Understanding Chemotherapy-Induced Neuropathy: What Every Patient Should Know
When going through chemotherapy, many people are prepared for side effects like hair loss or nausea. But fewer expect something that can feel just as disruptive—nerve damage, also known as chemotherapy-induced peripheral neuropathy, or CIPN. This condition happens when certain cancer treatments affect the nerves that carry signals between your brain, spinal cord, and the rest of your body—especially your hands and feet. Not every chemotherapy drug causes neuropathy, but some are more likely to. These include platinum-based drugs like cisplatin and oxaliplatin, taxanes such as paclitaxel and docetaxel, and vinca alkaloids like vincristine. Other medications like bortezomib or thalidomide, often used in blood cancers, can also affect the nerves. The risk often depends on the type and amount of chemotherapy you receive, as well as how long you’ve been on treatment.
In this article, we’ll walk you through what neuropathy is, what causes it, and how you can recognize the signs early. We’ll also explore ways to relieve the symptoms, tips for staying safe at home, and the kinds of questions you can ask your doctor. Whether you’re currently in treatment or recovering afterward, knowing more about neuropathy can help you take better care of yourself and improve your quality of life.
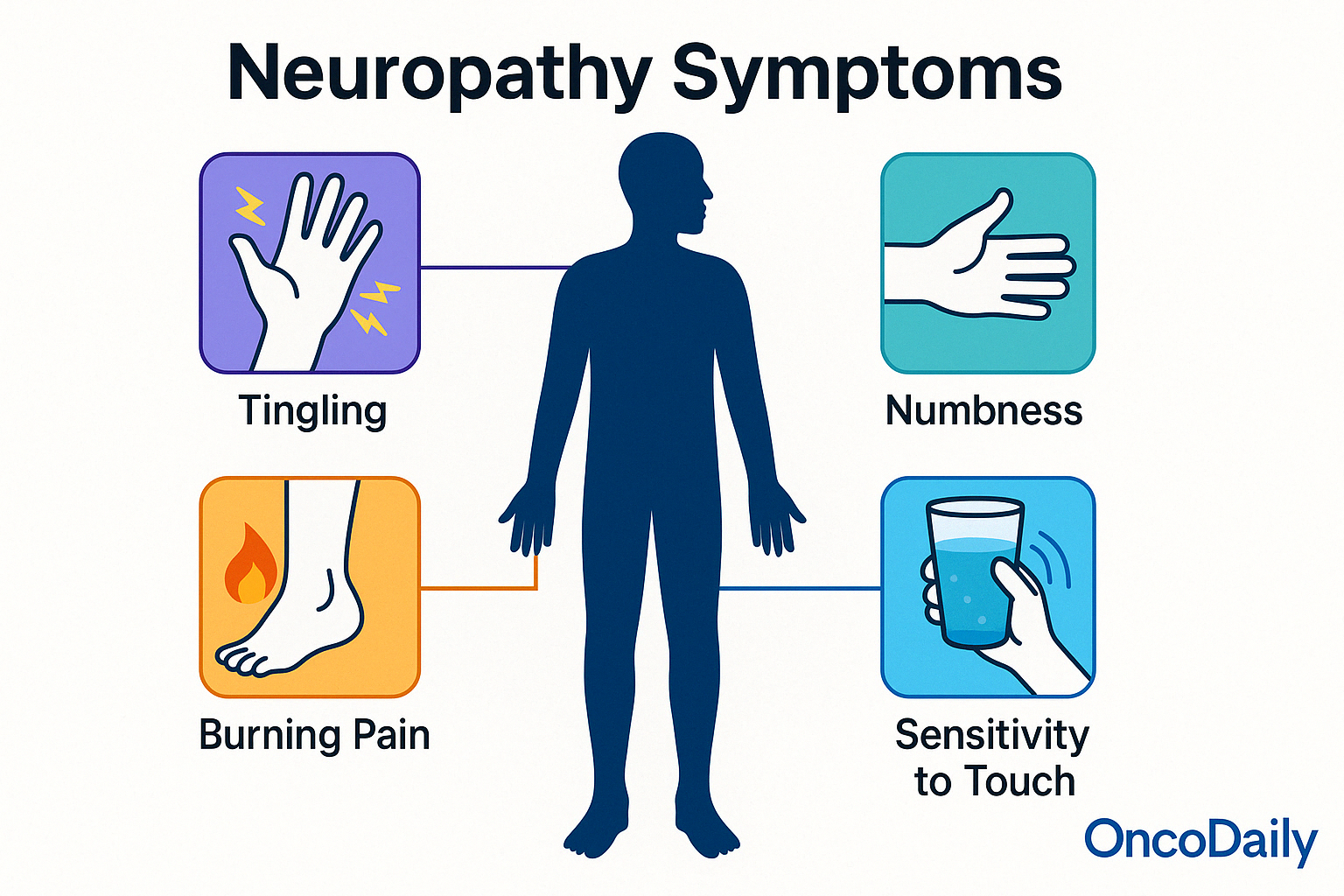
What Are the Symptoms of Chemotherapy-Induced Neuropathy?
