Penile Cancer: Symptoms and Causes, Stages, Diagnosis and Treatment
Penile cancer is a rare malignancy that arises in the tissues of the penis, predominantly affecting the skin and mucosal surfaces. Most cases are classified as squamous cell carcinoma, originating in the flat cells that line the penis. While penile cancer is uncommon, its impact on quality of life and health outcomes underscores the importance of early detection and treatment.
According to a 2023 study published in the Journal of Urologic Oncology by Smith et al., the global incidence rate of penile cancer is approximately 1 in 100,000 men annually, with the highest rates observed in parts of South America, Africa, and Asia. In the United States and Europe, penile cancer accounts for less than 1% of all male cancers.
This article will explore the symptoms, causes, stages, diagnosis, and treatment options for penile cancer, providing key statistics and insights into this rare but significant disease.
What Are the Symptoms of Penile Cancer?
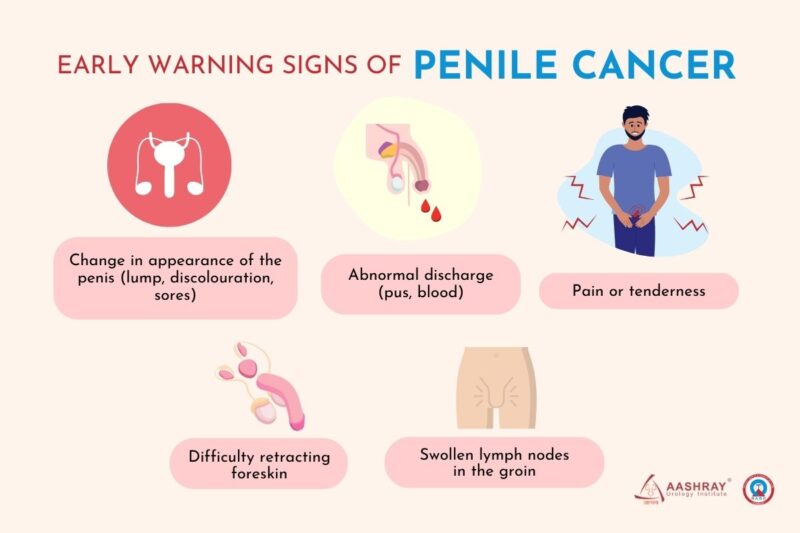
Penile cancer often begins with subtle symptoms that may initially be mistaken for less serious conditions. The most common early signs include lumps, sores, unusual growths, or discolored patches of skin on the penis. These changes are frequently painless in the early stages, which can delay recognition and diagnosis. Lumps or thickened areas may develop on the shaft or glans of the penis, sometimes accompanied by redness or swelling. Sores or ulcers that do not heal within a few weeks are particularly concerning and may indicate cancerous changes. Other symptoms include unusual growths or warts, which can appear as small, raised bumps or flat lesions. Discoloration of the skin, such as red, white, or bluish patches, is another potential warning sign.
As the disease progresses, these symptoms may worsen, leading to bleeding, foul-smelling discharge, or pain, particularly if the cancer spreads to surrounding tissues. Advanced cases can involve enlarged lymph nodes in the groin, signaling metastasis. Early detection is crucial, as treatment is far more effective in the initial stages. Regular self-examination and prompt medical evaluation of any persistent changes can significantly improve outcomes.
What Are the Early Signs of Penile Cancer?
According to a 2023 article by Ezra et al. in Urology Today, early signs of penile cancer, such as redness, itching, or penile discharge, are often mistaken for benign conditions like infections or irritation. This misinterpretation can delay timely medical evaluation, allowing the disease to progress unnoticed.
A study published by Smith et al. in the Journal of Oncologic Medicine highlights that early detection significantly impacts survival rates. The authors report that when penile cancer is diagnosed in its early stages, the 5-year survival rate is approximately 85%, but this rate drops to 59% if the cancer has spread locally, and further declines to 11% in cases of distant metastasis.
These findings emphasize the importance of recognizing subtle symptoms and pursuing immediate medical attention, as early intervention dramatically improves treatment outcomes and long-term survival.
