Primary peritoneal cancer (PPC) is a rare and aggressive malignancy that originates in the peritoneum, a thin layer of tissue that lines the inside of the abdomen and covers the abdominal organs. Despite its distinct origin, PPC shares many similarities with epithelial ovarian cancer in terms of its behavior, symptoms, and treatment approaches. This similarity often leads to PPC being treated in much the same way as ovarian cancer.
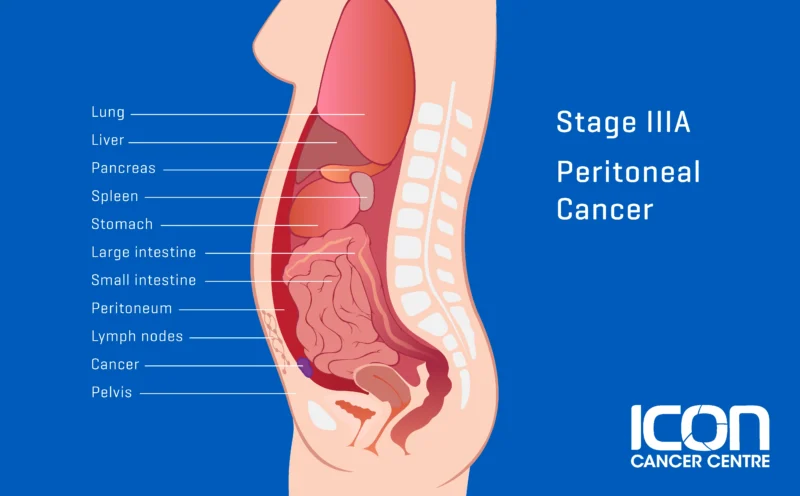
The image is taken from the Icon Cancer Centre website.
Prevalence and Epidemiology
PPC is an uncommon malignancy, accounting for approximately 10% of all cases of peritoneal and ovarian cancers combined. The exact incidence rate is difficult to determine due to the rarity of the disease and the challenges in distinguishing it from ovarian cancer, particularly in advanced stages. However, estimates suggest that PPC affects fewer than 7 in 1 million individuals each year.
PPC predominantly affects women, with a median age at diagnosis of around 60 years. While it can occur in men, such cases are exceedingly rare. The disease is more common among certain ethnic groups, with higher incidence rates reported in white women compared to black women.
Causes and Risk Factors
The exact cause of PPC is not well understood, but several risk factors have been identified:
- Genetic factors: Women with inherited mutations in the BRCA1 or BRCA2 genes (these genes help repair DNA and maintain the stability of genetic information), which are associated with an increased risk of breast and ovarian cancers, also have a higher risk of developing PPC.
- Family history: Having a first-degree relative (mother, sister, or daughter) with ovarian or peritoneal cancer increases the risk of developing PPC.
- Endometriosis: Women with a history of endometriosis, a condition where the endometrial tissue grows outside the uterus, have an increased risk of developing PPC and ovarian cancer.
- Hormone replacement therapy (HRT): The use of HRT, particularly estrogen-only therapy, has been associated with a slightly increased risk of PPC and ovarian cancer.
- Obesity and tall stature: Being overweight or obese, as well as having a tall stature, may increase the risk of developing PPC and ovarian cancer.
Symptoms
Early Stage Symptoms
In the early stages, PPC often presents with vague and non-specific symptoms, which can easily be mistaken for other less serious conditions. These symptoms include:
- Abdominal Discomfort or Pain: Patients may experience mild abdominal discomfort, which can be described as gas, indigestion, pressure, swelling, bloating, or cramps
- Bloating: Persistent bloating or a feeling of fullness in the abdomen is common
- Loss of Appetite: A reduced desire to eat or feeling full quickly after starting a meal
- Nausea and Indigestion: Mild nausea and indigestion are frequent complaints
- Changes in Bowel Habits: This can include increased constipation, diarrhea, or changes in stool consistency
- Frequent Urination: An increased need to urinate, which can be mistaken for urinary tract issues
- Fatigue: General tiredness and lack of energy, which can be subtle and easily overlooked
Late Stage Symptoms
As PPC progresses, the symptoms become more pronounced and severe, often indicating advanced disease. These symptoms include:
- Abdominal Swelling (Ascites): Significant fluid accumulation in the abdomen, leading to noticeable swelling and discomfort
- Severe Abdominal or Pelvic Pain: Intense and persistent pain in the abdomen or pelvis, which can be debilitating
- Unexplained Weight Loss or Gain: Rapid and unexplained changes in weight, often due to fluid retention or loss of appetite
- Nausea and Vomiting: More severe and frequent episodes of nausea and vomiting, often due to the pressure effects of the tumor or ascites
- Shortness of Breath: Difficulty breathing, which can occur if fluid accumulates around the lungs (pleural effusion)
- Bowel or Urinary Obstruction: Complete blockage of the bowel or urinary tract, leading to severe pain, inability to pass stool or urine, and vomiting
- Fatigue and Weakness: Extreme tiredness and weakness, which can significantly impact daily activities and quality of life
- Back Pain: Lower back pain, which can be due to the spread of cancer to nearby structures or pressure from ascites
Diagnosis
Diagnosing PPC can be challenging, as there is no single definitive test for the disease. The diagnostic process typically involves a combination of the following:
- Medical history and physical examination: The healthcare provider will ask about the patient’s symptoms, family history, and risk factors, and perform a physical examination, including a pelvic exam.
