
What Is Proton Beam Therapy and How It Works? Pros and Cons
Proton beam therapy (PBT) is an advanced type of radiation therapy that uses protons instead of traditional X-rays to target and treat cancer. Unlike conventional radiation, protons deliver energy directly to the tumor with remarkable precision, sparing surrounding healthy tissues and reducing the risk of side effects. This approach is particularly beneficial for treating cancers near critical organs or in pediatric patients, where minimizing long-term damage is crucial.
What Is Proton Beam Therapy?
Proton beam therapy is an advanced form of radiation treatment that utilizes protons—positively charged particles This type of therapy aims to destroy cancer cells by damaging their DNA, a process similar to other forms of radiation therapy.
How Proton Therapy Works
Proton therapy works by directing proton particles towards the tumor. Unlike X-rays, which continue to release radiation beyond the tumor site, protons release their energy only at a specific depth, directly within the tumor. This targeted approach allows the radiation to be precisely delivered to the cancer cells, minimizing damage to the healthy surrounding tissues. As a result, proton therapy can reduce radiation exposure to healthy organs and tissues, lower the risk of potential side effects, and be especially beneficial for tumors near critical structures, such as the brain or heart.
Common Uses of Proton Therapy
Proton therapy can deliver high doses of radiation to the prostate while protecting nearby organs like the bladder and rectum. Children’s developing bodies are more sensitive to radiation, making proton therapy a valuable option to minimize long-term risks like growth issues, heart disease, or secondary cancers.
The process of delivering radiation to a patient who has already received radiation therapy in the past, typically for a recurrence of cancer. Proton therapy is especially beneficial for reirradiation cases, as it allows doctors to deliver radiation to areas previously treated with minimal risk of further damage to surrounding healthy tissue. In cases where traditional radiation therapies are no longer an option due to prior treatments, proton therapy provides a safe alternative, especially for tumors located near critical structures like the spinal cord or brain.
How Does Proton Beam Therapy Work?
Proton therapy works by using protons—positively charged particles—to treat cancer. These protons deliver energy directly to the tumor, where it’s needed most, helping to destroy the cancer cells while causing minimal damage to surrounding healthy tissues. The key to how proton therapy works lies in a phenomenon known as the Bragg Peak.
The Bragg Peak and Proton Energy Delivery
When protons are used in radiation therapy, they have a unique behavior. As they travel through the body, they gradually lose energy. However, just before they stop, protons release a large burst of energy. This release happens at the Bragg Peak—a point where the proton deposits its maximum energy, which is exactly at the tumor site.
How it compares with X-ray radiation
X-rays, the type of radiation used in traditional therapies, deliver their energy as they pass through the body. This means that the X-rays continue to irradiate tissues both before and after the tumor, affecting healthy tissues along the way. In contrast, protons stop delivering their energy once they reach the tumor. The energy is focused on the tumor, meaning there is no radiation beyond the tumor site. This helps protect the healthy tissue surrounding the cancer, minimizing side effects.
Because proton therapy is so precise, it allows for higher doses of radiation directly to the tumor while reducing the amount of radiation to healthy tissue, which lowers the risk of side effects like fatigue, hair loss, or long-term health problems. This precision also makes proton therapy more effective for treating tumors that are difficult to reach with conventional radiation, such as those near the spine or brain.
What Are the Main Types of Proton Beam Therapy?
Proton beam therapy is a sophisticated and highly targeted cancer treatment method. There are two main types of proton therapy: Passive Scattering Proton Therapy (PSPT) and Pencil Beam Scanning (PBS). Both techniques use proton beams, but they differ in how the protons are delivered to the tumor and their precision in targeting the cancer cells.
Passive Scattering Proton Therapy (PSPT)
In PSPT, a broad proton beam is first created and then spread over a large area using a scattering device. This scattering process helps to deliver the protons to the tumor from different angles. While PSPT is still effective at treating many tumors, it is generally less precise compared to PBS. The scattering process spreads the proton beam over a wider area, which means that some healthy tissue surrounding the tumor may also receive radiation. This is not as ideal when it comes to tumors located near vital organs. PSPT is particularly useful for larger or more irregularly shaped tumors. It has been used successfully in head and neck cancers or tumors in difficult-to-reach locations where precise targeting is less critical, or where the tumor may be too large for PBS to treat effectively.