Neuropathy can feel different for each person, but many people describe it as a change in sensation—like their body isn’t “communicating” properly with their nerves. One of the most common early signs is a tingling or “pins and needles” feeling, especially in the hands, fingers, feet, or toes. Some people feel numbness, as if those areas are “asleep” or less responsive. Others experience a burning or sharp pain, even without any clear cause. You may also become more sensitive to touch, cold, or heat, where everyday activities like buttoning a shirt, walking barefoot, or holding a cold glass of water feel uncomfortable or even painful. In some cases, neuropathy affects the nerves involved in balance and coordination, making it harder to walk steadily or climb stairs.
These symptoms may come and go or steadily get worse, depending on the chemotherapy type and duration. Recognizing them early and discussing them with your doctor is key to managing neuropathy and preventing further nerve damage.
When Do Neuropathy Symptoms Appear, and How Long Do They Last?
Neuropathy symptoms can begin at any point during chemotherapy—sometimes after just a few treatments, or they may develop gradually over time. For some people, the tingling or numbness becomes noticeable only after treatment has ended, as the nerves continue reacting even after the drugs are out of the system. How long the symptoms last varies widely. In many cases, the nerve irritation is temporary and gradually improves in the weeks or months after chemotherapy stops. But for others, especially those who received higher doses or longer courses of neurotoxic drugs, neuropathy may persist for months—or even become permanent.
That’s why it’s so important to report symptoms early. Your care team may be able to adjust your treatment plan, suggest medications or therapies to ease discomfort, and help prevent the symptoms from getting worse.
How Is Neuropathy Diagnosed?
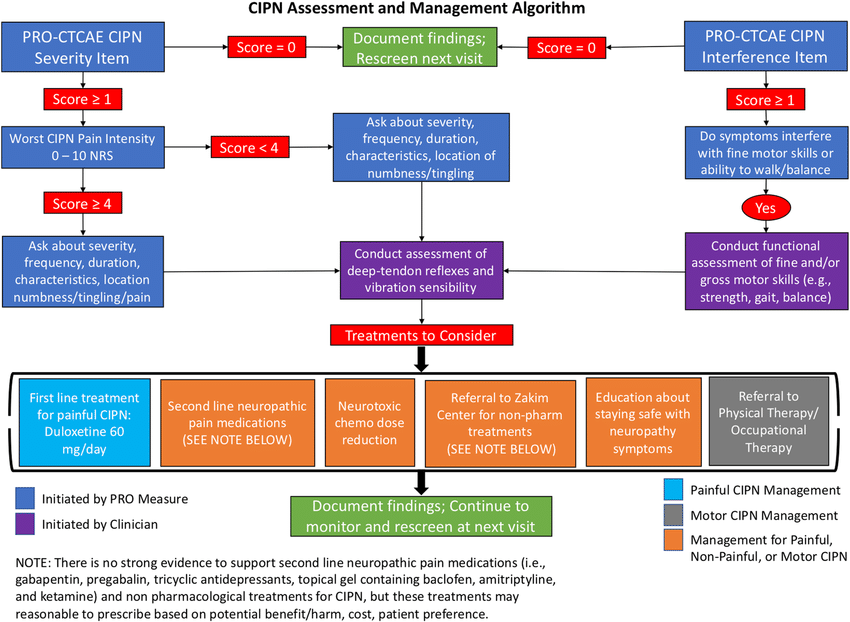
Diagnosing chemotherapy-induced neuropathy usually begins with a detailed discussion of your symptoms. Your doctor will ask when the sensations started, what they feel like (tingling, numbness, pain, etc.), how often they occur, and whether they’re affecting your ability to walk, sleep, or perform daily tasks. Since neuropathy is often a subjective experience, your own description plays a key role in helping your care team understand what’s happening.
