Radiotherapy for brain tumors, also referred to as brain radiation is a cornerstone in the treatment of brain tumors. This therapy employs high-energy rays to precisely target and eliminate cancerous cells within the brain. This overview will delve into the various forms of radiotherapy utilized, discuss their effectiveness in treating brain tumors, outline potential side effects patients might experience, and highlight recent advancements that have improved outcomes and reduced complications.
What is Radiotherapy for Brain Tumor?
Radiotherapy for brain tumors is a treatment that uses controlled, high-energy beams to destroy tumor cells while minimizing harm to surrounding healthy tissue. It works by damaging the cancer cells and making it difficult for them to multiply, after which the body removes them. Healthy cells have a better ability to repair themselves from this damage. To precisely target tumors and protect healthy brain tissue, various techniques are used, including external beam radiation therapy with methods like 3D-CRT, IMRT, proton beam therapy, and stereotactic radiosurgery, which shape and aim radiation beams from multiple angles with adjustable intensity.
Internal radiation therapy (brachytherapy) involves placing radioactive material directly in or near the tumor for a concentrated dose to the cancer with less impact on distant healthy tissue.
Types of Radiotherapy for Brain Tumor
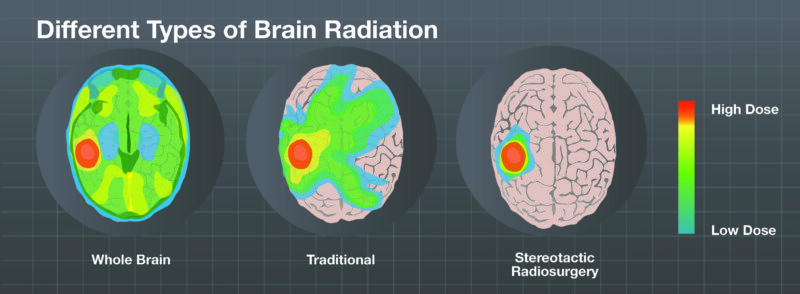
Radiotherapy for brain tumors is a crucial treatment, utilizing high-energy beams to target and destroy cancer cells. The two main categories of radiotherapy used are External Beam Radiotherapy (EBRT) and Stereotactic Radiosurgery (SRS), each with unique characteristics and applications.
External Beam Radiotherapy (EBRT)
External Beam Radiotherapy is the most common type of radiation therapy employed for brain cancer. It involves directing radiation at the tumor from a source located outside the body, much like undergoing an X-ray but with a significantly higher dose of radiation. This process typically utilizes a machine called a linear accelerator. Within EBRT, several specialized techniques exist.
Three-dimensional Conformal Radiation Therapy (3D-CRT) employs imaging scans, such as MRI and CT, in conjunction with computer software to create a detailed three-dimensional map of the tumor. This allows for the shaping of multiple radiation beams aimed at the tumor from various angles, effectively delivering a higher dose to the cancerous tissue while minimizing the radiation exposure to the surrounding healthy brain.
Intensity Modulated Radiation Therapy (IMRT) represents an advancement over 3D-CRT by enabling the adjustment of the intensity or strength of the radiation beams directed at different parts of the tumor and surrounding tissues. This capability is particularly useful for limiting the radiation dose to sensitive normal brain areas and may permit the delivery of a more potent dose to the tumor itself.
Volumetric Modulated Arc Therapy (VMAT) is a newer technique similar to IMRT; however, the radiation source rotates around the patient during treatment, delivering beams from multiple angles. This approach may offer the benefit of shorter overall treatment sessions. Conformal Proton Beam Radiation Therapy utilizes beams of protons instead of traditional X-rays. Protons have the unique property of releasing most of their energy after traveling a specific distance, which can result in less damage to the tissues the beam passes through before reaching the tumor.