Pencil Beam Scanning (PBS)
PBS delivers protons with much more precision by using a focused proton beam that can be directed at the tumor in a very specific way. The beam is scanned across the tumor in a pencil-like fashion, layer by layer, enabling doctors to target the tumor with minimal damage to surrounding healthy tissue. PBS provides greater accuracy and control, making it the preferred option for tumors located near critical organs or for small tumors that require very precise radiation. The protons are delivered with much more focus and can be adjusted more easily to accommodate changes in the tumor’s shape or position. PBS is particularly effective for small or moving tumors, such as those in the brain, spine, or lung. Its ability to target tumors with greater precision makes it ideal for cases where minimizing damage to healthy tissues is crucial, such as when treating pediatric cancers or tumors located near vital structures.
Key Differences Between PSPT and PBS
PBS provides much greater precision in targeting tumors, making it the preferred choice for more delicate or complex treatment areas.
- PSPT is better suited for larger, less mobile tumors, or those in areas that are harder to reach with high precision.
- PBS is ideal for smaller, irregularly shaped tumors and tumors located near vital organs where minimizing damage to healthy tissue is a top priority.
Clinical Outcomes and Effectiveness
In 2020, Baumann et al. published a study in JAMA Oncology comparing proton chemoradiotherapy with conventional therapy in 1483 patients, predominantly men with a median age of 62. The study found that patients receiving proton therapy were older and had more comorbidities. They also received a lower integral radiation dose outside the target area. Despite similar baseline toxicity and performance status, proton therapy was associated with significantly fewer severe adverse events, including 90-day grade ≥3 and grade ≥2 adverse events, as well as a lower likelihood of a decline in performance status during treatment. However, there were no significant differences in disease-free or overall survival between the two treatment groups. The authors concluded that proton chemoradiotherapy was linked to fewer acute adverse events, with similar survival outcomes, and recommended prospective trials to validate these findings.
Proton Beam Therapy Side Effects: What Should You Expect?
A common side effect of proton therapy is fatigue, which can make everyday tasks feel more tiring and may lead to longer recovery times after each treatment. This fatigue typically intensifies as the treatment continues but tends to improve once the treatment course is completed. To manage fatigue, oncologists advise patients to rest regularly and avoid pushing themselves too hard. Light physical activities, such as walking, can also help boost energy levels. Like many other forms of radiation, proton therapy can cause skin irritation in the area where the beams are directed, resulting in symptoms such as redness, dryness, or itching, similar to a mild sunburn. This irritation is usually temporary and improves after treatment. To manage skin irritation, patients are often encouraged to use gentle skincare products and moisturizers to soothe the affected area. Additionally, wearing loose clothing and avoiding prolonged exposure to hot water can help minimize irritation. Nausea is a possible side effect of proton therapy, especially when the treatment area is close to the digestive system. The severity of nausea can vary depending on the type and location of the cancer being treated. To manage nausea, oncologists suggest eating small, frequent meals and drinking fluids in small amounts. Over-the-counter anti-nausea medications may provide relief, but it’s important to consult with a healthcare provider before using them.
Practical Tips for Managing Side Effects
Regular check-ins with your oncologist are key to managing any side effects that arise. They can help adjust your treatment plan, offer symptom relief options, and guide you through side effect management. Drink plenty of fluids throughout the day, especially if experiencing fatigue or nausea. Water and herbal teas are often recommended to keep hydration levels up. Eating nutrient-rich foods can help boost energy levels and support the body’s healing process. Consult a dietitian to plan meals that support your treatment and overall well-being.
Patient and Oncologist Insights: Which doctor is using treatment with proton therapies?
