Anal cancer is a type of cancer that begins in the anus, the opening at the end of the digestive tract. While relatively rare, its incidence has been increasing in recent years, particularly due to infections with the human papillomavirus (HPV).HPV is recognized as a significant risk factor for anal cancer, with most squamous cell anal cancers linked to this virus.
This article provides an overview of anal cancer, including its symptoms, causes, types, diagnosis, and treatment options.
What Are the Symptoms of Anal Cancer?
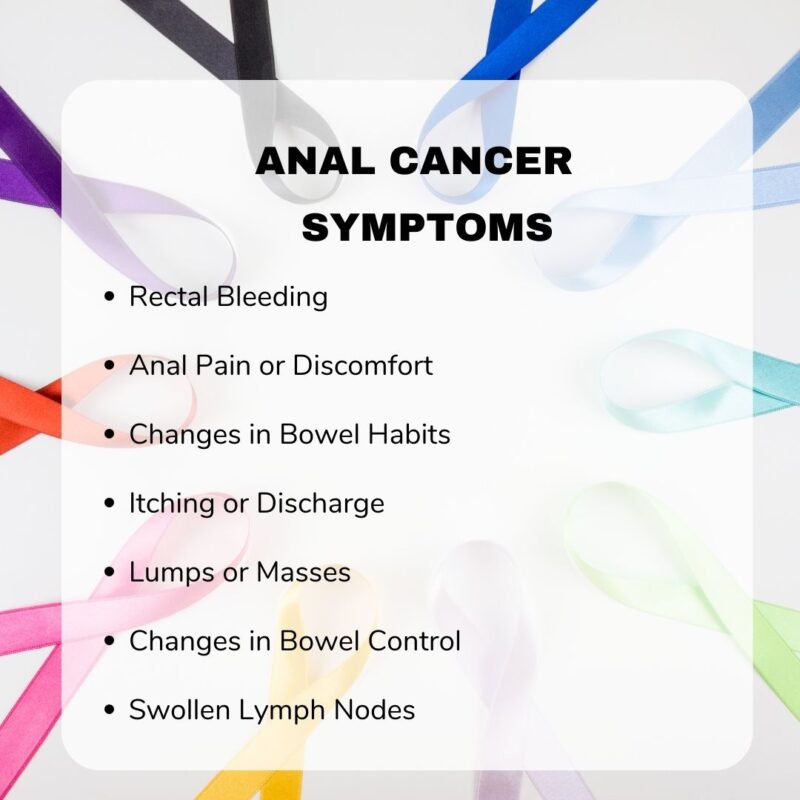
Anal cancer often presents with symptoms such as bleeding, itching, pain, and lumps around the anus. These early signs can closely resemble less serious conditions like hemorrhoids, leading to potential delays in diagnosis. For instance, both anal cancer and hemorrhoids can cause rectal bleeding and the sensation of a lump near the anus. However, while hemorrhoidal bleeding is typically bright red, bleeding from anal cancer may be either dark or bright red. Additionally, anal cancer may present with other symptoms such as diarrhea or constipation, whereas hemorrhoids are often associated with chronic constipation.
This symptom overlap can result in misdiagnosis. A study published in The American Journal of Medicine by Ryan et al. found that over half of anal cancer patients were initially misdiagnosed, with 25% experiencing symptoms for more than six months before receiving an accurate diagnosis. Such delays can adversely affect treatment outcomes, emphasizing the importance of prompt and accurate evaluation of anorectal symptoms.
Healthcare providers should maintain a high index of suspicion when patients present with anorectal symptoms, even those resembling benign conditions like hemorrhoids, to ensure timely and appropriate management.
What are the Causes and Risk Factors for Anal Cancer?
Anal cancer development is influenced by several primary factors, notably human papillomavirus (HPV) infection, smoking, weakened immune systems, and certain lifestyle choices.
- HPV Infection: A significant majority of anal cancer cases are linked to HPV infection. The Centers for Disease Control and Prevention (CDC) reports that approximately 91% of anal cancers are attributed to HPV, with high-risk strains like HPV-16 and HPV-18 being the most prevalent. A comprehensive analysis by de Martel et al. in The Lancet Global Healthfound that HPV DNA was present in 89.4% of anal cancer cases worldwide, underscoring the virus’s pivotal role in the disease’s etiology.