This method may be particularly advantageous for treating brain tumors with distinct edges. Finally, Whole Brain and Spinal Cord Radiation Therapy, also known as craniospinal radiation, is indicated when there is evidence that the tumor has spread along the membranes covering the spinal cord or into the cerebrospinal fluid. This type of radiation is often necessary for certain types of tumors that have a higher propensity to spread in this manner.
Stereotactic Radiosurgery (SRS)
Stereotactic Radiosurgery is a treatment method that delivers a large, highly precise dose of radiation to a small, well-defined tumor area in a single session. Despite its name, it does not involve any actual surgical cutting. Stereotactic Radiotherapy (SRT) is a similar technique that delivers the radiation dose in a few separate sessions, rather than just one. These approaches may be considered for tumors located in areas of the brain or spinal cord that are not amenable to traditional surgery, or when a patient’s overall health makes surgery too risky.
The goal is to target the tumor with a high dose of radiation while significantly limiting the exposure to the surrounding normal brain tissue. This precise radiation delivery can be achieved through different methods. One involves focusing numerous thin beams of radiation from hundreds of different angles to converge precisely at the tumor.
The Gamma Knife is a well-known machine that utilizes this technique. Another method employs a computer-controlled, movable linear accelerator. Instead of delivering many beams simultaneously, this machine moves around the patient’s head to deliver radiation to the tumor from a multitude of different angles. Machines like CyberKnife and Clinac are examples of systems that deliver stereotactic radiosurgery in this way. Stereotactic Radiotherapy, with its fractionated approach, can be more suitable for treating larger tumors or tumors located very close to critical brain structures that might not tolerate a large single dose of radiation.
Nikitas et al. (2020) in Clinical and Translational Radiation Oncology investigated synchronous thoracic SBRT and brain SRS for oligometastatic NSCLC. In 6 patients with 1-3 brain metastases, median overall survival was 12.4 months, with a 1-year OS of 67%, 1-year freedom from progression of 17%, and 1-year local control of 100%. Brain disease 1-year local control was 80% and 1-year freedom from progression was 53%. The study concluded that this local therapy approach achieves good local control and encouraging overall survival for patients with oligometastatic lung cancer limited to the brain.
How Effective is Radiotherapy for Brain Tumor?
Jalali et al. (2017) published in JAMA Oncology a phase 3 trial comparing stereotactic conformal radiotherapy (SCRT) to conventional radiotherapy (ConvRT) in 200 young patients with benign or low-grade brain tumors. 1 Over 5 years, SCRT resulted in significantly superior mean full-scale and performance IQ scores (p=0.04 and p=0.046, respectively) and a significantly lower cumulative incidence of new neuroendocrine dysfunction (31% vs 51%; p=0.01). 1 Five-year overall survival was 86% for SCRT and 91% for ConvRT (p=0.54). The study concluded that SCRT led to better neurocognitive and endocrine outcomes compared to ConvRT. 2.
What are the Side Effects of Radiotherapy for Brain Tumor?
Radiotherapy for brain tumors, while a powerful treatment, can cause side effects as it affects both tumor cells and healthy brain tissue. These side effects can be generally grouped into those that appear shortly after treatment begins and those that may develop over a longer period.
Lawrie et al. (2019) published a Cochrane Library review focused on radiotherapy for brain tumors, specifically examining nine studies (2406 participants initially) comparing different radiotherapy approaches for glioma. The review found evidence of low to very low certainty due to risk of bias and data paucity, preventing meta-analysis. One study suggested a greater risk of cognitive impairment with radiotherapy versus no adjuvant treatment at 12 years (RR 1.95, CI 1.02 to 3.71; n=65). No clear difference was found between radiotherapy and chemotherapy for cognitive impairment up to three years (n=117).
A small subgroup analysis suggested less neurocognitive impairment with stereotactic conformal radiotherapy versus conventional radiotherapy at five years (0/11 vs 2/12). Chemoradiotherapy versus radiotherapy showed no clear differences in cognitive impairment or quality of life over five years. The authors concluded that the low certainty of evidence makes it difficult to draw firm conclusions.