- Blood tests: Elevated levels of certain tumor markers, such as CA-125 (cancer antigen 125), can indicate the presence of PPC or ovarian cancer, although these markers are not specific to these conditions.
- Imaging tests: Imaging techniques like computed tomography (CT) scans, magnetic resonance imaging (MRI), and ultrasound can help detect abnormalities in the abdomen and pelvis, such as the presence of tumors or fluid accumulation (ascites).
- Biopsy: A biopsy, which involves removing a small sample of tissue from the suspected tumor or fluid from the abdomen (ascites), is often necessary to confirm the diagnosis and determine the type of cancer.
- Surgical exploration: In some cases, a surgical procedure called a laparoscopy or laparotomy may be performed to visually examine the abdomen and pelvis and obtain tissue samples for biopsy.
It is important to note that distinguishing between PPC and ovarian cancer can be challenging, especially in advanced stages when both the ovaries and peritoneum are involved. In such cases, the treatment approach is often similar for both conditions.
Treatment Options
The treatment of PPC is typically multidisciplinary and may involve a combination of the following approaches:
- Surgery: Cytoreductive surgery, also known as debulking surgery, is often the first line of treatment for PPC. The goal is to remove as much of the visible tumor as possible, including the primary tumor and any metastases. This procedure may involve the removal of the uterus, ovaries, fallopian tubes, omentum (a layer of fatty tissue covering the abdomen), and other affected organs or tissues.
- Hyperthermic intraperitoneal chemotherapy (HIPEC): HIPEC is a specialized treatment that involves delivering heated chemotherapy drugs directly into the abdominal cavity after cytoreductive surgery. The heated chemotherapy solution helps to target and destroy any remaining cancer cells in the peritoneal cavity.
- Systemic chemotherapy: Intravenous chemotherapy, is often administered after surgery to target any remaining cancer cells and reduce the risk of recurrence.
- Targeted therapy: In some cases, targeted therapies with monoclonal antibodies may be used in combination with chemotherapy to target specific molecular pathways involved in cancer growth and progression.
- Radiation therapy: While not commonly used as a primary treatment, radiation therapy may be considered in certain cases, such as for localized recurrences or to alleviate symptoms.
The choice of treatment depends on various factors, including the stage and extent of the disease, the patient’s overall health, and the potential risks and benefits of each approach.
In this video, produced by OncLive, the role of HIPEC for advanced primary peritoneal cancer is explained.
Prognosis of primary peritoneal cancer
The prognosis for PPC is generally poor, even with aggressive treatment. However, recent advancements in treatment strategies, such as cytoreductive surgery combined with HIPEC, have shown promising results in improving survival rates for selected patients.
The prognosis for PPC is influenced by several factors, including the stage at diagnosis, the extent of disease spread, the completeness of surgical resection, and the patient’s overall health and response to treatment. Early detection and prompt treatment are crucial for improving outcomes.
Patient Survivorship
Surviving PPC can be a challenging journey, both physically and emotionally. Patients may experience a range of side effects and complications during and after treatment, which can impact their quality of life. It is essential for patients to have a comprehensive support system and access to resources that can help them navigate this journey.
- Physical side effects: Common side effects of PPC treatment may include fatigue, nausea, vomiting, hair loss, neuropathy (nerve damage), and bowel or bladder dysfunction. These side effects can be managed through medication, dietary modifications, and supportive care.
- Emotional and psychological support: Coping with a cancer diagnosis and undergoing treatment can be emotionally and psychologically taxing. Patients may experience anxiety, depression, and fear of recurrence. Access to counseling, support groups, and mental health resources can be invaluable in managing these challenges.
- Fertility preservation: PPC and its treatments can impact fertility in women of reproductive age. Discussing fertility preservation options, such as egg or embryo freezing, with a reproductive specialist before starting treatment is recommended for those who wish to have children in the future.