- Smoking: Tobacco use has been identified as a significant risk factor for anal cancer. The American Cancer Society notes that individuals who smoke are several times more likely to develop anal cancer compared to non-smokers. This increased risk is thought to result from smoking-induced immune suppression and direct damage to the DNA of anal canal cells.
- Weakened Immune System: Immunosuppression markedly elevates the risk of anal cancer. People with compromised immune systems, such as those with HIV infection or organ transplant recipients on immunosuppressive therapy, face a higher likelihood of developing anal cancer. For instance, a study by Silverberg et al. in AIDS journal reported that HIV-positive individuals had a significantly increased incidence of anal cancer compared to the general population.
- Lifestyle Factors: Certain sexual behaviors can heighten the risk of anal cancer, primarily due to increased exposure to HPV. Engaging in anal intercourse and having multiple sexual partners are associated with a higher likelihood of HPV transmission. The American Cancer Society highlights that these factors contribute to the elevated risk of anal cancer.
Understanding these risk factors is crucial for developing effective prevention strategies, including HPV vaccination, smoking cessation programs, and regular screenings for high-risk populations.
What Are the Types of Anal Cancer?
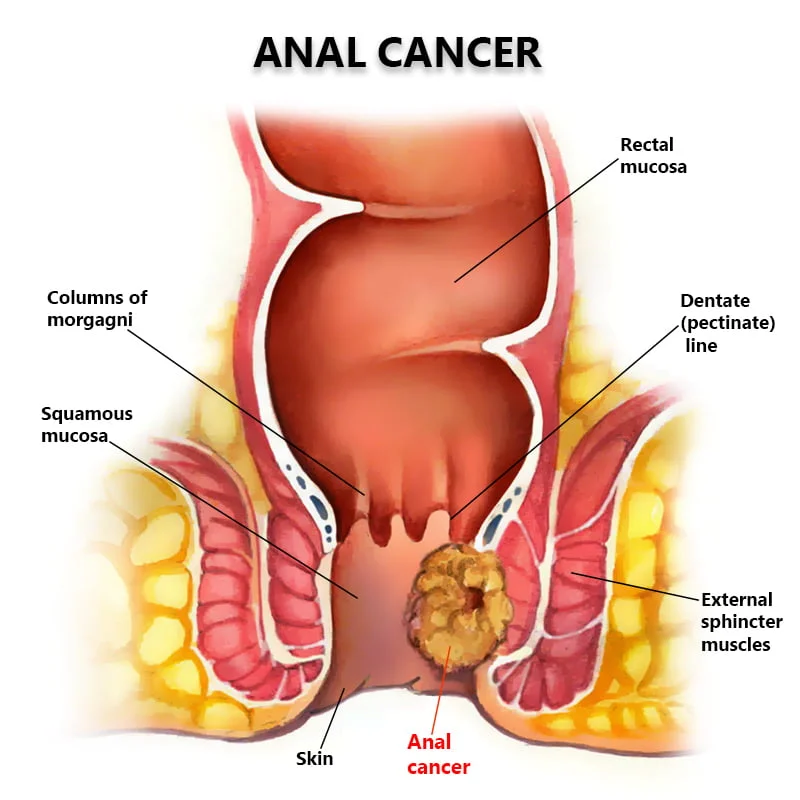
Squamous Cell Carcinoma of the Anus
Squamous cell carcinoma is the most common type of anal cancer, making up about 85-90% of all cases, according to the American Cancer Society. It starts in the thin, flat cells lining the inside of the anal canal. This type is strongly associated with human papillomavirus (HPV) infection, particularly with high-risk strains like HPV-16.
What makes squamous cell carcinoma distinct is its close link to HPV and its location in the squamous cells of the anal lining. Compared to other types like adenocarcinoma or melanoma, squamous cell carcinoma typically responds better to combined treatments of chemotherapy and radiation therapy, especially when detected early. Its prevalence and strong connection to HPV highlight the importance of HPV vaccination and routine screenings, particularly in high-risk groups. Early detection greatly improves treatment success rates.
