (micro), regional (meso), and international centers of excellence (macro)—designed to ensure patients can receive care aligned with available infrastructure.
The Global Retinoblastoma Academy was highlighted as a flagship training initiative, with over 50 countries represented in its 2025 cohort. Tools like the ARIA guidelines, the St. Jude Tumor Board Toolkit, and an interactive retinoblastoma board game were shared as innovations aimed at improving practical problem-solving and interdisciplinary learning in low-resource settings.
Clinical Detection and Diagnosis: A Matter of Timing
In a region where delayed diagnosis often costs both vision and lives, Dr. Muna Mohammad offered a sharp clinical perspective on retinoblastoma detection. She emphasized the importance of recognizing early signs—particularly leukocoria and strabismus – which are often seen first by caregivers and general practitioners.
She walked through the diagnostic workflow, highlighting the value of fundus photography (REDCAM), ultrasound, and MRI, while also stressing the need for early and accurate referral systems to ensure prompt intervention.
Pathology: The Hidden Pillar of Multidisciplinary Care
Dr. Maysa Al-Hussaini, histopathologist and acting chair at King Hussein Cancer Center, reminded the audience that diagnosis is not complete without expert pathology. In her talk, “Pathological Insights into Retinoblastoma”, she explained the technical challenges of specimen handling, processing, and analysis, including identification of rosettes, fleurettes, and high-risk features like choroidal invasion or optic nerve involvement.
Therapeutic Strategies: Evolving Evidence, Tailored Approaches
Dr. Hadeel Halalsheh, pediatric oncologist, provided a rigorous and detailed review of retinoblastoma treatment, walking the audience through the International Retinoblastoma Staging System and its implications on therapy choices.
She revisited the roles of systemic chemotherapy for both intraocular and metastatic disease, including protocols that incorporate topotecan and vincristine. Strategies such as chemoreduction, enucleation, radiotherapy, and autologous stem cell rescue were discussed in detail. Dr. Halalsheh emphasized that successful outcomes rely on a tightly integrated team—with pediatric oncologists, ophthalmologists, and pathologists collaborating at every step.
The Genetic Frontier: Risk Stratification and Family-Centered Care
Dr. Yacoub Yousef delved into the genetics of retinoblastoma, framing the disease not just as a tumor, but as a heritable predisposition with implications that extend across generations.
Dr. Yousef emphasized that RB1 gene testing plays a critical role in earlier diagnosis, reduction of treatment burden, and improved survival. However, recognizing that genetic testing is often unavailable in many regions, he introduced pragmatic screening protocols based on calculated family risk. His talk outlined risk-stratification models for bilateral and unilateral probands and shared data from a Jordanian cohort, which revealed:
- 50% of patients had bilateral disease
- 20% were from familial cases
- Screening resulted in earlier diagnosis and lower-stage presentation
He also addressed the challenges of examining under anesthesia (EUA) in low-risk children, emphasizing the importance of risk-guided screening to avoid unnecessary procedures while ensuring high-risk children are closely followed.
Dr. Yousef concluded with a discussion of genetic counseling, advocating for family education on the risk of second malignancies, the importance of early screening, and the psychological support needed for families navigating these risks.
A Unified Message: Early Detection, Equitable Systems, Shared Learning
As the workshop concluded, one theme echoed through every session: retinoblastoma is curable – but only when systems work together. From geneticists and pathologists to oncologists and health policymakers, each discipline holds a key to better outcomes.
Through initiatives like St. Jude Global, tools such as ARIA guidelines and tumor board kits, and the growing network of POEM collaborators, the international pediatric oncology community is demonstrating that partnership – not geography – should determine a child’s chance at life and sight.
Framing the Clinical Landscape of Retinoblastoma
Dr. Hadeel Halalsheh opened the workshop with introductory remarks and later delivered a talk on chemotherapy treatment approaches for retinoblastoma. As a key pediatric oncologist in the region, her session likely focused on systemic treatment strategies, their evolving role in multimodal therapy, and how chemotherapy is adapted in different resource settings. She may have also addressed challenges in toxicity management and treatment timing for improved ocular outcomes.
