
New Paper Alert: Management of Immune Checkpoint Inhibitor-Associated Toxicities in Older Adults with Cancer
Immune Checkpoint Inhibitor-Associated Toxicities are still a huge obstacle for patients, especially for older adults. When it comes to older adults, managing immune-related adverse events (irAEs) presents unique challenges. This population is more susceptible to these toxicities due to age-related factors such as frailty, comorbidities, and polypharmacy. As ICIs become increasingly common in cancer treatment, understanding how to tailor their use for older patients is crucial. This article reviews the impact of ICIs in elderly cancer patients, emphasizing the importance of comprehensive geriatric assessments (CGA) in guiding treatment decisions and managing irAEs effectively.
Title: Management of immune checkpoint inhibitor-associated toxicities in older adults with cancer: recommendations from the International Society of Geriatric Oncology (SIOG)
Authors: Colm Mac Eochagain, MB, Nina Rosa Neuendorff, MD, Karolina Gente, MD, Prof Jan Leipe, MD, Marthe Verhaert, MD, Christine Sam, MD, Nienke de Glas, PhD, Sindhuja Kadambi, MD, Beverly Canin, Fabio Gomes, MD, Prof Lore Decoster, PhD, Prof Beatriz Korc-Grodzicki, PhD, Siri Rostoft, Nicolò Matteo Luca Battisti, MD, Prof Hans Wildiers, PhD
Published in Lancet Oncology, 2025
Background
