GD2-CAR T-Cell Therapy Offers New Hope for Pediatric Brain Cancer
The clinical study on GD2-CAR T-cell therapy for childhood brain cancer, particularly diffuse intrinsic pontine glioma (DIPG) and other diffuse midline gliomas (DMG), has yielded pivotal findings that mark a significant step forward in pediatric neuro-oncology.
This novel therapy has recently received the Regenerative Medicine Advanced Therapy (RMAT) designation from the U.S. Food and Drug Administration (FDA), recognizing its potential to significantly improve treatment outcomes for patients with these historically incurable brain cancers.
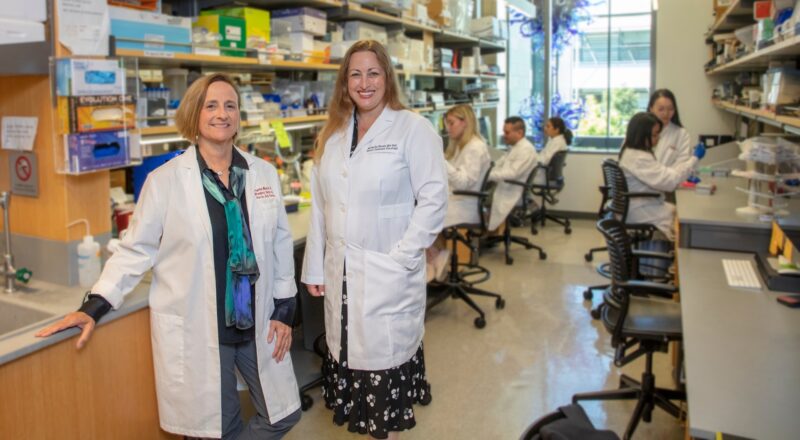
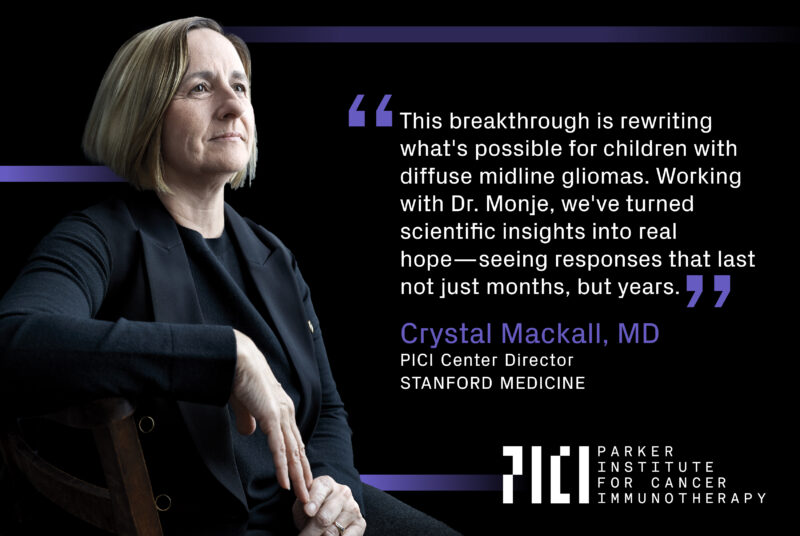
Crystal Mackall, MD, Center Director of the Parker Institute for Cancer Immunotherapy at Stanford, and Michelle Monje, MD, PhD, Milan Gambhir Professor in Pediatric Neuro-Oncology at Stanford Medicine, are leading a clinical trial to assess the safety and efficacy of GD2-CAR T-cell therapy for pediatric brain cancers.
In the trial, which involved 11 participants, 9 showed clinical benefits. Of these, 9 experienced functional improvements, with 4 having their tumor volume reduced by over 50%. Remarkably, one of the 4 patients achieved a complete response, meaning his tumor was no longer detectable on brain scans. Although it’s still too early to confirm if this patient is cured, he remains healthy more than 4 years after diagnosis. The findings, published in Nature on November 13, offer hope for children battling this and other aggressive brain and spinal cord tumors.
