So yet again we find ourselves in the middle of a COVID-19 wave. Again. If this summer follows the previous three, we should expect ~10-15% of Americans and maybe slightly fewer Europeans to get infected:

False negatives at the beginning of infection are very common, thanks to the virus mutating. In a recent study, antigen and PCR tests only agreed 47-58% of the time. If they did agree, there was a 1-8 day delay between a PCR turning positive and an antigen test turning positive:

https://journals.asm.org/doi/10.1128/spectrum.01295-23
The higher we are in a wave, the more sceptical you should be of a negative result. There are two things you can do to help reduce scepticism (i.e., false negatives):
- Swab throat and saliva. These are positive days before the nose.
- Repeat testing. Two tests within 48 hours catch 92% of symptomatic cases and 39% of asymptomatic cases. Three tests 48 hours apart detected 94% of symptomatic and 57% of asymptomatic patients.
If you get a positive…Positives are positives. You’re infectious.
The faintness of a line provides clues, though:
- Very bold line = you’re very contagious.
- Barely see the line = you’re at the beginning or the end of your infection window.
I wouldn’t bother. Wastewater is where it’s at these days, and, fortunately, that doesn’t require you to do anything different.
Isolate for five days, at minimum.
- When is Day 0? The first day of symptoms (not the day you get a positive test).
- When do we leave isolation? Technically the CDC says Day 5. But 2 out of 3 people will still be infectious. It’s best to stay in isolation until you have a negative antigen test.
- Where was I infected? Wherever you were ~48 hours before symptoms started.
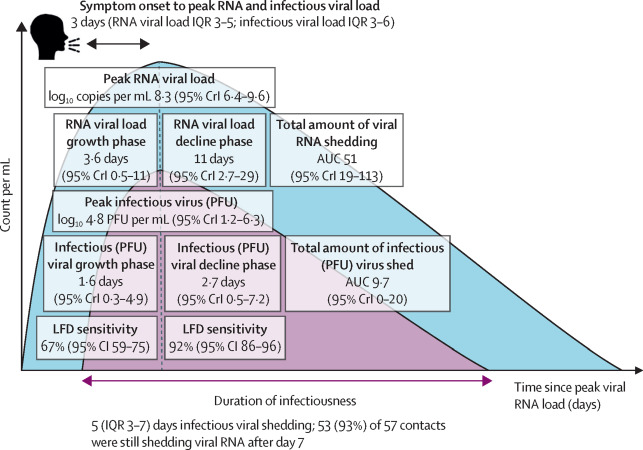
https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(22)00226-0/fulltext
A recent study found only 1 in 4 nursing home residents with COVID-19 were prescribed an antiviral. This isn’t very many:
https://jamanetwork.com/journals/jama/article-abstract/2807529
How long will I have symptoms? ~6-12 days. Maybe longer, maybe shorter. It depends on a lot of individual factors. But having symptoms doesn’t necessarily mean you’re infectious. A great way to know is to test to exit (if negative, you’re clear).
Pink eye with kids? According to the American Academy of Ophthalmology, the newer subvariants of COVID-19 are responsible for some cases of pink eye. In a small study in China, 25% of children aged 2-11 had pink eye during COVID-19 infection. Among adults, it’s much lower rates (1-2% of cases have pink eye).
Should I wear a mask?
- In your house: Masks work. A recent study found that if the index case (i.e., infected person) was masked at home, household transmission was reduced by 67%. Not sharing a bedroom reduced risk by 78%.
- Going outside. You don’t need to wear a mask to walk your dog.
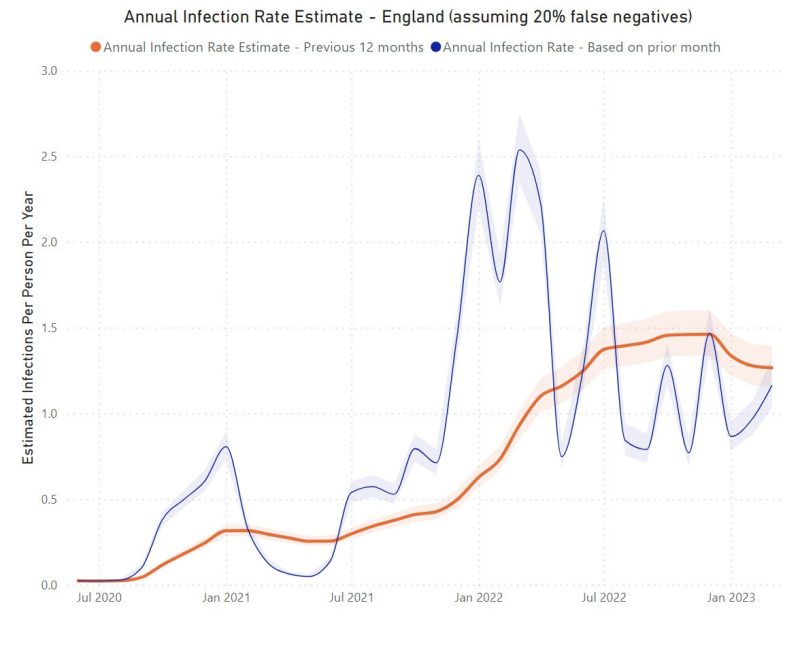
Does this mean I’m in the clear for winter? Maybe. Data from the UK shows that, on average, people get 1-2 infections yearly. You’ll have good protection going into the fall respiratory season. (I would delay a fall booster by at least six months; more on this later).
I’ve never had an infection. Do I have superpowers? Maybe. Or, perhaps, an infection went undetected. Scientists recently discovered that if you have two copies of a specific gene (HLA-B*15:01), you are 8x more likely to remain asymptomatic. Unfortunately, there’s no way for the average person to know. So, harm reduction is still the name of the game:
https://www.nature.com/articles/s41576-023-00641-6
Thanks to our immunity wall, 2023 looks very different, but we can still use tools to help minimize disruption.
Anonymous author


