Sebastian Schmidt, Head of Strategy and Medical Affairs Computed Tomography at Siemens Healthineers, shared a post on LinkedIn:
“Lung Cancer Screening – what does it mean for surgery and pulmonology?
lung cancer screening is moving forward, more and more countries are starting and participation grows.
But what does it mean for surgeons and pulmonologists? Can the additional patient volume be handled?
A recent publication from Anton Manyak (DOI: 10.1016/j.chest.2023.02.010) and team sheds some light on what surgeons and interventional pulmonologists can expect.
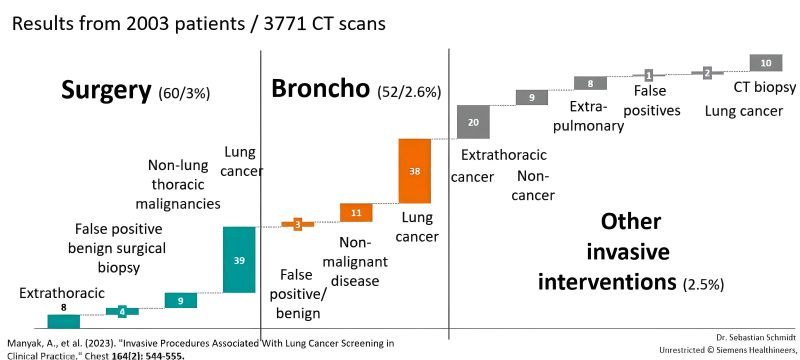
They analyzed a screening program with 2003 participants / 3771 CT scans.
They detected lung cancer in 58 patients (2.9%), which is a high value, well above the typical 1-1.5% – likely due to an above-average risk in their population. The screening caused 160 interventions.
Good news: The number of interventions for false-positives was very low. Four surgical biopsies and three bronchoscopies revealed benign findings, this is 0.3% of the participants. Again a confirmation that interventions on false-positives are very rare with modern guidelines, much below other screening programs and nothing to worry about.
2.6% of the participants got a bronchopscopy, 3% surgery. Surgery was predominantly lobectomy, followed by sublobectomy. Please notice that this was before the landmark publication of CALGB 140503 by Nasser Altoki and team, today the share of sublobar resections would likely be higher.
Interesting is the share of bronchoscopies and surgeries for diseases other than lung cancer: Examples are infections, ILDs, esophageal cancer, AAA or breast cancer.
If we upscale these nnumbers to a program with one million participants (e.g. Germany or UK), we can expect:
– 26.000 bronchoscopies for nodules, mostly sized 8-15mm. This stands in relation to >400k bronchoscopies in Germany today for other reasons. However, bronchoscopic biopsies of small nodules can be challenging
– 30.000 surgeries, mainly sublobar resections and lobectomies. This would indeed be a change, given the rarity of stage Ia cancer in some countries today
– Significantly less systemic stage IV treatments
On the economics, most analyses show that the additional cost for bronchoscopies and early-stage surgery is balanced by savings for late-stage therapy. This is further shifting in favour of screening, due to improvements in minimally invasive surgery (less morbidity) and raising costs for late-stage treatments.
These changes are clearly doable in most healthcare system, still may require needs for training of staff, upgrades in equipment for bronchoscopy and a shift in spending. These changes should be on the radar of surgeons and pulmonologists.
The reduction in mortality is clearly worth the effort, and the effort is balanced by less effort in late-stage therapies.”
Source: Sebastian Schmidt/LinkedIn