Bridging Global Gaps in Retinoblastoma Access
In his presentation on global perspectives and access to care, Dr. Mathew Wilson likely emphasized international disparities in early diagnosis, treatment availability, and outcomes for retinoblastoma. His discussion may have drawn on global health frameworks to illustrate how regional collaborations, telemedicine, and policy-level interventions can improve equity in care.
Foundations of Diagnosis in Retinoblastoma
Dr. Muna Mohammad presented on the diagnostic process for retinoblastoma, likely covering clinical signs such as leukocoria and strabismus, as well as the use of fundoscopy, ultrasound, and MRI. She may have emphasized the need for early referral and multidisciplinary coordination, especially in low-resource settings, where diagnostic delays can worsen prognosis.
Pathological Insights into Retinoblastoma
In her talk on pathology, Dr. Maysa Al-Hussaini likely addressed histopathologic hallmarks of retinoblastoma, risk stratification markers (e.g. optic nerve invasion), and the prognostic implications of enucleation specimens. Her insights may have helped bridge pathology with treatment decisions, particularly in cases requiring adjuvant therapy.
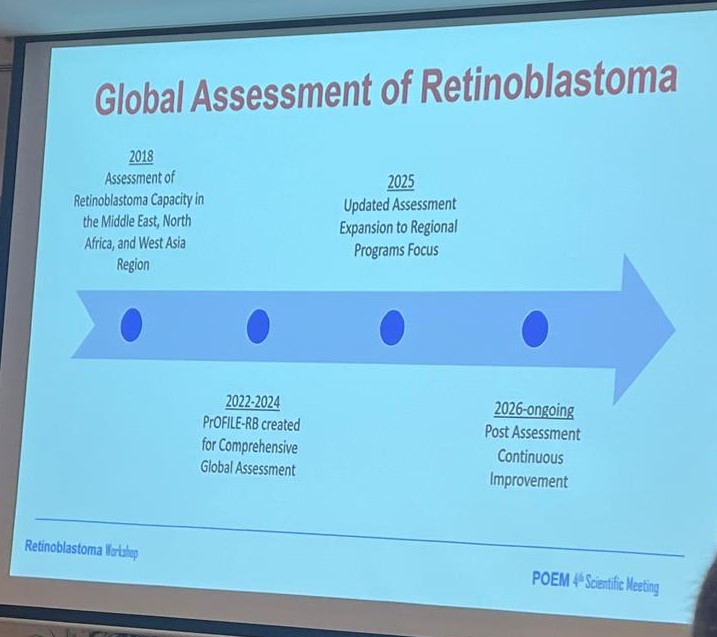
Building a Unified Retinoblastoma Registry
Susan Ybarra led a session on RB-Profile, likely detailing efforts to establish a centralized database to track retinoblastoma outcomes across the POEM region. Her talk may have focused on the value of collaborative data collection for benchmarking treatment protocols, enabling research, and driving quality improvement.
Regional Voices: Shared Lessons from Syria, Pakistan, and Iraq
Drs. Khaled Ghanem, Haleema Saeed, and Ahmed Sabhan shared national experiences in managing retinoblastoma in Syria, Pakistan, and Iraq respectively. These talks likely highlighted context-specific challenges – from conflict and access barriers to workforce shortages—and the innovative solutions their teams have implemented, such as public awareness campaigns, adapted treatment protocols, and cross-border collaborations.
The Retinoblastoma Workshop at the POEM 4th Scientific Meeting offered a comprehensive overview of clinical, genetic, and policy-level advances in retinoblastoma care across the POEM region. From early detection through genetic risk stratification to innovations in intra-ocular chemotherapy and telemedicine-driven models of care, the sessions emphasized collaboration, adaptation, and capacity building as key tools in improving pediatric ocular oncology outcomes. The workshop not only highlighted regional successes but also pointed to future directions in research, training, and equitable access. Find out more about POEM 4th Scientific Meeting in OncoDaily.