
A European Project to Better Understand and Treat Pancreatic Cancer
Pancreatic cancer, specifically pancreatic ductal adenocarcinoma (PDAC), is one of the most aggressive and deadly cancers, with an average survival rate of only 8 to 10 months after diagnosis.
This major medical challenge is at the core of the European COMBAT-PDAC project, which has received nearly two million euros in funding under the European Partnership for Personalised Medicine (EP PerMed).
This ambitious initiative is also supported by the French National Research Agency (ANR), ensuring robust funding for the French contributions to the project. The goal is to better understand tumor cell diversity and develop more effective personalized treatments.
A Multidisciplinary Approach to Advance Research
Under the coordination of Michele Solimena from the Paul Langerhans Institute in Dresden, the COMBAT-PDAC consortium brings together experts from renowned institutions, including the Helmholtz Institute of Dresden-Rossendorf, the European Institute of Oncology (IEO) in Milan, the Institute for Research in Biomedicine in Barcelona, the Vall d’Hebron Institute of Oncology (VHIO), and the Cancer Research Center of Marseille (CRCM – AMU/CNRS/Inserm/IPC).
The pancreatic cancer research team, led by Dr. Nelson Dusetti at the CRCM, contributes critical expertise in pancreatic cancer research with unique capabilities to model tumor responses in vitro.
“Our team has developed pancreatic organoid models that allow us to rapidly and accurately evaluate the efficacy of new treatments proposed within the consortium,” explains Dr. Dusetti.
These patient-derived models help to better understand the significant heterogeneity in treatment responses observed in clinical practice.
Why Is Pancreatic Cancer So Difficult to Treat?
Pancreatic cancer is particularly challenging to treat due to its high level of heterogeneity, both between patients and within individual tumors.
Each pancreatic tumor comprises multiple distinct cell populations with diverse genetic, molecular, and phenotypic characteristics.
This diversity complicates the effectiveness of standard treatments, as some cellular subpopulations can resist initial therapies, inevitably leading to recurrence and disease progression.
“To effectively treat this type of cancer, it is crucial to eliminate all tumor cells from the very beginning of treatment. Unfortunately, current therapies often fail to target the entire range of heterogeneous cell populations present within a tumor,” says Dr. Dusetti.
This biological complexity not only contributes to treatment resistance but also makes it difficult to develop biomarkers capable of predicting therapy responses.
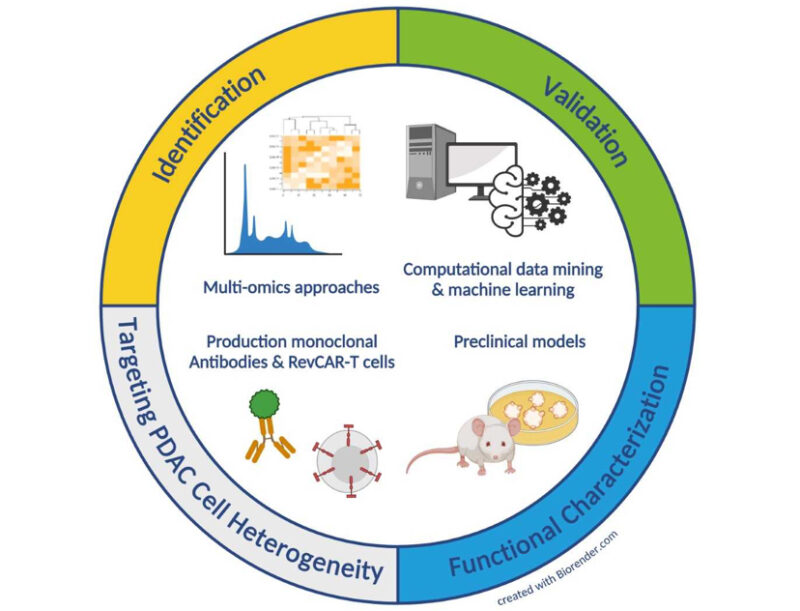
The COMBAT-PDAC project aims to address this challenge by adopting an integrated and innovative approach to identify specific markers for these different cell populations.
These markers could enable not only more precise diagnoses but also personalized treatments that maximize effectiveness and minimize recurrence. By tackling this intrinsic heterogeneity, the consortium hopes to pave the way for therapies truly adapted to the complexity of pancreatic cancer.
Toward Personalized and Targeted Treatments
A key objective of the project is to identify biomarkers capable of accurately predicting which patients will benefit from specific treatments.
“Using these models, we can not only evaluate the efficacy of innovative treatments across a wide range of patient-derived models but also highlight predictive biomarkers essential for personalizing new therapeutic strategies identified within this project,” emphasizes Dr. Dusetti.
By combining cutting-edge techniques such as in-depth genetic analysis, engineered antibodies, and modified T lymphocytes (CAR-T cells), the project seeks to develop therapeutic strategies that target the numerous distinct cell populations present in pancreatic tumors.
New Hope for More Effective and Personalized Treatments for Every Patient
The COMBAT-PDAC project represents hope for patients battling this formidable cancer. By combining fundamental research with clinical applications, the consortium aims to improve patient survival by developing treatments tailored to the complexity of each tumor.
“Through collaboration with international partners, we hope to provide innovative tools to better treat pancreatic cancer while paving the way for personalized therapeutic solutions,” concludes Dr. Dusetti.
Nelson Dusetti is the Scientific Director of the company Predicting Med (CSO) and Chair of TRANSLATE-IT CRCM. He is also research director at INSERM. He is the Head of the Department of Translational Research and Innovative Therapies at CRCM.
Further Reading:
Pancreatic Cancer: Symptoms, Causes, Types, Diagnosis & Treatment
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023
