
Olubukola Ayodele: The question is no longer if we can extend survival, but how much
Olubukola Ayodele, Head of Breast Cancer Unit at University Hospitals of Leicester NHS Trust, shared a post on LinkedIn:
“Yesterday, during a meeting, the speaker asked what we would like other specialties and the public to know about oncology. Many thoughts came to mind, but I concluded that it’s important for everyone to understand that new systemic anticancer therapies (SACT), such as targeted therapy and immunotherapy, have significantly improved the treatment of previously incurable solid tumors.
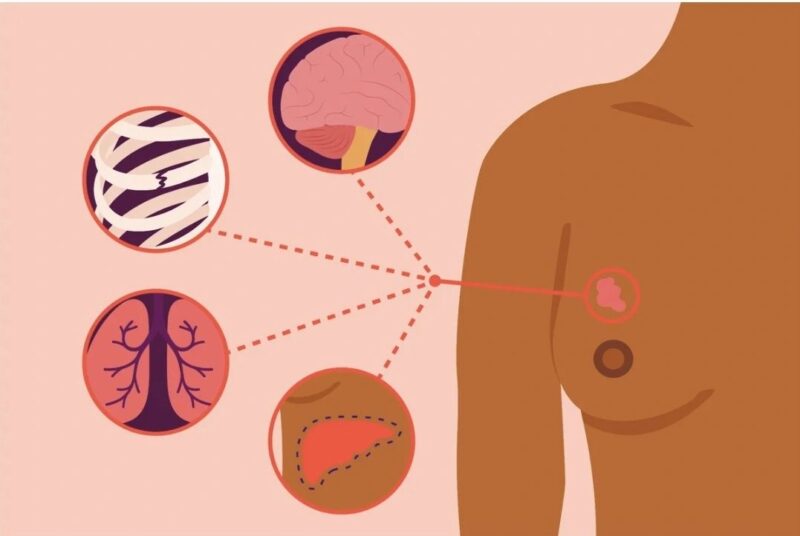
For years, a diagnosis of metastatic breast cancer (MBC) was considered a terminal event, with treatment focused on palliation rather than meaningful extension of life. However, in the past decade, we’ve witnessed a paradigm shift. The introduction of novel systemic therapies – targeted agents, antibody-drug conjugates (ADCs), and immunotherapy – has fundamentally altered the illness trajectory of what we once called ‘incurable’ solid tumors.
Take HER2-positive breast cancer, for example. Historically, this subtype carried a grim prognosis in the metastatic setting. The advent of trastuzumab was a breakthrough, but it was just the beginning. With the arrival of next-generation HER2-targeted therapies like trastuzumab deruxtecan (T-DXd), patients are now experiencing response rates and survival outcomes that were unimaginable a decade ago. Many are living not just months but years with a quality of life that allows them to work, travel, and engage fully with their families.
Hormone receptor-positive breast cancer has also undergone a transformation. The introduction of CDK4/6 inhibitors has redefined first-line treatment for metastatic disease, doubling progression-free survival in many cases. More recently, oral SERDs and AKT inhibitors have expanded options, personalizing therapy based on molecular profiling.
Even triple-negative breast cancer, once the most unforgiving subtype, has seen remarkable progress. Immunotherapy, particularly when combined with chemotherapy in PD-L1+ disease, has extended survival, and ADCs like sacituzumab govitecan are providing durable responses in later-line settings.
While a cure remains elusive for most patients with metastatic disease, these advances are enabling a chronic disease model for many. We now speak in terms of long-term management rather than just end-of-life care. As an oncologist, it is incredibly rewarding to offer patients HOPE grounded in real science – not just wishful thinking.
The future is even brighter. With ongoing clinical trials exploring novel combinations, bispecific antibodies, and personalized approaches based on liquid biopsies, we are continuously redefining what is possible. The question is no longer IF we can extend survival, but HOW MUCH – and at what point ‘incurable’ may no longer apply.”
-
Challenging the Status Quo in Colorectal Cancer 2024
December 6-8, 2024
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023