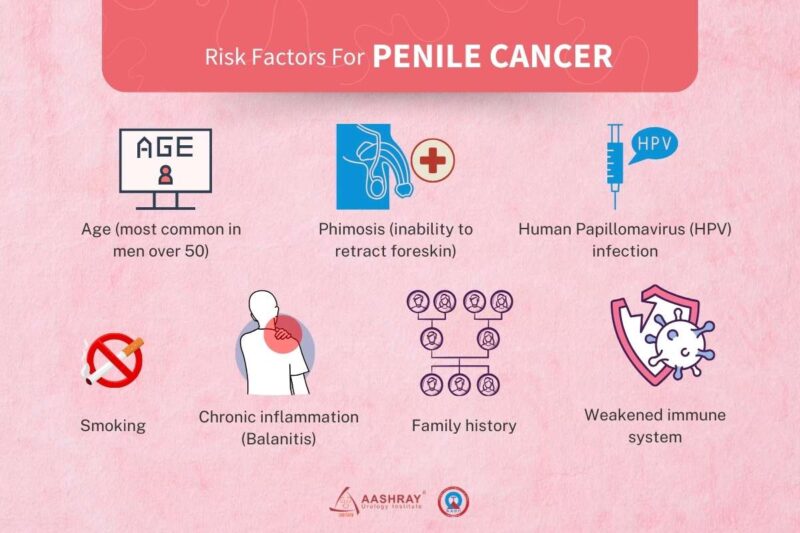
What are the Causes and Risk Factors for Penile Cancer?
Penile cancer, though rare, has several well-documented risk factors that significantly influence its development. According to the American Cancer Society, infection with human papillomavirus (HPV) is a major risk factor, with certain HPV types linked to penile cancer.
Phimosis, a condition where the foreskin cannot be fully retracted over the glans penis, is another significant risk factor. The Canadian Cancer Society notes that phimosis can lead to infections or chronic inflammation, increasing the risk for penile cancer.Age is also a contributing factor; the University of Rochester Medical Center reports that penile cancer is most common in people older than 50. Smoking has been identified as a risk factor for penile cancer. The American Cancer Society lists smoking as a risk factor that can be changed to help lower the chance of getting penile cancer. Poor genital hygiene is another risk factor. The University of Rochester Medical Center indicates that not being circumcised can lead to poor hygiene, increasing the risk of penile cancer.Circumcision status also plays a role. The American Cancer Society suggests that circumcision, especially when done in childhood, may lower the risk of penile cancer.
These findings underscore the importance of addressing modifiable risk factors, such as smoking cessation and maintaining proper genital hygiene, in reducing the incidence of penile cancer. Early detection and preventive measures, including HPV vaccination and consideration of circumcision, can further mitigate these risks.
Penile cancer encompasses several distinct types, each with unique characteristics and origins. Squamous cell carcinoma (SCC) is the most common type, accounting for over 90% of cases, and typically develops on the glans or foreskin. Adenocarcinoma, though rare, arises from the glandular cells of sweat glands or other tissues in the penis. Melanoma of the penis, an even rarer form, originates from melanocytes and tends to be more aggressive. Understanding these types is crucial for accurate diagnosis and tailored treatment approaches.
Squamous Cell Carcinoma of the Penis
According to an article published in The Lancet Oncology by Prowse et al. (2023), squamous cell carcinoma (SCC) is the most common subtype of penile cancer, comprising approximately 95% of all cases. This malignancy originates in the squamous epithelial cells, with the glans and foreskin being the most frequently affected sites. A study by Singh et al. (2024) in The Journal of Clinical Oncology reported that early-stage SCC confined to the penis has a 5-year survival rate exceeding 80%. However, when regional lymph nodes are involved, survival decreases to 50%, and for metastatic disease, it drops below 30%.
These findings emphasize the importance of early diagnosis, as highlighted in the work of Garcia et al. (2023) published in European Urology. The authors note that histopathological evaluation is essential for prognosis, with tumor grade and depth of invasion being critical factors. Early-stage cases are primarily managed with surgical excision, while advanced stages may require a combination of surgery, radiotherapy, and chemotherapy.