Immunotherapy has revolutionized cancer treatment, particularly immune checkpoint inhibitors (ICIs), which have proven effective in various malignancies. However, managing immune-related adverse events (irAEs) in older adults poses unique challenges. Older patients are more susceptible to these adverse events due to age-related factors such as comorbidities, frailty, and polypharmacy. This article focuses on the impact of ICIs in elderly populations, with a particular emphasis on immune-related adverse events and the critical role of comprehensive geriatric assessments (CGA) in guiding treatment decisions.
Methods
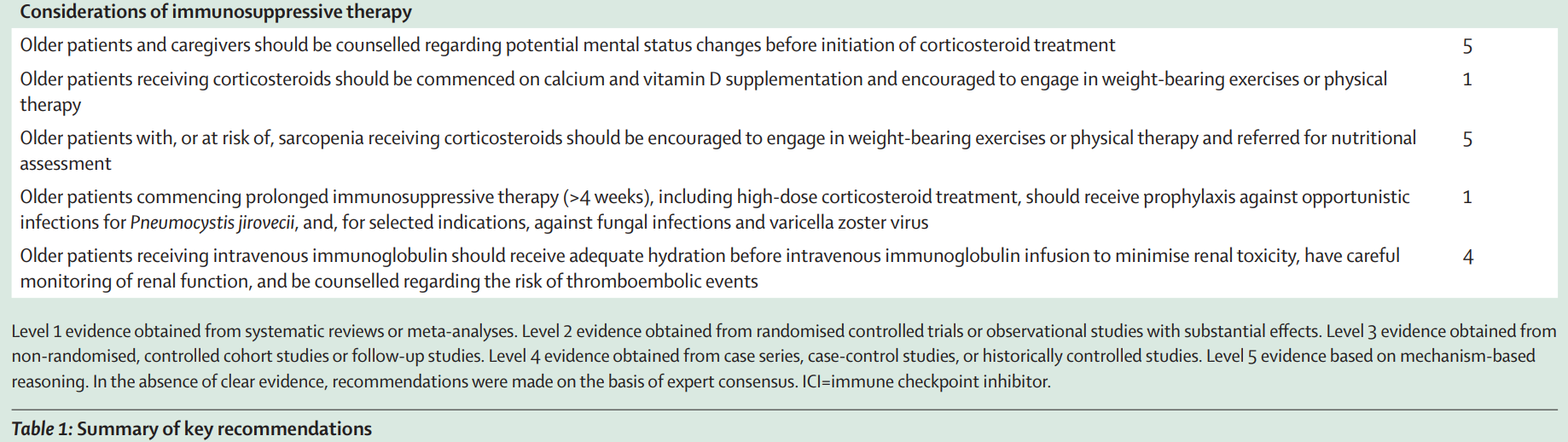
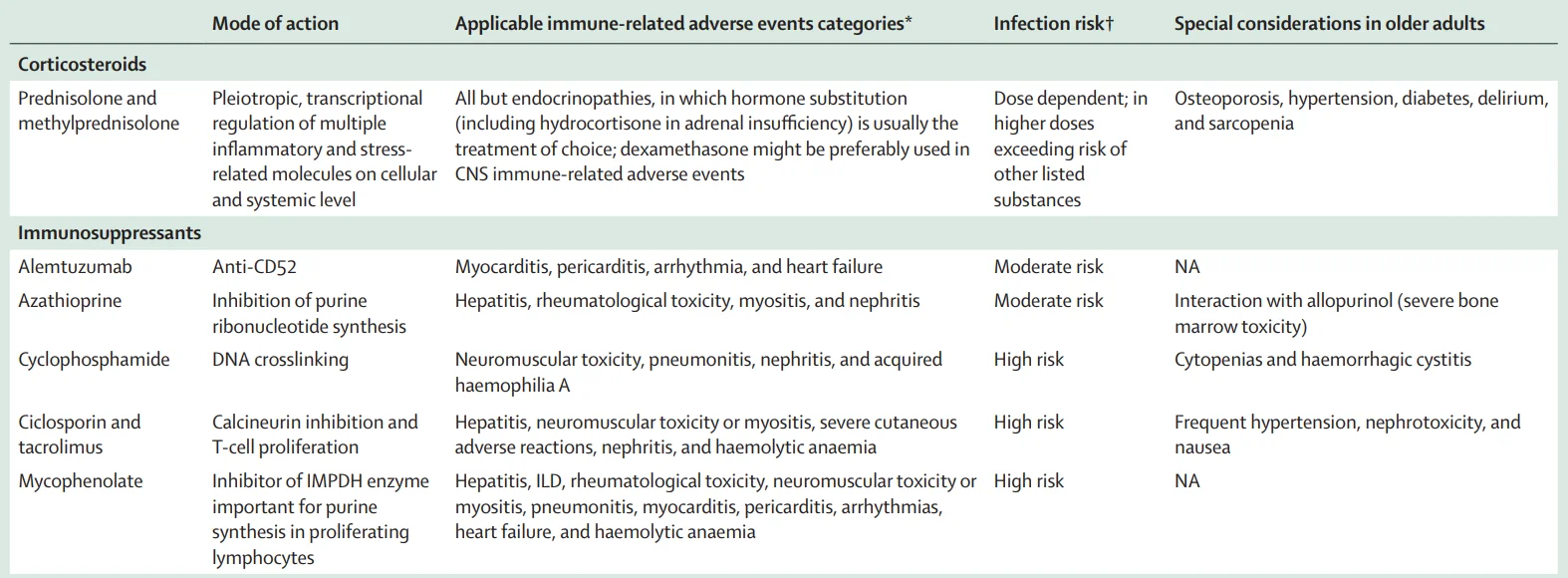
The article provides a thorough review of available literature, focusing on studies that address the use of ICIs in older adults with cancer. It synthesizes data from clinical trials, observational studies, and expert opinions, with a focus on immune-related adverse events. The review examines the incidence, severity, and management of these events in patients aged 70 years or older, including a discussion on the safety of various immunosuppressive therapies. It also explores strategies for optimizing treatment outcomes through multidisciplinary care.
Study Design
The review includes both prospective and retrospective studies involving older patients receiving ICIs for various types of cancer. It evaluates immune-related adverse events, comparing older adults to younger patients and identifying factors that contribute to increased susceptibility, such as frailty and pre-existing conditions. The article also discusses the role of geriatric assessments in managing these events and highlights the importance of a personalized approach to treatment.