Radiation Oncologists emphasize the importance of precision and how proton therapy allows for higher doses of radiation to be delivered directly to tumors, which can be particularly beneficial for patients with cancers in sensitive areas. They also note that, while proton therapy is a powerful tool, it is important to consider whether it is the best option for each individual case, factoring in tumor type, location, and stage.
Many patients who have undergone proton therapy report feeling a greater sense of reassurance knowing that healthy tissue is being protected. For those with pediatric cancers, parents often appreciate the long-term benefits of reduced radiation exposure. However, they also acknowledge that accessibility and cost can be significant barriers, requiring careful consideration before choosing proton therapy.
Read more about Who is Radiation Oncologist, and what to know about your doctor: Article by OncoDaily
What Are the Risks or Complications of Proton Beam Therapy?
While proton therapy is highly precise, there remains a risk of unintended tissue damage if the proton beam is not accurately targeted. Even small deviations in positioning can lead to radiation exposure to healthy tissues near the tumor, especially when the tumor is close to sensitive organs or structures, such as the brain, spinal cord, or chest organs. However, advanced planning and imaging techniques are used to minimize this risk and ensure the best possible outcomes. As with any form of radiation therapy, there is a potential risk of developing secondary cancers years after treatment. This is due to the DNA damage that radiation can cause, which may lead to mutations in healthy cells. However, proton therapy reduces the overall radiation dose to surrounding healthy tissues, which lowers the risk of secondary cancers compared to traditional X-ray radiation, where the exposure extends beyond the tumor. Even though proton therapy is less likely to cause side effects compared to traditional radiotherapy, some common, short-term side effects can still occur, such as fatigue, nausea, and skin irritation. In some cases, depending on the treatment area, patients may also experience swelling, inflammation, or tenderness in the treated area. These side effects are typically temporary and can be managed with supportive care. Although proton therapy aims to minimize long-term damage, there may be concerns about delayed effects, particularly for pediatric patients. In children, radiation to growing tissues can still cause growth issues or developmental delays, even with reduced radiation exposure. However, proton therapy is still considered safer for children than traditional radiotherapy due to its precision. Proton therapy is a relatively newer treatment compared to traditional radiation techniques, and while studies have demonstrated its effectiveness and lower side effect profile, long-term data is still being collected. It is important for patients to discuss the potential long-term effects with their oncology team before undergoing treatment.
What Types of Cancer Are Treated with Proton Beam Therapy?
Proton therapy is an advanced form of radiation treatment that has shown success in treating a wide range of cancers, especially those located near sensitive or hard-to-reach areas. Its ability to precisely deliver radiation while minimizing damage to healthy tissues makes it a valuable treatment option for various types of cancer, particularly those that are difficult to treat with traditional radiation.
Brain Tumors: Proton therapy is particularly beneficial for treating brain tumors due to its ability to target the tumor with high precision, reducing the risk of damage to surrounding healthy brain tissue. . Proton therapy has been used effectively to treat both primary brain tumors (e.g., gliomas, meningiomas) and metastatic brain tumors, achieving favorable clinical outcomes with minimal cognitive side effects.
Prostate Cancer: Proton therapy is increasingly used to treat prostate cancer, offering the ability to deliver high doses of radiation directly to the prostate while sparing surrounding tissues like the bladder and rectum. Clinical studies have shown that proton therapy can reduce the likelihood of side effects such as urinary incontinence and erectile dysfunction when compared to traditional X-ray radiation.
Head and Neck Cancers: Proton therapy is highly effective for treating head and neck cancers, including cancers of the throat, mouth, and larynx. Its precision allows doctors to target tumors in these delicate areas while avoiding radiation exposure to critical structures like the salivary glands, spinal cord, and jawbone. Proton therapy has been associated with fewer side effects such as dry mouth, swallowing difficulties, and damage to healthy tissues when compared to conventional radiation.
Pediatric Cancers: Children are particularly sensitive to radiation, and proton therapy has been shown to be a safer option for pediatric cancers. Due to the growing tissues in children’s bodies, traditional radiation therapies can lead to long-term developmental and growth issues. Proton therapy minimizes the radiation dose to healthy tissues, thus reducing these risks. Proton therapy is used for various pediatric cancers, including brain tumors, spinal cord tumors, and soft tissue sarcomas, offering excellent results with fewer long-term side effects.