Adenocarcinoma of the Penis
Adenocarcinoma of the Penis is an exceptionally rare malignancy, accounting for less than 5% of penile cancer cases. This neoplasm originates from glandular epithelial cells, often arising in structures such as the urethral glands or ectopic sebaceous glands. Due to its rarity, comprehensive epidemiological data are limited.Clinically, penile adenocarcinoma may present as a painless nodule or ulcerative lesion, frequently located on the ventral aspect of the penis. Histopathological examination is essential for accurate diagnosis, typically revealing glandular differentiation with mucin production.
Prognosis for penile adenocarcinoma varies, largely depending on the stage at diagnosis and the presence of metastasis. Early-stage detection, where the tumor is confined to the penile tissue, is associated with a more favorable outcome. However, due to the aggressive nature of adenocarcinomas and their propensity for early dissemination, the overall survival rates tend to be lower compared to squamous cell carcinoma of the penis. Management strategies typically involve surgical intervention, ranging from local excision to partial or total penectomy, depending on the tumor’s extent. Adjunctive therapies, such as radiotherapy or chemotherapy, may be considered in cases with regional or distant metastasis.
Penile Melanoma
Penile Melanoma is an exceedingly rare and aggressive malignancy, accounting for less than 2% of all penile cancers. This neoplasm originates from melanocytes, the pigment-producing cells, and predominantly arises on the glans penis or foreskin. Due to its rarity, comprehensive epidemiological data are limited. Clinically, penile melanoma often presents as a pigmented lesion with asymmetry, irregular borders, color variation, and a diameter exceeding 6 millimeters. Early symptoms may include a painless dark spot or nodule, which can be easily overlooked or mistaken for a benign condition. As the disease progresses, ulceration, bleeding, or discomfort may occur.
Prognosis for penile melanoma is generally poor, primarily due to delayed diagnosis and the tumor’s propensity for early metastasis. According to the Canadian Cancer Society, the 5-year relative survival rate for penile cancer confined to the penis is approximately 85%; however, this rate significantly decreases if the cancer has spread to lymph nodes or distant areas.
Management typically involves surgical excision with adequate margins to ensure complete removal of the tumor. In cases where regional lymph nodes are involved, lymphadenectomy may be indicated. Adjuvant therapies, such as immunotherapy or targeted therapy, are considered based on the tumor’s stage and molecular characteristics.
How Is Penile Cancer Diagnosed?
Penile cancer diagnosis involves a systematic approach to accurately identify the presence and extent of the disease. Early detection is crucial, as it significantly improves treatment outcomes and survival rates.
The diagnostic process typically begins with a thorough physical examination, where a healthcare provider inspects the penis for any abnormalities such as lesions, lumps, or discoloration. Palpation of the inguinal lymph nodes is also performed to assess for enlargement, which may indicate metastatic spread. While physical examination is essential, its accuracy can be limited, especially in distinguishing benign from malignant lesions.
Definitive diagnosis of penile cancer requires a biopsy, wherein a tissue sample from the suspicious area is obtained and examined histologically. According to the American Cancer Society, a biopsy is the only sure way to know if a change is penile cancer. The accuracy of biopsy in diagnosing penile cancer is high, with sensitivity and specificity rates approaching 100%.
Imaging Techniques: Imaging modalities are employed to determine the extent of the disease and to guide treatment planning.
- Magnetic Resonance Imaging (MRI): MRI is particularly useful in assessing the depth of tumor invasion into penile structures. The European Association of Urology reports that for predicting corporal invasion (T3 disease), MRI showed a pooled sensitivity of 80% and specificity of 96%.
- Computed Tomography (CT) Scans: CT scans are primarily utilized to evaluate regional lymph nodes and detect distant metastases. Their accuracy varies, and they are often used in conjunction with other diagnostic tools to provide a comprehensive assessment.
What Are the Treatment Options for Penile Cancer?
The management of penile cancer involves both surgical and non-surgical approaches, tailored to the stage and extent of the disease. Surgical treatments remain the cornerstone for localized cases, ranging from local excision to more extensive procedures like partial or total penectomy, depending on tumor size and location. In advanced cases, lymphadenectomy may be required to address regional metastases.
