Gustavo Viani, Professor of Radiation Oncology at Ribeirão Preto Medical School, University of Sao Paulo, shared a post on X:
“Do all early-stage breast cancer patients need axillary surgery?
The INSEMA trial challenges this long-standing practice, showing that skipping sentinel lymph node biopsy (SLNB) may be safe for select patients. plays a key role. Let’s dive into the data.”
Axillary surgery has been a cornerstone in breast cancer treatment for staging and control. But does every patient with early-stage, node-negative breast cancer need it?
The INSEMA trial explores the possibility of skipping sentinel lymph node biopsy (SLNB). Breast Cancer.
The INSEMA trial is a randomized, noninferiority study comparing:
•Surgery omission group (no axillary surgery)
•Surgery group (sentinel lymph node biopsy)
The goal? Evaluate if omitting axillary surgery compromises invasive disease-free survival. Cancer Research.
Over 5,500 patients with T1/T2 node-negative invasive breast cancer undergoing breast-conserving surgery were enrolled.
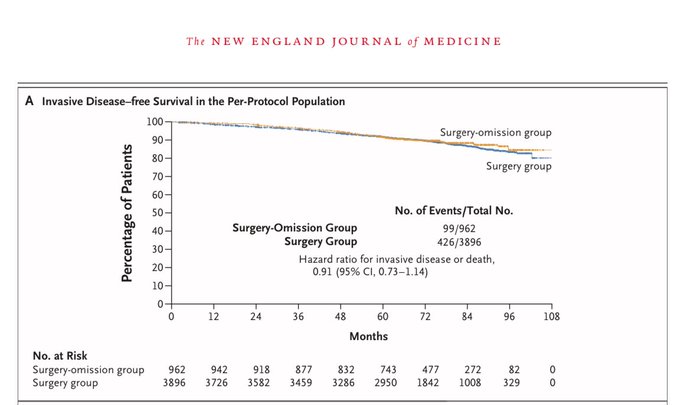
Results focused on 5-year invasive disease-free survival (IDFS). Here’s what they found.
Key results:
•IDFS rates:
•No axillary surgery: 91.9%
•SLNB: 91.7%
•Hazard ratio (HR): 0.91 (noninferior)
This suggests no significant difference in outcomes between groups.
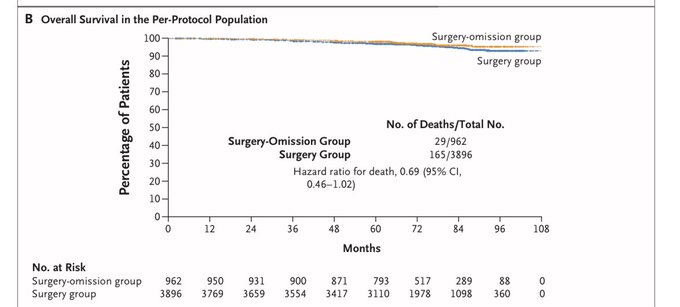
Survival outcomes:
•Overall survival (OS) at 5 years:
•No axillary surgery: 98.2%
•SLNB: 96.9%
Patients who skipped axillary surgery reported fewer complications and better quality of life.
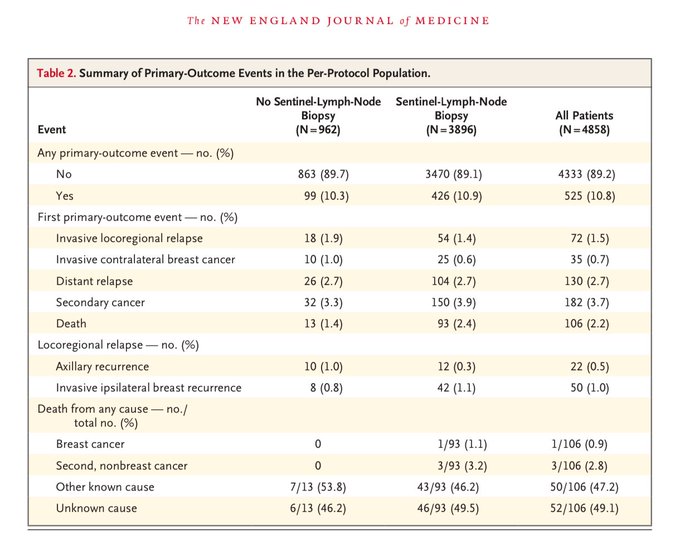
Recurrence rates:
•Axillary recurrence was slightly higher in the no-surgery group (1.0%) than in the SLNB group (0.3%).