Other Cancer Types Treated with Proton Therapy
Lung Cancer: Proton therapy can be used to treat lung cancer, particularly in patients with tumors located near critical structures such as the heart or spinal cord.
Liver Cancer: Proton therapy is increasingly being used for liver cancers, especially in cases where tumors are near vital organs.
Spinal Cord Tumors: Proton therapy is one of the most effective options for treating spinal cord tumors. Given the close proximity of the spinal cord to other critical structures, proton therapy allows for highly targeted treatment that minimizes radiation exposure to healthy tissues surrounding the spine.
Esophageal Cancer: Proton therapy has proven beneficial in treating esophageal cancer, especially for patients with tumors located near the heart, lungs, or spine. Its ability to precisely target the tumor reduces the risk of damage to these organ
Pediatric Cancer and Proton Beam Therapy
Pediatric cancers require special consideration due to the sensitivity of children’s developing bodies to radiation. Proton therapy has become an invaluable tool in treating pediatric cancers, offering precise targeting of tumors while significantly minimizing the risk of long-term damage to healthy tissues. Here are some of the key benefits of proton therapy for pediatric cancer patients. Proton therapy allows for highly targeted treatment, which reduces the exposure of surrounding healthy tissues to radiation. This is especially important in pediatric patients, as their bodies are still developing, and traditional radiation can interfere with growth, bone development, and organ function. Children are at a higher risk of developing secondary cancers later in life when exposed to radiation. Proton therapy is particularly effective for treating brain and spinal cord tumors, which are more common in pediatric cancer patients. Traditional radiation methods can cause significant damage to the surrounding brain or spinal cord tissue, leading to cognitive or neurological issues. In children, organs such as the heart, lungs, and reproductive organs are still developing. Proton therapy targets tumors with minimal radiation exposure to these organs, reducing the risk of long-term damage that could interfere with growth and development.
Improved Quality of Life
Proton therapy generally results in fewer short-term side effects such as nausea, fatigue, and skin irritation when compared to traditional radiation. This can make the treatment process less distressing for young patients, helping them maintain a higher quality of life during their cancer treatment. Because proton therapy is more precise, the recovery time for pediatric patients is often quicker than with traditional radiation treatments, which may mean less time in the hospital and a faster return to normal activities.
Better Control of Complex or Hard-to-Reach Tumors
Proton therapy can be used to treat tumors in hard-to-reach locations, such as near the brainstem, spine, or in the eye socket, with high precision. This level of accuracy ensures that radiation is directed only at the tumor, sparing surrounding critical structures and reducing the risk of complications. For children with cancer that has spread to multiple areas, proton therapy can be used to target multiple tumor sites with minimal impact on surrounding healthy tissue, reducing the risk of complications in vital organs.
Reduction in the Risk of Cognitive or Cognitive-Related Issues
Children’s brains are particularly vulnerable to the effects of radiation. Proton therapy has been shown to help preserve cognitive function by minimizing the radiation dose to healthy brain tissues. This is crucial for helping pediatric patients maintain cognitive abilities and quality of life after treatment.
Proton Therapy for Head and Neck Cancer
Head and neck cancers, which affect areas like the mouth, throat, larynx, and sinuses, are often challenging to treat due to the proximity of vital structures such as the eyes, ears, and salivary glands. Proton therapy has emerged as an effective treatment option for these types of cancers, offering distinct advantages over traditional radiation methods. The ability to minimize damage to surrounding healthy tissue is crucial in head and neck cancer treatments, where even small radiation doses to normal structures can lead to significant complications. This is particularly important in head and neck cancer treatment, where organs like the brain, eyes, and salivary glands are at risk. Proton therapy helps avoid collateral damage to these critical structures, which can result in fewer side effects and better functional preservation. Traditional X-ray radiation can result in significant side effects such as dry mouth, difficulty swallowing, or damage to the skin, as these sensitive areas receive radiation unintentionally. One of the most common issues for patients undergoing head and neck radiation is the damage to salivary glands, which can lead to long-term dry mouth (xerostomia). Head and neck cancers can result in serious long-term complications if treated with conventional radiation, such as difficulty swallowing, changes in taste, and permanent scarring. Proton therapy has been shown to reduce these risks, leading to fewer complications both during and after treatment.