Results
The review highlights that older adults receiving ICIs face a distinct set of challenges compared to younger patients. While the overall incidence of grade 3–5 immune-related adverse events may not differ significantly between older and younger patients, older adults often experience more severe consequences due to their comorbidities and frailty. Common adverse events include gastrointestinal, dermatologic, and pulmonary toxicities, with older patients being more vulnerable to complications such as infections, delirium, and corticosteroid-related side effects.
One notable finding is that older adults with frailty have a higher risk of hospitalization and death compared to non-frail patients, despite similar rates of adverse events. Furthermore, although the risk of corticosteroid-associated delirium does not appear to be greater in older patients, frail individuals are more prone to delirium-related complications, such as falls.
Key Findings from Immune Checkpoint Inhibitor-Associated Toxicities in Older Adults with Cancer
The treatment of older adults with cancer using immune checkpoint inhibitors presents a unique set of challenges. While the therapeutic benefits of ICIs are substantial, older patients are at increased risk of immune-related adverse events and treatment complications due to their frailty, comorbidities, and age-related physiological changes. The management of these patients requires a personalized, multidisciplinary approach, including comprehensive geriatric assessments to guide treatment decisions and optimize outcomes.
- Immune-related adverse events (irAEs): Older adults experience irAEs at rates similar to younger patients, but the impact is more profound due to frailty and comorbidities.
- Corticosteroid-related risks: Prolonged use of corticosteroids in older adults can lead to significant side effects, including infections, hyperglycemia, psychiatric symptoms, and osteopenia.
- Multidisciplinary approach: Incorporating geriatric assessments and multidisciplinary care can improve the management of immune-related adverse events and overall outcomes.
- Infection risks: Older patients have a heightened risk of infections, especially when high-dose corticosteroids or immunosuppressive therapies are used. Prophylactic measures, including antiviral and antibacterial agents, are recommended.
- Frailty: Frailty, rather than chronological age, is a key factor influencing treatment outcomes and susceptibility to adverse events.
Key Takeaway Messages
- Geriatric assessments are essential for older adults starting ICI therapy. These assessments should evaluate frailty, functional independence, cognitive status, and comorbidities to guide treatment decisions effectively.
- Personalized treatment plans that account for comorbidities and frailty are critical. Age alone should not dictate treatment decisions; instead, a holistic approach, including shared decision-making with patients and caregivers, is vital for optimizing outcomes.
- Multidisciplinary care involving geriatricians, oncologists, physiotherapists, dietitians, and other specialists can enhance the management of immune-related adverse events and help mitigate their impact on the patient’s quality of life.
- Monitoring and management of common comorbidities such as diabetes, osteoporosis, and hypertension are essential during ICI treatment to prevent exacerbating existing conditions.
- Prophylactic interventions, such as antiviral therapy and trimethoprim–sulfamethoxazole for patients on prolonged corticosteroid therapy, should be considered in older patients to prevent severe infections.
Older patients often experience the same rate of immune-related adverse events as younger individuals, but the consequences can be more severe due to existing health issues. Close monitoring, tailored management strategies, and prophylactic treatments are essential for reducing risks. Furthermore, a shift in focus from chronological age to a more holistic evaluation of the patient’s overall health status, including their functional and cognitive abilities, will help ensure that treatment plans align with patient preferences and quality of life considerations.
In conclusion, the integration of geriatric assessments into the management of older adults undergoing immunotherapy can lead to improved outcomes and better quality of life. Further research into the specific challenges faced by frail older adults receiving ICIs is necessary to refine treatment protocols and ensure that this vulnerable population benefits from the advances in cancer immunotherapy.
You can read the full article here
Written by Sona Karamyan, MD
-
Challenging the Status Quo in Colorectal Cancer 2024
December 6-8, 2024
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023