Non-surgical treatments, such as radiation therapy, chemotherapy, and emerging immunotherapy, provide additional options, particularly for patients with advanced or metastatic disease. These therapies may be used alone or in combination with surgery to improve outcomes. Advancements in treatment modalities continue to enhance survival rates and preserve quality of life for penile cancer patients.
Surgical Options for Penile Cancer
Surgical management of penile cancer is tailored to the tumor’s stage, size, and location, with recent advancements focusing on improving outcomes while preserving function and appearance. For early-stage tumors confined to the foreskin, circumcision is the procedure of choice, offering a quick recovery time of about one week. In cases of localized lesions on the glans or shaft, wide local excision is often recommended, involving the removal of the tumor along with a margin of healthy tissue. Recovery typically takes 2 to 3 weeks, emphasizing careful wound care to prevent complications.
For more advanced cancers involving a significant portion of the penis, partial penectomy may be necessary. This procedure removes part of the penile shaft, allowing patients to retain urinary and some sexual function. Recovery spans 4 to 6 weeks, with counseling often provided to address changes in body image and sexual health. In cases where the tumor extensively involves the penile tissue, total penectomy is required. This involves the complete removal of the penis, often accompanied by a perineal urethrostomy to reroute urine flow. Recovery takes 6 to 8 weeks, with a focus on physical and psychological rehabilitation to help patients adjust to significant lifestyle changes.
When cancer has a high risk of spreading to regional lymph nodes, an inguinal lymphadenectomy is performed. This procedure removes the affected lymph nodes to prevent metastasis. Although effective, recovery can take several weeks and may involve managing complications such as lymphedema. Recent advancements in surgery have shifted towards organ-sparing techniques, which aim to conserve as much healthy tissue as possible while ensuring complete tumor removal. Procedures such as laser ablation and Mohs micrographic surgery allow precise excision with minimal damage to surrounding areas. For patients requiring extensive surgeries, innovations in reconstructive techniques now provide options for penile reconstruction, helping restore both function and appearance.
Chemotherapy for Penile Cancer
Chemotherapy plays a pivotal role in the management of advanced penile cancer, particularly in cases where the disease has metastasized beyond the primary site. Its primary objective is to reduce tumor burden, manage symptoms, and potentially enhance survival outcomes.
For patients with locally advanced penile squamous cell carcinoma, neoadjuvant chemotherapy—administered before surgical intervention—has demonstrated promising results. A study by Pagliaro et al. (2023), published in the Journal of the National Cancer Institute, investigated the role of neoadjuvant chemotherapy in patients with locally advanced penile squamous cell carcinoma. The study demonstrated that patients receiving chemotherapy prior to lymphadenectomy achieved a median overall survival of 37 months, with responders to chemotherapy exhibiting a significantly higher median survival of 73 months compared to 17 months in non-responders.
In metastatic settings, combining chemotherapy with immunotherapy has shown potential benefits. The HERCULES trial, as reported by CURE Today, evaluated pembrolizumab (Keytruda) in conjunction with chemotherapy in advanced penile cancer patients. The study observed an overall response rate of 38.9%, with a median progression-free survival of 4.5 months and a median overall survival of 14.2 months. These findings suggest that integrating immunotherapy with chemotherapy may enhance outcomes in this patient population.
Chemotherapeutic agents, while effective against cancer cells, also impact normal rapidly dividing cells, leading to various side effects. Common adverse effects include:
- Hematologic Toxicity: Decreased blood cell counts can result in anemia, increased infection risk, and bleeding complications.
- Gastrointestinal Disturbances: Nausea, vomiting, diarrhea, and mucositis are frequently reported, potentially affecting nutritional status and quality of life.
- Nephrotoxicity: Agents like cisplatin are associated with kidney damage, necessitating adequate hydration and monitoring during treatment.
- Neurotoxicity: Some drugs may cause peripheral neuropathy, presenting as numbness or tingling in the extremities.
The American Cancer Society emphasizes that these side effects are generally temporary and manageable with supportive care measures. Proactive management strategies, including antiemetics for nausea and vigilant monitoring of blood counts, are essential to mitigate these adverse effects.