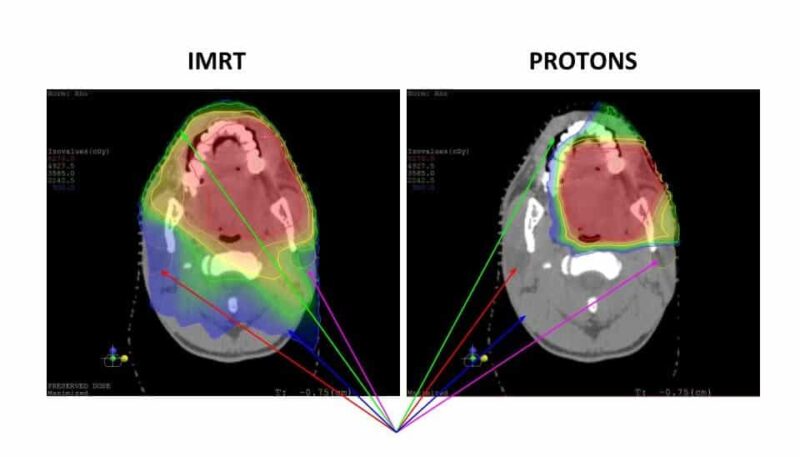
source: www.okcproton.com
How to Prepare for Proton Beam Therapy
Preparing for proton therapy is an essential part of ensuring that the treatment is as effective as possible. Proton therapy requires meticulous planning to precisely target the tumor and avoid surrounding healthy tissue. Here’s a practical guide on what to expect during the preparation process. Before beginning proton therapy, patients undergo several imaging scans to help the medical team accurately locate the tumor and plan the radiation dose. CT scans are typically used to create detailed images of the area where radiation will be delivered, ensuring precise tumor targeting. In some cases, especially for tumors in soft tissues like the brain or spinal cord, an MRI scan may be necessary. MRI scans provide detailed images of soft tissues, helping to assess the tumor’s size, shape, and position. These scans are essential for tailoring the treatment plan and ensuring the proton beam is delivered with accuracy.
What to Wear
Patients should wear comfortable, loose-fitting clothes to their appointments. This will make it easier for them to change in and out of treatment gowns if necessary. It’s important that the clothing does not interfere with the positioning process, especially if the tumor is located in a specific part of the body that requires a precise setup.
Patient Positioning for Accurate Treatment
Accurate positioning is one of the most important steps in proton therapy. The team will work to ensure the patient is in the correct position for each treatment session. Depending on the area being treated, the patient may be placed in a mold or immobilizing device to ensure they remain still during the procedure. This helps avoid any shifts in the tumor’s position during treatment. Tiny markers or tattoos may be applied to the skin as reference points for alignment during treatment. These marks ensure that the tumor is targeted accurately every time. In some cases, the treatment team will design personalized supports to keep the patient in the ideal position during each session. The goal is to replicate the exact position used during the planning scans to maintain treatment precision.
Mental and Emotional Preparation
Patients should ask their medical team any questions they may have about the procedure. Understanding how the therapy works, how long each session will take, and what to expect will help reduce anxiety. Since patients must remain still during the treatment, relaxation techniques such as deep breathing exercises or meditation can help manage stress and improve focus. Having loved ones provide emotional support during the preparation process can be reassuring. Some centers may also have counseling services to assist patients in coping with the emotional aspects of cancer treatment.
How Proton Beam Therapy Is Performed
Proton beam therapy is a highly specialized treatment that targets tumors with precision, delivering protons directly to cancer cells while minimizing damage to healthy tissue. Here’s a step-by-step breakdown of how the procedure is performed, from patient setup to the delivery of the proton beam.
