Adolescents and young adults (AYAs), typically aged 15 to 39, face numerous life challenges, from puberty and establishing careers to navigating relationships. When cancer enters the picture, these hurdles become even more overwhelming. Each year, nearly 90,000 AYAs are diagnosed with cancer, and they often require specialized support to handle the unique complexities of cancer care during this pivotal life stage.
A new study titled “Influence of an AYA cancer program on cancer care delivery” published on ASCO highlights the positive impact of a decade-long program at the University of North Carolina (UNC) Lineberger Comprehensive Cancer Center, designed to better support AYAs with cancer. The program has significantly improved outcomes for this group, particularly in areas such as fertility counseling, which is crucial for young cancer patients concerned about their future ability to have children.
Authors: Jacob Newton Stein, Dawn Ritzwoller, Catherine Swift, Melissa Matson, Alexis Caroline Wardell, Hannah Clark Winslow, Austin Waters, Emily Ruth Haines, Lauren Lux, Andrew Brian Smitherman.
This study evaluates the impact of the Adolescent and Young Adult (AYA) Cancer Program at the University of North Carolina (UNC) on cancer care for patients aged 13-39. The program, established in 2015, aims to address barriers to care and stagnant survival rates for AYAs with cancer. It provides services such as fertility counseling, improved access to clinical trials, specialized sarcoma care, a survivorship clinic, and psychosocial support. The program focuses on creating personalized care plans to meet both the medical and psychosocial needs of AYA patients.
A retrospective cohort study was conducted over an 8-year period (2014-2022) using electronic health records (EHR) and State Cancer Registry data. The study compared AYA patients who received care through the AYA Cancer Program with those who did not. The analysis looked at sociodemographic characteristics, cancer site, treatment, and care utilization. Key outcomes measured included complications, supportive care services utilization, and overall treatment outcomes.
The study used SMR propensity weighting and multivariable log binomial modeling to adjust for factors such as age, race, sex, cancer site, metastatic status, and receipt of systemic therapy. The results highlight the positive influence of the AYA Cancer Program on clinical trial participation, fertility preservation, and psychosocial support, demonstrating improvements in outcomes for AYA cancer patients.
Results of the Study
A total of 4,016 AYAs receiving cancer care at UNC were included in the study, with 670 of these patients having contact with the AYA Cancer Program. Among the patients engaged in the program, several key differences were observed compared to those who did not participate in the program. Specifically, program-engaged patients were typically younger at the time of diagnosis, which reflects the program’s focus on adolescents and young adults. Additionally, these patients were more likely to be Black, highlighting the potential role of targeted outreach to underserved populations. Furthermore, these patients had higher rates of metastatic disease or hematologic malignancies, which are more complex cases that might benefit from specialized care coordination.
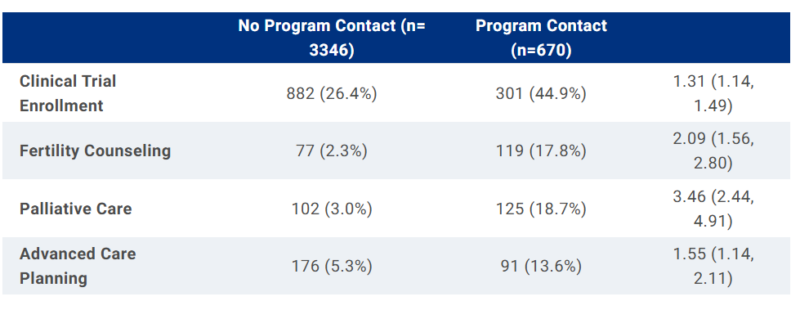
In terms of outcomes, weighted model analyses showed that patients who participated in the program were significantly more likely to receive guideline-recommended care. This included enrollment in clinical trials, which offers access to cutting-edge therapies and can be critical for treatment of rare or advanced cancers; receipt of fertility counseling, an essential service for many AYAs who may want to preserve their fertility before undergoing cancer treatments that can affect reproductive health; palliative care, which focuses on improving quality of life by managing symptoms and providing psychosocial support; and advanced care planning, which involves discussing and documenting treatment preferences and end-of-life care plans, an important aspect of care that is often overlooked in younger populations.
The program’s reach and impact grew significantly over time. Initially, only 6% of the total AYA population at UNC engaged with the program. However, by the end of the study period, more than 25% of the AYA cancer patients were connected with the program. This substantial increase demonstrates the program’s success in expanding its services and making a positive impact on the cancer care of adolescents and young adults.
About Jacob Newton Stein
Dr. Jacob Newton Stein is a medical oncologist at the University of North Carolina (UNC) Lineberger Comprehensive Cancer Center, specializing in the treatment of sarcomas, a rare and diverse group of cancers that can affect patients across all age groups, including adolescents and young adults. With a patient-centered approach, Dr. Stein is dedicated to listening closely to his patients and addressing their concerns while collaborating with multidisciplinary teams to deliver high-quality, cutting-edge cancer care. He is committed to providing equitable care to all patients, ensuring that everyone, regardless of background or circumstances, has access to the best possible treatment.
In addition to his clinical work, Dr. Stein is a health services researcher with a focus on optimizing cancer care delivery systems. His research aims to improve the quality of care for patients, especially those from underserved populations. Current research projects include developing interventions to enhance the delivery of precision medicine for patients with advanced cancer, creating predictive models to identify those at high risk for complications from cancer therapies, and aligning sarcoma care with the goals and needs of younger patients. His work seeks to bridge gaps in cancer care and reduce health disparities.
Dr. Stein completed his undergraduate education at Emory University before attending medical school at the University of North Carolina at Chapel Hill. He then went on to complete his residency at the University of Washington and his fellowship at the University of North Carolina at Chapel Hill. Through his combination of clinical expertise and research, Dr. Stein is dedicated to improving outcomes for cancer patients, particularly those with rare and complex cancers like sarcomas.