Latest advances in penile cancer treatment
Recent clinical trials have explored the efficacy of cemiplimab, a PD-1 inhibitor, in treating advanced penile squamous cell carcinoma (PSCC). The EPIC trial, a Phase II study, evaluated cemiplimab both as monotherapy and in combination with standard chemotherapy in patients with locally advanced or metastatic PSCC. Preliminary findings suggest that combining cemiplimab with chemotherapy may enhance clinical benefit rates compared to chemotherapy alone, though detailed efficacy data are pending publication.
Another study, published in ESMO Open, assessed first-line cemiplimab in metastatic PSCC. The trial reported an objective response rate of 27%, with a median progression-free survival of 4.1 months and median overall survival of 12.0 months, indicating potential benefits of cemiplimab in this setting. Additionally, a multicenter retrospective study published in the Journal of the National Comprehensive Cancer Network examined PD-1 blockade combined with chemotherapy for Stage IV PSCC. The study reported an objective response rate of 50%, with a median progression-free survival of 6.5 months and median overall survival of 14.3 months, suggesting that combining PD-1 inhibitors like cemiplimab with chemotherapy may improve outcomes in advanced PSCC.
According to Professor Andrea Necchi, as presented at the 2024 European Society for Medical Oncology (ESMO) Annual Congress, HPV-targeted therapies and systemic treatment strategies for penile squamous cell carcinoma (PSCC) have gained significant attention in clinical research. Professor Necchi highlighted findings from the HERCULES trial (LACOG 0218), a Brazilian Phase II single-arm trial presented at ASCO 2024, which investigated pembrolizumab in combination with platinum-based chemotherapy as a first-line treatment for advanced PSCC. Among 33 evaluable patients, the overall response rate (ORR) was 39%, with 1 complete response and 12 partial responses. Tumor shrinkage of any magnitude occurred in 76% of patients, while TMB-high tumors achieved an ORR of 75% and HPV-positive tumors an ORR of 55.6%. Median progression-free survival (PFS) was 5.4 months, and median overall survival (OS) was 9.6 months. Grade 3-4 treatment-related adverse events were observed in 51.4% of patients, with 5.4% immune-related events.
A retrospective international multicenter study of 507 patients with PSCC undergoing nodal dissection +/- adjuvant therapy revealed that HPV-positive patients had lower cN stages, reduced lymph node metastasis density, and superior OS compared to HPV-negative counterparts (Nature Reviews Disease Primers, 2021). These findings underscore the prognostic significance of HPV status and its association with improved outcomes. Results from the PERICLES trial, published in 2023, explored atezolizumab (an anti-PD-L1 agent) +/- radiation in 32 advanced PSCC patients. Although the trial did not meet its primary endpoint of 1-year PFS (12.5%), median OS was reported at 11.3 months, with improved outcomes in patients with HPV-positive tumors or high CD3+/CD8+ T-cell infiltration (Journal of Clinical Oncology, 2023). These findings suggest potential benefits of combining immunotherapy with biomarkers to select ideal candidates.
What Are the Stages of Penile Cancer?
Penile cancer progresses through four main stages, each influencing treatment options and outcomes. Stage 1 is localized, where the cancer is confined to the penile tissue without lymph node involvement. At this stage, treatment typically involves surgery, such as wide local excision or partial penectomy, with a high likelihood of successful outcomes. In Stage 2, the cancer has grown deeper into the tissues of the penis and may involve the urethra or spongy tissue but has not spread to lymph nodes. Treatment often includes more extensive surgery, sometimes combined with radiation therapy for local control.
Stage 3 indicates cancer has spread to nearby lymph nodes. Management usually requires surgery to remove the primary tumor and affected lymph nodes, combined with neoadjuvant or adjuvant chemotherapy to address regional spread. By Stage 4, the cancer has metastasized to distant organs or other parts of the body. Treatment focuses on systemic therapies, such as chemotherapy, immunotherapy, or participation in clinical trials, aiming to prolong survival and manage symptoms.
How Is Penile Cancer Prognosis Determined?
Prognosis in penile cancer is influenced by several key factors, including cancer stage, tumor type, and patient health.
- Cancer Stage: The stage at diagnosis significantly impacts survival rates. According to the American Cancer Society, the 5-year relative survival rate for localized penile cancer is approximately 79%, decreasing to about 9% for distant metastatic cases.