Short-Term Side Effects
Short-term side effects of brain tumor radiotherapy are those that typically occur during or within about six weeks following the start of treatment. These can include feelings of tiredness or fatigue, increased irritability, nausea, vomiting, and headaches. Some individuals may also experience a loss of appetite and hair loss in the area of the scalp that receives radiation. Additionally, the skin on the scalp may become dry, itchy, red, or tender, indicating skin irritation.
Long-Term Side Effects
Long-term side effects of radiotherapy for brain tumors are less common than short-term effects but can emerge months or even years after the treatment has concluded. These may involve difficulties with thinking and memory, personality changes, and trouble concentrating. More specifically, individuals might experience memory loss, confusion, cataracts, or hearing difficulties. Depending on the area of the brain that was treated, there could also be a loss of specific functions such as vision, language, motor skills, or sensory perception.
In rare instances, a condition called radiation necrosis, where dead brain tissue forms at the site of the tumor, can occur. There is also a very small risk of developing a new tumor in the scalp, skull, or brain many years after the radiation therapy. Vascular issues, including stroke, are also mentioned as uncommon long-term effects. In children, radiation therapy may potentially affect the pituitary gland and other parts of the brain, possibly leading to learning problems or slowed growth and development
What is a Radiotherapy Mask for Brain Tumor?
A radiotherapy mask for a brain tumor is a custom-made device used during radiation therapy to ensure that the treatment is delivered to the precise location of the tumor each time. Its primary purpose is to keep the patient’s head completely still throughout the radiation session. This immobility is crucial for the accuracy of the treatment, as even slight movements could cause the radiation beams to miss the tumor or hit healthy brain tissue.
The mask is typically created before the actual treatment begins, during a planning session called simulation. During this session, the patient lies down on the treatment table in the position they will be in for each radiation treatment. A member of the radiation therapy team will then create a mask that is specifically molded to fit the contours of the patient’s face and head. This is often done using a warm, wet sheet of plastic mesh material that is placed over the face and shaped to the individual’s features. Once it cools and hardens, the mask becomes a rigid shell that will hold the head firmly in place during treatment sessions.
Marks may be placed on the mask to help the therapy team align the radiation beams accurately each day. During each treatment session, the patient will lie down, and the mask will be placed over their face and attached to the treatment table, ensuring that their head remains in the exact same position.

Read OncoDaily’s Special Article About Radiotherapy Masks
Palliative Radiotherapy for Brain Tumor
Radiotherapy plays a significant role in palliative care for brain tumors when a cure is not achievable. In these situations, the primary goal shifts to relieving symptoms and improving the patient’s quality of life. Radiotherapy can be very effective in achieving this by targeting the tumor to reduce its size and the pressure it exerts on the surrounding brain tissue.
For instance, in cases of secondary brain tumors, where cancer has spread to the brain from elsewhere in the body, radiotherapy is a common treatment. These tumors growing inside the brain can cause troublesome symptoms such as severe headaches, nausea, and increasing drowsiness due to the elevated pressure within the skull. Radiotherapy aims to shrink these tumors, thereby alleviating the pressure and consequently reducing these distressing symptoms. While it may take some time, often a few days or weeks, for the effects of the radiotherapy to become noticeable in terms of symptom control, it can provide significant relief for patients
Steinmann et al. (2012) published in BMC Cancer a prospective multi-center QoL study of 151 patients with brain metastases receiving palliative radiotherapy (mostly whole-brain). 1 At 3 months, QoL significantly deteriorated in global QoL, physical function, fatigue, nausea, pain, appetite loss, hair loss, drowsiness, motor dysfunction, communication deficit, and leg weakness. Headache scores remained stable despite reduced corticosteroid use. Better baseline QoL in several domains predicted 3-month survival, with lower Karnofsky score, higher age, and higher pain at baseline being prognostic of poorer survival. The study concluded that palliative radiotherapy leads to moderate QoL deterioration in the short term, and baseline QoL may offer prognostic information.
How is Radiotherapy Administered for Brain Tumor?