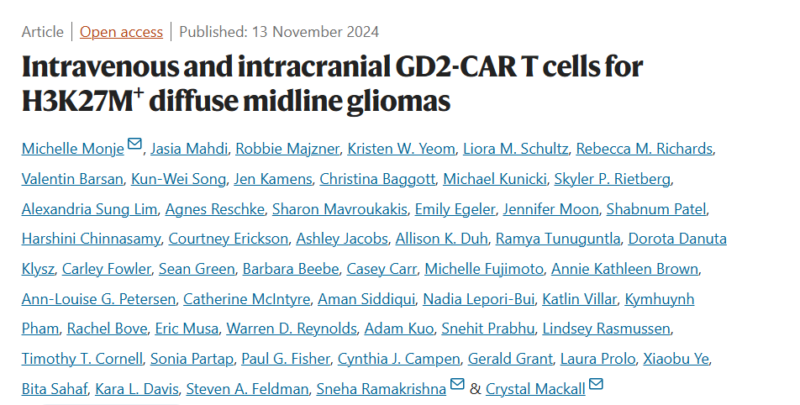
Intravenous and intracranial GD2-CAR T cells for H3K27M+ diffuse midline gliomas
Authors: Michelle Monje, Jasia Mahdi, Robbie Majzner, Kristen W. Yeom, Liora M. Schultz, Rebecca M. Richards, Valentin Barsan, Kun-Wei Song, Jen Kamens, Christina Baggott, Michael Kunicki, Skyler P. Rietberg, Alexandria Sung Lim, Agnes Reschke, Sharon Mavroukakis, Emily Egeler, Jennifer Moon, Shabnum Patel, Harshini Chinnasamy, Courtney Erickson, Ashley Jacobs, Allison K. Duh, Ramya Tunuguntla, Dorota Danuta Klysz, Carley Fowler, Sean Green, Barbara Beebe, Casey Carr, Michelle Fujimoto, Annie Kathleen Brown, Ann-Louise G. Petersen, Catherine McIntyre, Aman Siddiqui, Nadia Lepori-Bui, Katlin Villar, Kymhuynh Pham, Rachel Bove, Eric Musa, Warren D. Reynolds, Adam Kuo, Snehit Prabhu, Lindsey Rasmussen, Timothy T. Cornell, Sonia Partap, Paul G. Fisher, Cynthia J. Campen, Gerald Grant, Laura Prolo, Xiaobu Ye, Bita Sahaf, Kara L. Davis, Steven A. Feldman, Sneha Ramakrishna, Crystal Mackall.
About Crystal L. Mackall
Crystal L. Mackall, MD is the Ernest and Amelia Gallo Family Professor of Pediatrics and Medicine at Stanford University. She serves as the Founding Director of the Stanford Center for Cancer Cell Therapy, Associate Director of the Stanford Cancer Institute, Leader of the Cancer Immunotherapy Program, and Director of the Parker Institute for Cancer Immunotherapy.
Dr. Mackall has had a distinguished career in immuno-oncology, having spent 27 years at the National Cancer Institute (NCI), where she rose to become the Chief of the Pediatric Oncology Branch and Head of the Immunology Section. Since 2016, she has continued her pioneering work at Stanford, leading an internationally recognized translational research program in cancer immunotherapy, with a primary focus on pediatric cancers.
Her research has significantly advanced the understanding of fundamental immunology and its application to the treatment of human diseases. Dr. Mackall has led numerous first-in-human and first-in-child clinical trials, exploring treatments such as dendritic cell vaccines, cytokine therapies, and adoptive immunotherapy using natural killer (NK) cells and genetically modified T cells. Her work is at the forefront of developing novel immunotherapies that aim to revolutionize the treatment of children’s cancers and beyond.
About Michelle Monje

Michelle Monje, MD, PhD is the Milan Gambhir Professor of Pediatric Neuro-Oncology at Stanford University. She holds additional courtesy professorships in Neurosurgery, Pediatrics, Pathology, and Psychiatry and Behavioral Sciences. Dr. Monje practices at Stanford Medicine Children’s Health, where she leads pioneering research and clinical work in pediatric neuro-oncology, with a focus on brain cancers such as diffuse midline gliomas and DIPG (diffuse intrinsic pontine glioma). Her research aims to develop innovative therapies, including CAR-T cell therapy, to improve outcomes for children with these challenging, often fatal brain tumors.
“This is a universally lethal disease, and we’ve found a therapy that can cause meaningful tumor regressions and clinical improvements. Although there’s still much to optimize for each patient, the fact that one patient had a complete response is incredibly exciting. I’m hopeful he may be cured.” – said Michelle Monje
PICI:
“PICI applauds the FDA’s decision to grant Regenerative Medicine Advanced Therapy (RMAT) designation to the GD2-CAR T cell therapy for diffuse midline gliomas (DMG), devastating and almost always fatal pediatric cancers, with no approved therapies beyond palliative care.
The therapy was developed by Crystal Mackall, MD, Director of the PICI Center at Stanford Medicine (Mackall Lab), and Michelle Monje, MD, PhD, and team. The PICI-co-funded, first-in-child trial, in collaboration with Stanford, California Institute for Regenerative Medicine, CureSearch, has shown remarkable results.
Early results include improved neurological function, tumor shrinkage, and even a complete, durable response lasting over three years in one child. Results from Arm A of this study will be published in the coming weeks and the RMAT designation represents a critical step forward.”
Further Reading:
History of Immunotherapy: Cancer Treatment
CAR T Cell Therapy for Cancer Treatment