Adenocarcinoma of the Anus
Adenocarcinoma of the anus is a much rarer form of anal cancer, accounting for only about 5-10% of cases, according to the American Cancer Society. Unlike the more common squamous cell carcinoma, which arises from the flat cells lining the anal canal, adenocarcinoma develops from the glandular cells. These cells are responsible for producing mucus and are located higher up in the anal canal or near the rectum.
One key difference is that adenocarcinoma of the anus behaves more like rectal cancer than typical anal cancer, which means it is often treated with surgery as the primary treatment, followed by radiation or chemotherapy if needed. Because of its rarity, there are fewer large studies on adenocarcinoma, but recognizing its distinct origin and behavior is crucial for determining the appropriate treatment approach.
How Is Anal Cancer Diagnosed?
Diagnosing anal cancer involves a comprehensive approach that includes physical examinations, biopsies, imaging studies, and, in certain cases, genetic testing. These methods collectively aid in the accurate detection and staging of the disease, facilitating the development of effective treatment strategies.
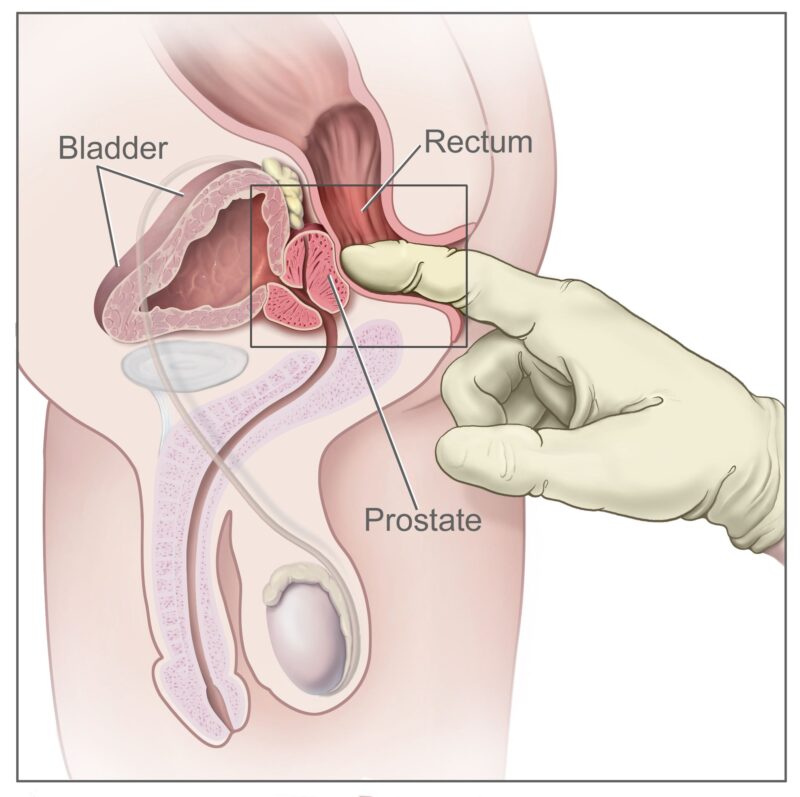
- Physical Examinations: The initial assessment typically begins with a thorough medical history and physical examination. A digital rectal examination (DRE) is commonly performed, wherein a healthcare provider inserts a gloved, lubricated finger into the anus to palpate for any irregularities or masses. This examination can identify abnormalities in the anal canal and rectum.Additionally, for female patients, a gynecologic examination, including cervical cancer screening, is recommended due to the shared risk factors between anal and cervical cancers.
- Biopsy: If a suspicious lesion is detected during the physical examination, a biopsy is conducted to obtain a tissue sample for histopathological analysis. This procedure involves the removal of a small tissue section from the affected area, which is then examined microscopically to confirm the presence of cancer cells and determine the specific cancer type. Accurate histological identification is crucial for guiding appropriate treatment decisions.
- Imaging Techniques: Imaging studies are integral to assessing the extent of the disease and identifying potential metastases. Commonly employed imaging modalities include: CT scans provide detailed cross-sectional images of the body’s internal structures, aiding in the evaluation of tumor size, local invasion, and distant spread, particularly to lymph nodes and organs such as the liver and lungs. MRI utilizes magnetic fields and radio waves to produce high-resolution images, offering superior soft-tissue contrast. This modality is especially useful in assessing the involvement of pelvic structures and determining the tumor’s relationship to adjacent tissues.