Radiotherapy for brain tumors is a multi-step process. It begins with a detailed planning session called simulation, where imaging scans are used to map the tumor, and a custom mask or mould is created to ensure precise head positioning during treatment. The radiation oncologist and a team of experts then design a personalized treatment plan, specifying the radiation dose and delivery method. The actual treatment involves daily sessions, typically Monday through Friday for several weeks, where the patient lies still on a treatment table while a machine called a linear accelerator delivers radiation to the tumor. Radiation therapists position the patient and operate the machine, while the radiation oncologist oversees the entire process.
Patients can expect to have an initial simulation appointment that takes a couple of hours, followed by daily treatment sessions lasting around 15 to 30 minutes, with the radiation delivery itself only taking a few minutes. The medical team will guide the patient through each step, ensuring they are comfortable and well-informed.
How Long Does It Take to See Results?
It typically takes some time to observe the effects of radiotherapy on a brain tumor. According to the provided information, it’s not immediate. Cancer cells begin to die off during the course of treatment, which can span several days to weeks. This process of cell death continues for weeks and even months after the radiotherapy sessions have concluded.
In terms of symptom relief, which is a key indicator of treatment response, it might take a few days or even weeks for patients to notice an improvement. Initially, the radiotherapy might cause some swelling in the brain, which could paradoxically lead to a temporary worsening of symptoms before they start to get better.
Following the completion of radiotherapy, regular follow-up care is essential. This usually involves periodic MRI scans, which are a primary tool for monitoring brain tumors. Doctors also conduct regular physical and neurological examinations and may order blood tests. In some cases, other types of imaging, such as MR spectroscopy, perfusion or diffusion MRI, or CT scans, might be used as well.
These follow-up assessments allow the medical team to monitor the health of the brain, check for any signs that the tumor might be returning, and identify and manage any potential side effects from the treatment. By comparing these follow-up scans and clinical evaluations over time, doctors can determine the success of the radiotherapy in controlling the tumor’s growth or causing it to shrink.
What Are the Costs of Radiotherapy for Brain Tumor?
The cost of brain tumor radiotherapy varies significantly based on the specific type of radiation used, your insurance coverage, the location of the treatment facility, the number of treatment sessions required, and additional expenses like consultations, imaging, medications, and follow-up care. It’s crucial to discuss these potential costs with your healthcare team and insurance provider to get an accurate estimate tailored to your individual situation.
Lester-Coll published in the Journal of Neurosurgery a cost-effectiveness analysis of treating up to 10 brain metastases with SRS, WBRT, or SRS+WBRT using a Markov model based on the JLGK0901 study and modified data from other trials. For 1 metastasis, ICERs were: SRS vs WBRT $117,418/QALY, SRS vs SRS+WBRT $51,348/QALY. For 2-10 metastases, ICERs were: SRS vs WBRT $123,256/QALY, SRS vs SRS+WBRT $58,903/QALY. Sensitivity analyses showed the model was sensitive to SRS cost and post-treatment utilities. The study concluded that SRS alone is the most cost-effective strategy compared to SRS+WBRT, and may be cost-effective versus WBRT depending on willingness-to-pay and SRS cost. (Year of publication not provided in the text).
Whar Are The Recent Advancements in Radiotherapy for Brain Tumors?
Chen et al. (2024) published in JAMA Oncology a randomized trial investigating induction BEEP chemotherapy followed by WBRT versus WBRT alone for breast cancer brain metastases. In 112 patients, the median brain-specific progression-free survival was 8.1 months in the BEEP arm versus 6.5 months in the WBRT arm (HR 0.71, p=0.15). While the 2-month objective response rate was not significantly different, the 8-month brain-specific PFS rate was significantly higher in the BEEP group (48.7% vs 26.3%; p=0.03). The study concluded that induction BEEP before WBRT may improve brain metastasis control.
Can All Brain Tumours Patients Receive Radiotherapy?
