Featuring molecular insights into cancer cell progression, novel predictive biomarkers for multiple cancer types, and strategies to improve immunotherapy treatments
The University of Texas MD Anderson Cancer Center’s Research Highlights showcases the latest breakthroughs in cancer care, research and prevention. These advances are made possible through seamless collaboration between MD Anderson’s world-leading clinicians and scientists, bringing discoveries from the lab to the clinic and back.
Neutrophils help cancer cells colonize abdominal fat
The omentum – a fatty tissue that suspends from the stomach – is a common site of metastasis for abdominal cancers, especially ovarian cancers. The omentum contains abundant clusters of immune cells, but it is unclear why they do not effectively defend against cancer cells. In a new study, researchers led by Won Jae Lee and Honami Naora, showed that neutrophils release webs of DNA called neutrophil extracellular traps (NETs) that specifically attract innate-like B cells to the omentum.
Furthermore, NETs stimulate these B cells to produce an immunosuppressive cytokine called interleukin (IL)-10 that helps cancer cells settle and grow. The study shows that NETs alter immune cells in the omentum before metastasis occurs, creating an immunocompromised environment that supports cancer cell colonization. Inhibiting NETs decreases these innate-like B cells in lab models, highlighting a potential therapeutic strategy.
New biomarker predicts improved outcomes with dose-dense chemotherapy in ER-positive breast cancer
A new biomarker study provides novel insights into how dose-dense chemotherapy can improve survival for some patients with estrogen receptor (ER)-positive breast cancer. In the study, researchers analyzed 12-year follow-up data from the Phase III CALGB 9741 trial, which included 1,973 patients with node-positive, early-stage breast cancer. The results showed that dose-dense chemotherapy, given every two weeks instead of the standard three-week schedule, improved disease-free survival by 20% and overall survival by 15%.
Using a biomarker test developed at MD Anderson in the lab of Fraser Symmans, the researchers discovered that 40% of the patients with a low endocrine activity index were most likely to benefit from this treatment. Their findings show that dose-dense chemotherapy is more effective than the standard schedule for women with early-stage ER-positive breast cancer and low endocrine activity index, and the results highlight the importance of biomarker-driven approaches in tailoring cancer therapies.

Many patients with metastatic renal cell carcinoma are treated with immune checkpoint inhibitors as part of their systemic regimens, but only a small subset of patients achieve durable long-term or curative responses. To identify molecular biomarkers for these exceptional responders and better predict which patients benefit most, researchers led by Sachet Shukla, utilized whole-exome and RNA sequencing to analyze pre-treatment tumor samples and matched germline samples from treated patients in two clinical trials.
The researchers identified several potential drivers of exceptional responses, including high clonal neoantigen load, heightened metabolic activity, and humoral immunity – a type of immune response using antibodies as evidenced by the presence of tertiary lymphoid structures. Prospective validation is needed before these biomarkers become clinically viable, but this multi-institutional study lays the foundation for better understanding the mechanisms underlying responses in this important subset of patients.

DNA is wrapped into nucleosomes that form chromatin and are rearranged by protein complexes. The INO80 chromatin remodeler enzyme moves nucleosomes along DNA and modifies its protein composition, which is important for many processes including gene regulation and cell differentiation.
To better understand how INO80 modifies the protein composition of nucleosomes, researchers led by Blaine Bartholomew, discovered that Arp5 – a protein subunit of INO80 – dynamically rotates, thereby switching the region of Arp5 contacting the nucleosome.
If one of these two contacts is broken, INO80 cannot modify the composition of the nucleosome, which is a crucial activity of INO80 and highlights the potential of targeting Arp5 therapeutically for several biological processes that could be useful in treatment of cancer and other diseases.

Mutation drives granulosa cell tumor growth, highlighting potential therapeutic targets
Adult granulosa cell tumors (AGCTs) constitute a rare type of ovarian cancer that typically involves a specific mutation in the FOXL2 gene, which disrupts ovarian function and can lead to incurable relapse. However, it is not well understood how this specific mutation is able to promote cancer cell growth. To provide further mechanistic insights, researchers led by Tyler Hillman, examined cell lines of relapsed AGCT with this specific mutation.
They found that the mutation causes the FOXL2 protein to interact abnormally with the glucocorticoid receptor, which normally helps control gene expression for various cell processes. By changing how the glucocorticoid receptor binds to DNA, mutant FOXL2 promotes genes involved in cancer cell growth. The study uncovers the co-regulation between the FOXL2 mutation and glucocorticoid receptors, highlighting potential therapeutic targets for this patient population.