- Positron Emission Tomography (PET) Scan: PET scans involve the administration of a radioactive tracer to detect hypermetabolic activity indicative of cancer. This technique is valuable in identifying metastatic disease and evaluating the overall tumor burden.
- Genetic Testing: Genetic testing plays a pivotal role in understanding the molecular characteristics of anal cancer, particularly in cases associated with human papillomavirus (HPV) infection. HPV is implicated in approximately 90% of anal squamous cell carcinomas. Advanced genomic profiling has revealed recurrent alterations in pathways such as phosphoinositol-3-kinase (PI3K/AKT/mTOR), offering insights into potential therapeutic targets.
For individuals with a family history of cancer or those diagnosed with HPV-related cancers, genetic testing can identify specific mutations and biomarkers that inform personalized treatment strategies. For example, the detection of circulating HPV DNA in blood samples has emerged as a non-invasive biomarker for monitoring treatment response and disease progression.
Incorporating genetic markers into the diagnostic process enhances the precision of treatment planning, enabling the selection of targeted therapies and improving patient outcomes. As research advances, the integration of molecular profiling into routine clinical practice holds promise for the development of individualized therapeutic approaches in anal cancer management.
What Are the Treatment Options for Anal Cancer?
Treatment options for anal cancer typically depend on the stage and type of the cancer but generally include three main approaches. According to the American Cancer Society, the primary treatments used are:
- Surgery
- Chemotherapy
- Radiation therapy
These treatments may be used alone or in combination, depending on the individual case. In most cases, chemotherapy and radiation therapy are combined as the first-line treatment, while surgery is usually considered if the cancer does not respond to other treatments.
Surgical Options for Anal Cancer
Surgery plays a crucial role in certain cases of anal cancer, particularly when tumors are caught early or when there is local recurrence after other treatments. For superficially invasive squamous cell carcinoma (SISCCA) and select cases of perianal cancers, a local excision may be sufficient. This procedure involves removing the tumor with a margin of healthy tissue, aiming to preserve the anal sphincter and avoid more extensive surgeries. The guidelines recommend that local excision should only be considered if negative margins can be achieved without compromising sphincter function.
For more advanced or persistent cases, especially when prior treatments like chemoradiation fail, a more extensive surgical option known as abdominoperineal resection (APR) may be necessary. APR involves removing the anus, rectum, and part of the sigmoid colon, requiring the creation of a permanent colostomy. Due to prior radiation, healing can be challenging, so reconstructive tissue flaps are often used to support wound healing. Additionally, if cancer recurs in the groin lymph nodes, especially after previous radiation, an inguinal lymph node dissection might be performed, sometimes combined with APR depending on the spread of the disease.
Chemotherapy for Anal Cancer
Chemotherapy remains a fundamental component of anal cancer treatment, particularly in combination with radiation therapy for localized disease and as systemic therapy for metastatic cases. According to the NCCN Guidelines Version 2.2025, the preferred regimen for localized anal cancer includes 5-fluorouracil (5-FU) /mitomycin alongside radiation therapy. This combination has consistently demonstrated effective disease control. An alternative, equally effective regimen uses capecitabine/mitomycin with radiation, offering similar efficacy with the convenience of oral administration of capecitabine (Goodman et al., 2017).
For patients with metastatic disease, the first-line systemic therapy typically consists of carboplatin and paclitaxel. This combination is favored due to its manageable side effect profile and has shown significant activity in advanced anal cancer, particularly in the InterAAct trial, where carboplatin plus paclitaxel was associated with better tolerability compared to cisplatin-based regimens (Rao et al., 2020).
Additionally, a modified docetaxel, cisplatin, and fluorouracil (DCF) regimen has been recognized as a category 2B recommendation. The EPITOPES-HPV02 trial demonstrated that this regimen offers a promising option for patients with metastatic or unresectable locally recurrent anal squamous cell carcinoma, showing notable tumor response and disease control (Kim et al., 2018, Lancet Oncology). Other chemotherapy regimens include FOLFCIS (cisplatin, leucovorin, 5-FU) and mFOLFOX6 (oxaliplatin, leucovorin, 5-FU), providing additional options tailored to the patient’s tolerance and disease status. Emerging combinations, such as carboplatin, paclitaxel, and retifanlimab-dlwr (an immunotherapy agent), are also being explored, showing promising early results and have been added as category 2B recommendations.