Radiotherapy eligibility for brain tumor patients depends on various factors. It’s often used when surgery isn’t an option or after surgery to eliminate remaining cancer cells and prevent recurrence. It can also slow tumor growth. Stereotactic radiosurgery (SRS) is typically used for smaller tumors, while stereotactic radiotherapy (SRT) might be suitable for larger tumors or those near critical brain structures. Radiotherapy is generally prescribed for radiosensitive tumors, and proton beam therapy may be preferred for tumors with distinct edges. It’s also used for brain metastases.
However, patients with cancers highly resistant to radiation might explore other treatment options. While SRT can treat larger tumors, very extensive tumors might present challenges. For tumors that heavily infiltrate normal brain tissue, the suitability of certain radiation types might be carefully considered. Prior radiation exposure is a factor that is taken into account, although re-irradiation can be an option in some cases of recurrence. Ultimately, the decision is personalized based on the tumor’s characteristics, the patient’s health, and a careful assessment of the risks and benefits.
How Can Patients Support Their Health During Radiotherapy?
To support their health during radiotherapy for a brain tumor, patients can adopt several lifestyle strategies and self-care practices, as suggested by the provided information.
Nutrition
Maintaining a healthy diet is important. Patients should follow any specific instructions given by their healthcare team regarding foods to eat or avoid. It’s also advisable to drink fluids as directed and try to maintain a stable weight throughout the treatment period.
Exercise
Engaging in a daily exercise routine that is manageable and can be sustained is recommended to help combat fatigue, a common side effect of radiation therapy. It’s important to choose activities that are tolerable for the individual.
Brain-Stimulating Activities
While not explicitly mentioned as a tip during treatment, the texts suggest that occupational or vocational therapy might be recommended as part of follow-up care, which could involve activities to stimulate cognitive functions.
Mental Health Support
Relying on the support of friends and family can be beneficial for emotional well-being during this time. Additionally, participating in support groups can provide a valuable network of individuals with shared experiences. It’s also crucial for patients to feel comfortable asking questions and discussing any concerns they may have with their healthcare team.
Expert-Recommended Self-Care Strategies
Quitting smoking is strongly advised for those who smoke. Patients should also carefully follow any instructions provided by their care team for looking after their skin in the areas receiving radiation. It’s important to promptly inform the medical team about any side effects experienced or any pain. The healthcare team may also recommend home care services, pain management strategies, and physical therapy as part of the overall care plan.
Written by Aren Karapetyan, MD
FAQ
What is radiotherapy for brain tumors?
Radiotherapy uses controlled high-energy beams to damage and destroy cancer cells in the brain.
When might radiotherapy be used to treat a brain tumor?
It can be used after surgery, as the main treatment if surgery isn't possible, or to help relieve symptoms.
What are the main types of radiotherapy for brain tumors?
The primary types are external beam radiation therapy (EBRT), where radiation comes from outside the body, and stereotactic radiosurgery (SRS), which delivers a high dose to a small area.
How effective is radiotherapy for brain tumors?
Radiotherapy aims to shrink tumors, control their growth, kill remaining cancer cells after surgery, and relieve symptoms.
What are some common short-term side effects of brain radiotherapy?
Short-term side effects can include fatigue, headaches, nausea, and hair loss.
What are some potential long-term side effects?
Long-term side effects might include memory problems, personality changes, or difficulties with concentration.
What is a radiotherapy mask and why is it used?
A radiotherapy mask is a custom-made device that holds the head still during treatment to ensure the radiation is precisely targeted.
How long does it take to see results from brain radiotherapy?
It can take days or weeks for cancer cells to start dying, and this continues for weeks or months after treatment ends. Symptom relief may also take days or weeks.
Can all brain tumor patients receive radiotherapy?
Eligibility depends on factors like tumor type, size, location, patient health, and prior radiation exposure.
How can patients support their health during brain radiotherapy?
Patients can support their health by eating a healthy diet, engaging in tolerable exercise, following skin care instructions, and seeking support from friends, family, or support groups.