Next, your doctor may perform a neurological exam. This involves checking your reflexes, muscle strength, balance, and sensitivity to touch, temperature, or vibration. For example, you may be asked to close your eyes while the doctor lightly touches your feet with a tuning fork or soft tool to see how your nerves respond. In more complex or unclear cases—especially when symptoms are severe or don’t match the usual patterns—your doctor might order a nerve conduction study or electromyography (EMG). These tests measure how well your nerves transmit signals and how your muscles respond. While not always necessary, they can help confirm the diagnosis and rule out other nerve conditions unrelated to chemotherapy.
Early diagnosis allows for quicker intervention, which may reduce the risk of long-term damage. Keeping a symptom journal and reporting changes promptly can be extremely helpful in guiding this process.
How Is Chemotherapy-Induced Neuropathy Treated or Managed?
If you’re experiencing nerve pain or tingling during or after chemotherapy, you’re not alone—and the good news is that there are several ways to manage the symptoms and help protect your quality of life. While neuropathy may not always be reversible, many people find relief through a combination of medication, therapy, and small changes at home.
Doctors often start with medications that calm nerve pain. One commonly used option is duloxetine (Cymbalta)—originally an antidepressant, but now shown to help with nerve pain in people receiving chemotherapy. Others may be prescribed gabapentin (Neurontin) or pregabalin (Lyrica), which were first developed for seizures but work well for nerve-related symptoms like burning, tingling, or sharp pain. These medications won’t heal the nerves, but they can make the discomfort much easier to live with, especially when it’s interfering with sleep or daily activities. Beyond medication, physical and occupational therapy can be incredibly helpful. A physical therapist can guide you through gentle exercises to improve balance, strength, and coordination, which is especially important if your feet feel numb or weak. If you’re finding it hard to grip objects or do things like button a shirt, an occupational therapist can offer strategies and tools to make everyday tasks easier and safer.
There are also simple steps you can take at home. Wearing gloves while cooking or cleaning can protect sensitive fingers. If your feet are affected, wearing socks and well-fitting shoes indoors can prevent injuries you might not feel. Daily skin checks are important too—neuropathy can dull your sense of touch, so you might not notice a cut or burn right away. And while it may sound unrelated, cutting back on alcohol and managing blood sugar—especially for people with diabetes—can help protect nerve health.
Can Chemotherapy-Induced Neuropathy Be Prevented?
While there is no guaranteed way to prevent chemotherapy-induced neuropathy, researchers and doctors are working hard to understand who is most at risk and how to protect the nerves before damage occurs. Knowing the risk factors and staying in close communication with your care team can help reduce the chance of severe or lasting symptoms. Some people are more likely to develop neuropathy during treatment. This includes individuals who already have pre-existing nerve problems, such as from diabetes, vitamin B12 deficiency, or a history of alcohol overuse. Older age and receiving high doses or multiple rounds of neurotoxic chemotherapy drugs (like taxanes or platinum-based agents) also raise the risk.
Researchers are exploring several approaches to prevent neuropathy. These include testing protective medications, such as certain vitamins (like vitamin B6 or B12) and antioxidants, as well as newer drugs that aim to shield the nerves during treatment. So far, no single strategy has been proven effective for everyone, and more studies are needed. However, participating in clinical trials or discussing potential preventive options with your doctor may be helpful—especially if you’re at higher risk.
Tips for Daily Living with Neuropathy
Living with chemotherapy-induced neuropathy can feel overwhelming at times, especially when everyday tasks become more difficult or uncomfortable. But with a few thoughtful adjustments, it’s possible to protect yourself, stay active, and improve your comfort and confidence at home.
One of the most important things to focus on is safety. Since neuropathy can affect your balance and sensation—particularly in your feet—it’s a good idea to take precautions to prevent falls. Wearing sturdy shoes even inside the house, keeping floors free of clutter, and using non-slip mats in the bathroom can go a long way in preventing injuries. If your hands are affected, be cautious around hot surfaces or sharp objects, and consider using gloves when cooking or cleaning to avoid burns or cuts that you might not feel. Because nerve damage can also reduce your ability to sense temperature or pain, it’s helpful to check your skin daily—especially your feet and hands—for any signs of blisters, injuries, or irritation. Use warm (not hot) water when bathing, and test the temperature with a sensitive area like your elbow before using heating pads or warm compresses.