•Despite this, recurrence did not impact disease-free or overall survival significantly.
The role of :
•For patients who skipped axillary surgery, incidental radiation doses to the axilla during whole-breast radiotherapy provided sufficient regional control.
•Axillary level I received ~85% of the prescribed dose for the breast, while level II received ~15%.
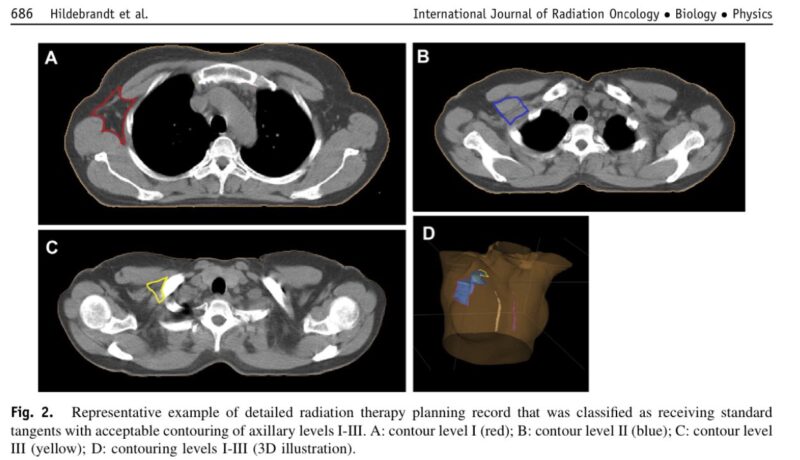
This incidental coverage ensured excellent outcomes while avoiding complications from additional targeted axillary radiation.
•Lymphedema: 1.8% (no surgery) vs. 5.7% (SLNB).
•Arm mobility issues: 2.0% vs. 3.5%.
•Pain with movement: 2.0% vs. 4.2%.
Thus compensated for the omission of axillary surgery in patients with low-risk, node-negative tumors. It played a key role in maintaining excellent control while reducing long-term morbidity.
Who benefits from omitting SLNB?
•Patients ≥50 years old.
•Low-risk, HR-positive, HER2-negative tumors ≤2 cm.
•G1 or G2 grade tumors.
This subgroup showed excellent outcomes without axillary surgery.
How does INSEMA compare to other trials?
•SOUND, BOOG, and NAUTILUS trials are also exploring de-escalation of axillary surgery.
•INSEMA’s large cohort and robust design offer strong evidence for sparing low-risk patients unnecessary interventions. Clinical Trial.
However, the findings apply to carefully selected patients. Higher-risk subgroups (e.g., younger patients or tumors >2 cm) need further evaluation before skipping SLNB becomes standard.
The INSEMA trial emphasizes a shift towards less invasive, patient-centered care in oncology. By sparing low-risk patients from unnecessary surgery, we enhance quality of life without compromising survival.
Gustavo Viani, MD is an Associate Professor in the Department of Medical Imaging, Hematology, and Oncology at Hospital das Clínicas, Faculty of Medicine of Ribeirão Preto, University of São Paulo (FMRP-USP). Dr. Viani’s research focuses on radiation oncology, with expertise in brachytherapy, stereotactic radiosurgery, dose fractionation, radiation tolerance, and overall oncology practices.
More posts featuring Gustavo Viani.