- Survivorship care plan: Upon completing treatment, patients should work with their healthcare team to develop a comprehensive survivorship care plan. This plan should outline follow-up care, surveillance for recurrence, management of long-term side effects, and strategies for maintaining a healthy lifestyle.
- Palliative care: For patients with advanced or recurrent PPC, palliative care services can provide comprehensive support to manage symptoms, alleviate pain, and improve overall quality of life.
Problems During and After Treatment and How to Manage Them
Patients undergoing treatment for PPC may encounter various challenges and side effects that can impact their daily lives. It is essential to be aware of these potential problems and to work closely with the healthcare team to manage them effectively.
- Gastrointestinal issues: Chemotherapy and radiation therapy can cause gastrointestinal side effects such as nausea, vomiting, diarrhea, constipation, and loss of appetite. Medications, dietary modifications, and hydration management can help alleviate these symptoms.
- Fatigue and weakness: Cancer treatment can lead to significant fatigue and weakness, making it difficult to perform daily activities. Strategies such as pacing activities, getting adequate rest, and engaging in light exercise (as tolerated) can help manage fatigue.
- Pain management: Abdominal pain and discomfort are common in PPC patients, particularly after surgery or during treatment. Effective pain management strategies, including medication and complementary therapies like acupuncture or massage, can help improve quality of life.
- Lymphedema: Lymphedema, or swelling in the legs or arms due to fluid buildup, can occur after surgery or radiation therapy. Early recognition and management, including compression garments and physical therapy, can help reduce the risk and severity of lymphedema.
- Nutritional support: Cancer and its treatments can affect appetite and nutrient absorption, leading to malnutrition and weight loss. Working with a registered dietitian can help ensure adequate nutritional intake and manage any dietary restrictions or side effects.
- Emotional and psychological support: As mentioned earlier, access to counseling, support groups, and mental health resources is crucial for managing the emotional and psychological challenges associated with PPC diagnosis and treatment.
- Palliative care: For patients with advanced or recurrent PPC, palliative care services can provide comprehensive support to manage symptoms, alleviate pain, and improve overall quality of life.
Patients need to communicate openly with their healthcare team about any side effects or challenges they are experiencing. Early intervention and appropriate management strategies can help minimize the impact of these problems and improve overall well-being.
Future Perspectives
Targeted Therapies
- Folate Receptor Alpha (FRα) Targeting: Mirvetuximab Soravtansine is an antibody-drug conjugate that targets FRα, which is overexpressed in many PPC cases. Clinical trials have shown promising results in improving progression-free survival and overall survival in patients with FRα-positive PPC.
- PARP Inhibitors: Drugs like olaparib, niraparib, and rucaparib are effective, especially in patients with BRCA mutations.
- Angiogenesis Inhibitors: Bevacizumab is used to inhibit the growth of new blood vessels that tumors need to grow.
Immunotherapy
- Checkpoint Inhibitors: Drugs like pembrolizumab and nivolumab are being tested in combination with other treatments to enhance efficacy.
- Adoptive Cell Therapy: CAR-T cells and tumor-infiltrating lymphocytes (TILs) are being explored for their potential to target and destroy cancer cells more effectively.
Personalized Medicine
- Genomic Profiling: Molecular profiling advances allow personalized treatment plans based on specific mutations and biomarkers.
- Biomarker-Driven Trials: Clinical trials are increasingly focusing on biomarker-driven approaches to improve outcomes and reduce side effects.
Combination Therapies
- Sequential and Concurrent Therapies: Combining different treatment modalities, such as surgery, chemotherapy, targeted therapy, and immunotherapy, is being explored to enhance overall treatment efficacy.
More information about completed and ongoing clinical trials for PPC can be found here – clinicaltrials.gov.
Conclusion
In conclusion, primary peritoneal cancer is a rare and aggressive form of cancer that requires a multidisciplinary approach to treatment and comprehensive support for patients. While the prognosis remains challenging, advancements in treatment strategies and a better understanding of the disease have improved outcomes for selected patients. By staying informed, seeking prompt medical attention for any concerning symptoms, and working closely with their healthcare team, patients can navigate this journey with greater confidence and support.
Sources
- Ovarian, Fallopian Tube, and Primary Peritoneal Cancer – National Cancer Institute
- Treatments for primary peritoneal carcinoma – Canadian Cancer Society
- Primary peritoneal cancer – Cancer Research UK
- Primary peritoneal cancer – Foundation for Women’s Cancer
- Primary Peritoneal Carcinoma: A Rare Malignancy Presenting a Diagnostic Challenge – Cureus
- FDA Approves Mirvetuximab Soravtansine-gynx for FRα-Positive, Platinum-Resistant Epithelial Ovarian, Fallopian Tube, or Primary Peritoneal Cancer – The ASCO Post