It’s also important to know when to contact your doctor. If you notice that your symptoms are getting worse—such as increased numbness, sharp pain, or difficulty walking—don’t wait for your next appointment. These could be signs that your nerves are under more stress, and early intervention may help prevent permanent damage. Let your care team know if neuropathy is affecting your sleep, mood, or ability to do basic tasks—they want to help you feel as comfortable as possible. Emotionally, neuropathy can take a toll. The changes to your body and daily life can lead to frustration, anxiety, or even sadness. That’s completely normal. Talking with your care team about how you’re feeling is just as important as reporting physical symptoms. Support groups—either in person or online—can also provide a space to connect with others who truly understand what you’re going through. Small acts of self-care, like taking short walks, listening to music, or journaling your thoughts, can help you feel more in control.
Talking With Your Doctor About Neuropathy
When you’re dealing with chemotherapy-induced neuropathy, one of the most helpful things you can do is keep an open line of communication with your healthcare team. Your doctor can’t feel what you’re feeling—so the more clearly you can describe your symptoms, the better they can support you. Start by keeping a simple symptom journal. Write down when you notice tingling, numbness, or pain, where it happens (hands, feet, etc.), how often it occurs, and whether it affects your daily life—like walking, sleeping, or using your hands. Also note if the symptoms seem to be getting better, worse, or staying the same. This can help your doctor track how your nerves are responding to treatment and whether changes need to be made. During your appointments, it’s a good idea to ask questions such as:
-
Are these symptoms normal for the type of chemo I’m getting?
-
Is there anything I can do to reduce the discomfort or protect my nerves?
-
Are there medications or therapies that could help?
-
Will this neuropathy go away after treatment ends, or could it be long-term?
-
Should we consider adjusting my chemotherapy plan?
-
Are there signs I should watch for that mean I need to call right away?
You might also ask if your hospital offers access to pain specialists, physical therapists, or supportive care programs. Remember, no question is too small—your comfort, safety, and quality of life matter just as much as your treatment outcome. The more informed and involved you are, the better prepared you’ll be to manage neuropathy and continue your cancer journey with confidence.
You Can Watch More on OncoDaily Youtube TV
Written by Toma Oganezova, MD
FAQ
What is chemotherapy-induced peripheral neuropathy (CIPN)?
CIPN is nerve damage caused by certain chemotherapy drugs. It can lead to symptoms such as tingling, numbness, burning, or pain—usually in the hands and feet.
Which chemotherapy drugs are most likely to cause neuropathy?
Common culprits include platinum-based drugs (e.g., cisplatin, oxaliplatin), taxanes (e.g., paclitaxel, docetaxel), vinca alkaloids (e.g., vincristine), and other agents like bortezomib and thalidomide.
What are the early signs of chemotherapy-induced neuropathy?
Patients often report tingling, “pins and needles,” numbness, burning pain, or sensitivity to touch and temperature. These symptoms usually begin in the fingers and toes.
When do CIPN symptoms usually start?
They can appear after a few treatments or later in therapy. Some people don’t notice symptoms until chemotherapy has ended.
Will neuropathy go away after chemotherapy ends?
For some, symptoms improve or resolve over time. For others—especially those who received high doses or long treatments—neuropathy can become long-term or permanent.
How is neuropathy from chemotherapy diagnosed?
Diagnosis is based on patient-reported symptoms, a neurological exam, and sometimes tests like nerve conduction studies or electromyography (EMG).
What treatments are available for chemotherapy-induced neuropathy?
Medications like duloxetine, gabapentin, or pregabalin can help manage pain. Physical and occupational therapy may improve function. Lifestyle adjustments and safety strategies also help.
Can chemotherapy-induced neuropathy be prevented?
There is no guaranteed way to prevent it, but identifying risk factors and discussing protective strategies with your doctor can reduce severity.
What should I do if my neuropathy symptoms are getting worse?
Tell your doctor immediately. Early intervention can prevent progression and may lead to adjustments in your treatment or symptom relief strategies.
How can I stay safe at home if I have neuropathy?
Wear shoes indoors, use non-slip mats, avoid hot surfaces, check your skin daily, and make home modifications to prevent falls or injuries.
-
Challenging the Status Quo in Colorectal Cancer 2024
December 6-8, 2024
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023