Patient Setup
The treatment session begins with the patient arriving at the proton therapy facility. The patient is positioned on a treatment table, often with the help of an immobilization device (such as a mask for head and neck cancers or a body mold for other areas) to keep them in a precise position. Small, permanent marks may be placed on the skin to ensure that the patient remains in the same position for each treatment. These reference points are critical for accurate delivery.
Imaging and Alignment
Before delivering the proton beam, imaging scans like CT or MRI are used to verify the tumor’s correct positioning. The treatment team will align the patient’s body according to the reference marks or scans from the planning stage to ensure precise targeting of the tumor. The machine may make small adjustments to fine-tune the patient’s position, ensuring that the tumor receives the appropriate radiation dose while minimizing exposure to surrounding healthy tissue.
During the Treatment
Each session typically lasts about 30 minutes, including the setup and treatment delivery. The actual time the proton beam is delivered to the tumor is only a few minutes. Most patients do not feel any pain or discomfort during the treatment. The proton beam is not felt by the patient, though the machine itself may make some noise. It’s important to remain as still as possible during the treatment to ensure accuracy. Relaxing and staying calm can help reduce movement. Many patients find that closing their eyes and focusing on their breathing can make the process more comfortable.
After the Treatment
After the proton beam is delivered, the treatment session ends, and the patient is carefully assisted off the treatment table. The whole process is non-invasive, and patients typically don’t need any recovery time after the session. Most individuals can go about their normal activities right away, although they may be advised to take it easy depending on how they feel.
Repeat Sessions
Proton therapy often requires multiple sessions, usually spread over several weeks. The frequency and duration of treatment depend on the specific cancer being treated and its location. Each treatment session is carefully planned and adjusted based on the patient’s response.
Patient Tips for a Calm Treatment Experience
- Breathe Deeply: Focused breathing helps relax the body and mind during the treatment. Many patients find that taking slow, deep breaths helps them stay still.
- Listen to Music: Some centers offer music or even allow patients to bring their own playlists to listen to during the procedure, which can help distract and relax.
- Ask Questions: If you’re feeling anxious about the process, don’t hesitate to ask the treatment team to explain anything you don’t understand. Feeling informed can reduce anxiety.
FAQ
How does proton beam therapy differ from other radiation therapies?
Proton beam therapy uses protons instead of X-rays, allowing it to precisely target tumors while minimizing damage to nearby healthy tissue, which is especially useful for tumors near critical structures.
Is proton beam therapy painful?
No, proton beam therapy itself is painless. Patients may feel discomfort from lying still during treatment, but the actual proton beam does not cause pain.
Can proton beam therapy be used after previous radiation treatments?
Yes, proton therapy is often used for reirradiation due to its precision, which helps avoid previously treated tissues and reduce cumulative radiation exposure.
What types of cancers are commonly treated with proton therapy?
Yes, proton therapy is often used for reirradiation due to its precision, which helps avoid previously treated tissues and reduce cumulative radiation exposure.
Are there side effects from proton therapy?
Side effects can include fatigue, nausea, and skin irritation, though these are typically less severe compared to traditional radiation therapy.
How long does each proton therapy session take?
Each session typically lasts about 15 to 30 minutes, though the actual proton delivery may only take a few minutes. Most of the time is spent positioning and preparing.
Is proton therapy covered by insurance?
Coverage varies by insurance provider, but many plans cover proton therapy, especially when traditional radiation poses higher risks. Patients should consult with their provider for details.
What can I do to prepare for proton therapy?
Preparation includes imaging scans, such as CT or MRI, to map the treatment area accurately. Wearing comfortable clothing and discussing any concerns with your care team can also help.
How soon can I resume normal activities after proton therapy?
Most patients can continue normal activities during and after treatment, though some may experience fatigue. Recovery is typically faster than with conventional radiation.
Are there any restrictions during proton therapy treatment?
Patients may need to follow specific dietary or medication guidelines depending on the treatment area. It’s essential to follow any personalized instructions from the care team.
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023