You can read about radiotherapy for Anal Cancer here

What Are the Stages of Anal Cancer?
According to the NCCN Guidelines Version 2.2025 for Anal Carcinoma, anal cancer is staged from Stage I to Stage IV, based on the tumor size, lymph node involvement, and metastasis:
- Stage I: Tumor is ≤2 cm and confined to the anus without lymph node involvement.
- Stage II: Tumor is >2 cm but ≤5 cm, still localized without lymph node spread.
- Stage IIIA/IIIB: Tumor may be >5 cm or involve regional lymph nodes.
- Stage IV: Cancer has spread (metastasized) to distant organs.
Survival rates are better in early stages and decline with advanced disease. The NCCN emphasizes that the majority of patients with localized anal cancer (Stages I–III) achieve excellent disease control with chemoradiation. For instance, local control and colostomy-free survival rates in trials like RTOG 98-11 show favorable outcomes for non-metastatic disease.
How to Live with Anal Cancer?
Coping with an anal cancer diagnosis can feel overwhelming, but focusing on both physical and emotional health is crucial. Managing treatment side effects—such as fatigue, bowel changes, and skin irritation—often involves following your care team’s advice, staying hydrated, and eating a balanced diet. Joining support groups, either in-person or online, can provide comfort and practical advice from others who understand the experience. Mental health support, such as counseling or speaking with a therapist, can help manage anxiety or depression during treatment. Staying active, when possible, and leaning on family, friends, or patient advocacy organizations can greatly improve quality of life after treatment.
Can Anal Cancer Be Prevented?
reventing anal cancer involves addressing key risk factors and following recommended guidelines from cancer research organizations. One of the most effective preventive measures is the HPV vaccination. According to the American Cancer Society, the HPV vaccine is highly effective in preventing infection with the high-risk HPV strains most commonly linked to anal cancer. Vaccination is recommended for all children starting at ages 11 or 12, but can be given up to age 26 for those who missed earlier doses.
Additionally, regular screenings are important, especially for individuals at higher risk, such as those with weakened immune systems or a history of HPV-related diseases. Anal Pap tests and digital rectal exams may help detect precancerous changes early.
Reducing certain lifestyle risk factors also plays a significant role. Quitting smoking lowers the risk of anal and other cancers, while practicing safer sex—such as limiting the number of sexual partners and using protection—reduces the chance of HPV infection. Following these prevention strategies, as advised by the American Cancer Society and similar organizations, significantly lowers the risk of developing anal cancer.
You Can Watch More on OncoDaily Youtube TV
Written by Toma Oganezova, MD
FAQ
What are the common symptoms of anal cancer?
Common symptoms include rectal bleeding, anal itching, pain, a lump near the anus, and changes in bowel habits.
How is anal cancer diagnosed?
Diagnosis typically involves a physical examination, imaging tests, and a biopsy to confirm the presence of cancer cells.
What are the main types of anal cancer?
The primary type is squamous cell carcinoma. Other types include adenocarcinoma, basaloid carcinoma, and cloacogenic carcinoma.
What causes anal cancer?
Anal cancer is often linked to HPV infection, smoking, and having multiple sexual partners.
How is anal cancer treated?
Treatment options include radiation therapy, chemotherapy, and surgery, depending on the cancer's stage and location.
What is the prognosis for anal cancer?
The prognosis varies based on the cancer's stage at diagnosis, but early detection generally leads to better outcomes.
Can anal cancer be prevented?
Preventive measures include HPV vaccination, practicing safe sex, and avoiding smoking.
Is anal cancer common?
Anal cancer is relatively rare, accounting for a small percentage of gastrointestinal cancers.
Who is at higher risk for anal cancer?
Individuals with HPV infection, HIV, a history of cervical or vulvar cancer, and those who engage in receptive anal intercourse are at higher risk.
Are there screening tests for anal cancer?
While there's no standard screening, high-risk individuals may undergo anal Pap tests to detect precancerous changes.