Gustavo Viani, Associate Professor in the Department of Medical Imaging, Hematology, and Oncology at Hospital das Clínicas, Faculty of Medicine of Ribeirão Preto, University of São Paulo (FMRP-USP), shared a post on X:
“Hey – those treating melanoma brain metastases!
We know the challenge.
Melanoma brain metastases require precision and collaboration. SRS, immunotherapy, and new guidelines are revolutionizing outcomes.
This thread breaks it all down:
• SRS dosing strategies
• Timing for SRS + ICIs
• Why WBRT is now palliative
Let’s elevate care together
Introduction
• Melanoma is one of the most aggressive cancers, with brain mets affecting 50% of stage IV patients
• Advances in systemic therapy, like checkpoint inhibitors (anti-CTLA4 & anti-PD1) and BRAF/MEK inhibitors, have extended survival:
• Asymptomatic patients: Median survival >5 y
• Symptomatic patients: Median survival ~9 mo
Whole Brain Radiotherapy (WBRT)
•WBRT has been the cornerstone for multiple brain metastases but has significant drawbacks:
•Median survival: 3-4 mo
•Neurocognitive decreased in ~90% of survivors >6 mo
Standard WBRT doses:
•30 Gy/10 fr (3 Gy/fr)
•35 Gy/14 fr (2.5 Gy/fr)
Current Role: WBRT is now palliative for select patients or when SRS/systemic therapy isn’t an option
SRS Alone
SRS has emerged as the first treatment modality for patients with limited brain metastases (1-10 lesions) due to its precision and low neurotoxicity
Guidelines:
EORTC:
•SRS is recommended for up to 5 brain metastases, with individual consideration for larger numbers based on size and location
EANO-ESMO:
•SRS for 1-4 metastases ≤4 cm, or 5-10 metastases ≤3 cm with a cumulative volume ≤15 mL
NCCN/ASCO:
•SRS for up to 10 metastases, prioritizing lesion volume over the absolute number of metastases
Study Outcomes:
Thompson et al. (2022):
• SRS provides a 1-y local control rate of 76% (vs. 9% with WBRT) and a median survival of 7.5 mo (vs. 3.5 mo with WBRT).
Liew et al. (2010):
• SRS achieved 73% local tumor control in melanoma brain metastases, with prolonged survival for patients with ≤8 metastases
SRS Dose:
• For small, well-defined lesions: 20-24 Gy/ 1 fr
• For larger lesions or those near critical structures: 27-30 Gy/3 fr
SRS vs. Surgery
•SRS is increasingly favored over surgery for local tumor control due to its non-invasive nature and equivalent outcomes for most patients
Surgery is reserved for:
•Large symptomatic lesions
•Solitary mets in surgically accessible areas
•Cases requiring tissue for histological drugs
Guidelines:
•EORTC: Surgery is a Second-line option when SRS is not feasible
•ASCO-SNO-ASTRO: Recommends SRS to the surgical cavity to increase local control after resection
Study Outcomes:
Hong et al. (2019):
•Compared WBRT vs. observation after surgery/SRS for 1-3 metastases. WBRT showed No survival benefit (16.5 vs. 13 mo)
•Emphasizes the value of local control with SRS alone
SRS Dose for Surgical Cavities:
•15-18 Gy/1 fr depending on cavity size and proximity to critical structures
•Alternatively, 25-30 Gy /5 fr – larger cavities
Combining SRS with Immunotherapy
•Combining SRS with immune checkpoint inhibitors (ICIs) has become a game-changer, leveraging the synergy of local and systemic treatments
Guidelines:
•EORTC, EANO-ESMO, NCCN:
•Recommend concurrent use of ipilimumab + nivolumab (COMBO) w/ SRS for asymptomatic brain metastases, regardless of BRAF status
•Timing matters: Concurrent therapy (within 4 weeks) high outcomes over sequential approaches
Study Outcomes:
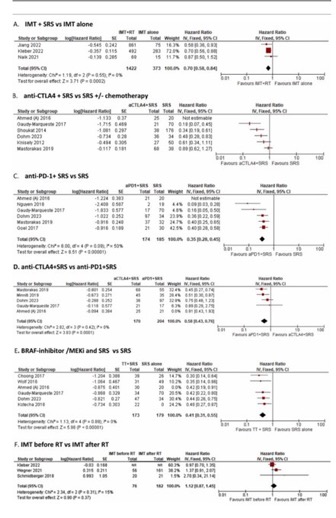
Meta-analysis (Williams et al. 2024):
•Patients receiving SRS + ICIs had a 30% decreased risk of death compared to ICIs alone
• 65 % decreased for patients treated with SRS+anti-PD1 and by 59 % with SRS+anti-CTLA4 and/or anti-PD1 (HR 0.41, 95 %CI 0.31–0.54) to SRS alone
Matsunaga et al. (2018):
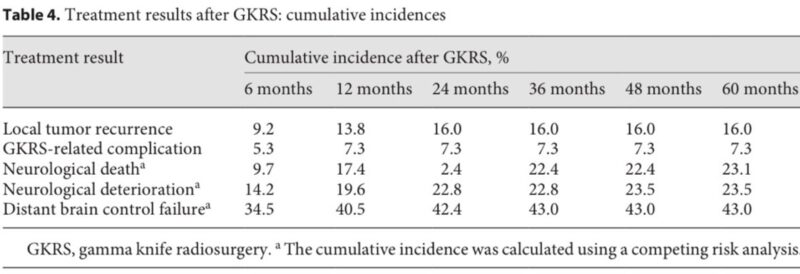
•SRS achieved 86.2% local tumor control at 12 mo, demonstrating efficacy when combined with systemic therapy
SRS Dose in Combination with ICIs:
•Standard SRS doses (e.g., 20-24 Gy/1 fr) remain effective and safe
•Careful coordination ensures no delay in initiating immunotherapy
Number of Metastases: SRS vs. WBRT
•SRS is preferred over WBRT even for patients with multiple metastases, depending on cumulative tumor volume
Study Outcomes:
Liew et al. (2010):
•Prolonged survival in patients with ≤8 metastases treated with SRS
Matsunaga et al. (2018):
•SRS provided effective control for patients with multiple brain metastases, with outcomes influenced by tumor volume rather than number of lesions
SRS Dose for Multiple Metastases:
•Treat smaller metastases with 20-24 Gy/1 fr
•Consider hypo schedules (e.g., 27 Gy/3 fr) for larger or critically located lesions
Future Directions
Optimizing SRS protocols for patients with larger/multiple lesions:
•Hypo schedules like 27 Gy/3 fr show promise for larger tumors
Defining the ideal timing of systemic therapy w/ SRS:
•Current evidence favors starting ICIs within 4 weeks of radiation for optimal synergy
•Further evaluation of hippocampal-sparing WBRT to mitigate cognitive decrease in palliative cases
Conclusion
The treatment paradigm for melanoma brain metastases has shifted:
•SRS + immunotherapy is the new standard for asymptomatic cases
•WBRT is reserved for select palliative case
•Ongoing clinical trials will refine strategies for increased OS and QuoL
Precision and synergy define the future of melanoma care.”
Gustavo Viani, MD is an Associate Professor in the Department of Medical Imaging, Hematology, and Oncology at Hospital das Clínicas, Faculty of Medicine of Ribeirão Preto, University of São Paulo (FMRP-USP). Dr. Viani’s research focuses on radiation oncology, with expertise in brachytherapy, stereotactic radiosurgery, dose fractionation, radiation tolerance, and overall oncology practices.