CTLA-4 blockade generates greater memory response than PD-1 blockade
Immune checkpoint inhibitors targeting CTLA-4 and PD-1, which stimulate the body’s own T cells to eliminate cancer, are an efficient treatment strategy for many cancers. Notably, CTLA-4 blockade seemingly leads to more durable responses compared to PD-1 blockade. Some studies suggest this could be attributed to differing memory CD8 T cell responses from each strategy, but the mechanisms remain unclear.
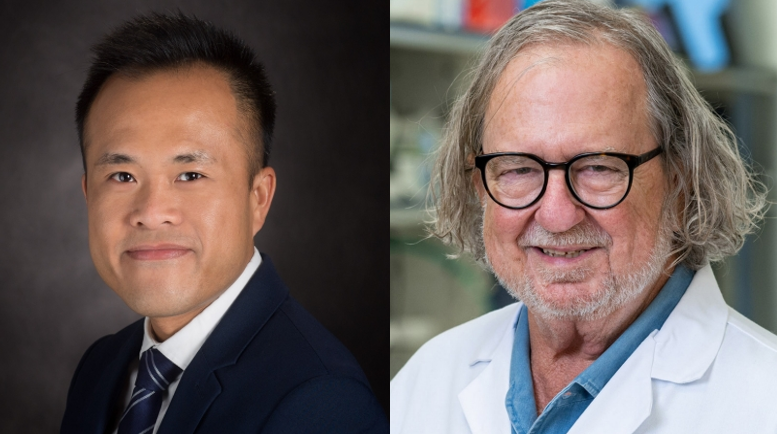
In a new study, researchers led by Stephen Mok and James Allison, used tumor and peptide vaccine models to demonstrate that CTLA-4 blockade generates memory CD8 T cells with greater expansion and a stronger antitumor response compared to PD-1 blockade. CTLA-4 blockade resulted in more memory CD8 T cells expressing the transcription factor TCF-1, which is essential for this response.
Moreover, CD4 T cells are required for the generation of memory CD8 T cells, further highlighting key differences between the two checkpoint therapies. Understanding the different long-term immune effects with these treatments can drive future therapeutic strategies to improve patient outcomes.
Biomarker levels provide insights into neuroendocrine tumor progression
Patients with advanced gastroenteropancreatic neuroendocrine tumors (GEP-NET) – rare tumors that develop in the pancreas or gastrointestinal tract – are routinely monitored for disease progression using imaging tests. Circulating chromogranin A (CgA) is an established biomarker for these tumors, but there are mixed results in using serum or plasma CgA to monitor disease progression.
In the prospective, multicenter CASPAR study, Qing Meng, and colleagues examined imaging tests from 153 patients with well-differentiated GEP-NET and validated an automated assay using serum CgA levels. The assay was highly accurate in ruling out tumor progression, with a diagnostic specificity of 93.4% and negative predictive value of 84.3%, but it was not as strong at detecting tumor progression.
These results show that serum CgA biomarkers are a valuable tool best used alongside routine monitoring, with imaging tests to improve clinical decision-making for patients with GEP-NET.

High T cell variety associated with improved response and fewer side effects in NSCLC
Patients with advanced non-small cell lung cancer (NSCLC) may benefit from immune checkpoint inhibition, but many end up with immune-related side effects, highlighting a need to identify potential risk factors. Patients with higher T cell receptor (TCR) richness in their peripheral blood have improved outcomes, but the characteristics of TCR and their role in side effects is poorly understood.
In the LONESTAR clinical trial, researchers led by Mehmet Altan, Alexandre Reuben, John Heymach, and Jianjun Zhang, used TCR sequencing methods on peripheral blood samples from patients with NSCLC receiving dual immune checkpoint therapy, characterizing T cells in relation to treatment response and side effects. Patients with a higher TCR diversity in their blood before treatment were more likely to respond and also had a lower risk of experiencing side effects. Knowing a patient’s peripheral blood TCR variety could help guide patient selection for dual immune checkpoint treatment.

Awards and Honors
Jason Huse, Professor of Anatomic Pathology, and Wen Jiang, Associate Professor of Radiation Oncology, have been elected to The American Society for Clinical Investigation.

Further reading:
MD Anderson Research Highlights: ASH 2024 Special Edition
Obe-cel CAR T Therapy Achieves High Response Rates in R/R B-cell ALL: FELIX Trial Results
MD Anderson study reveals hidden chromosomal abnormalities in healthy breast cells