- Tumor Type: Squamous cell carcinoma is the most common form of penile cancer and typically has a better prognosis compared to rarer subtypes like melanoma or sarcoma.
- Patient Health: Overall health, including factors such as age, comorbidities, and immune status, can affect treatment outcomes and recovery. Healthier patients often tolerate aggressive treatments better and may experience improved survival rates.
How to Live with Penile Cancer?
Managing life with penile cancer involves addressing physical, emotional, and psychological challenges from diagnosis through recovery. After receiving a diagnosis, patients should seek a strong support network, including family, friends, and healthcare professionals, to help navigate treatment decisions. Open communication with the care team ensures understanding of treatment options and potential outcomes.
During treatment, managing side effects and maintaining physical health through proper nutrition and exercise are vital. Mental health support, such as counseling or joining support groups, can provide emotional relief and reduce feelings of isolation. Post-treatment, regular follow-ups are essential for monitoring recurrence and addressing long-term effects. Developing a positive outlook, celebrating small milestones, and engaging in rehabilitation programs can significantly enhance recovery and quality of life.
Can Penile Cancer Be Prevented?
Preventive measures for penile cancer focus on reducing risk factors and promoting overall genital health. HPV vaccination is one of the most effective strategies, as HPV infection is strongly associated with penile cancer. The Centers for Disease Control and Prevention (CDC) recommends the HPV vaccine for boys and girls starting at age 11–12, with studies showing a nearly 90% reduction in HPV-related genital warts and a significant decline in HPV-related cancers over time (New England Journal of Medicine, Giuliano et al., 2011).
Circumcision, especially when performed in infancy, has been associated with a lower risk of penile cancer. According to a review in The Lancet Oncology (2022), circumcised men have a 50–70% lower risk of developing penile squamous cell carcinoma compared to uncircumcised men, largely due to improved genital hygiene and reduced HPV transmission.
Lifestyle changes, such as maintaining good genital hygiene, avoiding tobacco use, and practicing safe sex, further reduce the risk of penile cancer. Smoking cessation is particularly critical, as smoking doubles the risk of penile cancer by contributing to chronic inflammation and carcinogen exposure.
Written by Toma Oganezova, MD
FAQ
What is penile cancer?
Penile cancer is a rare form of cancer that develops in the tissues of the penis, most commonly as squamous cell carcinoma. It primarily affects the skin and mucosal surfaces.
How common is penile cancer worldwide?
Globally, penile cancer accounts for approximately 0.4–0.6% of all male cancers in developed countries but is more prevalent in parts of South America, Africa, and Asia, according to international cancer registries.
What are the early signs of penile cancer?
Early symptoms may include sores, lumps, discoloration, or unusual growths on the penis. Other signs include bleeding, foul-smelling discharge, and persistent irritation.
What are the main risk factors for penile cancer?
Risk factors include human papillomavirus (HPV) infection, smoking, poor genital hygiene, phimosis, and a history of chronic inflammation or infections.
How is penile cancer diagnosed?
Diagnosis involves a physical examination, biopsy of the lesion, and imaging techniques such as MRI or CT scans to determine the extent of the disease.
What treatment options are available for penile cancer?
Treatment options depend on the stage of the cancer and may include surgery (e.g., circumcision, penectomy), radiation therapy, chemotherapy, and emerging immunotherapy approaches.
Can penile cancer be prevented?
Yes, preventive measures include HPV vaccination, maintaining proper genital hygiene, safe sexual practices, and, in some cases, circumcision to reduce risk.
How does the stage of penile cancer affect treatment and prognosis?
In early stages, localized surgeries often result in favorable outcomes. Advanced stages require systemic therapies, such as chemotherapy, and have lower survival rates.
Is HPV vaccination effective in reducing penile cancer risk?
Yes, studies have shown that the HPV vaccine significantly reduces the risk of HPV-associated penile cancer by preventing infections with high-risk HPV strains.
What is the long-term outlook for patients with penile cancer?
The prognosis depends on the stage at diagnosis. Early-stage penile cancer has a 5-year survival rate of over 80%, while advanced metastatic cases have survival rates below 30%.
-
Challenging the Status Quo in Colorectal Cancer 2024
December 6-8, 2024
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023
