Sebastian Schmidt, Head of Strategy and Medical Affairs Computed Tomography at Siemens Healthineers, shared on LinkedIn:
“Lung cancer screening and radiation protection.
One concern in the early times of lung cancer screening was radiation exposure from the CT examinations. Now a recent study again looks at the topic:
Like previous studies, they calculate the ratio between benefit (lives saved) to radiation-induced harm (radiation-induced cancers/deaths). Using data from various studies, the result is between 9:1 and 63:1.
Assumptions were worst case, which is fair in this case. Some reasons:
– Data is from NLST, NELSON and Co, which started more than 20 years ago and reflects technology from that time.
– Underestimation of benefits: As I previously explained, the used studies only gave the lower threshold of mortality benefit – real benefit would give higher ratios.
– They use radiation mortality from non-screened populations (Hiroshima). As we know from the International Early Lung Cancer Action Program (I-ELCAP), lung cancer mortality is very low in screening, so mortality from radiation-induced lung cancer within a screened population is lower.
Overall: The radiation exposure from screening is well-justified and no reason against screening. Even under worst-case assumptions.
Still, we want of course as little radiation induced cancers as possible – what can we do?
Consider cumulated radiation dose – 90mGy fitting to US recommendations are too high (3mGy CTDI, annual, 50-80). Simply setting lower dose thresholds would not do the trick, impacting image quality. So concrete recipes are required to ensure good enough image quality at reasonable dose.
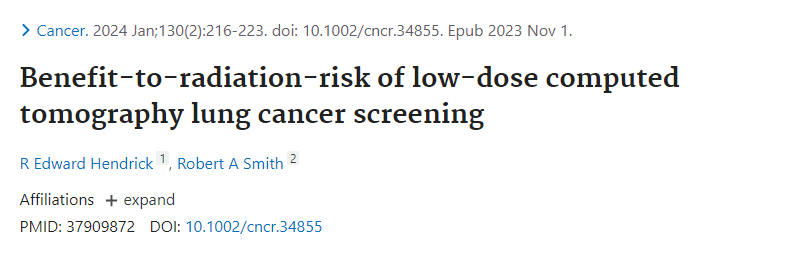
The best analysis that I know came from the German Federal Office For Radiation Protection (BfS), which provided a profound report on the topic. As far as I know, it’s only available in German, short summary of few key points:
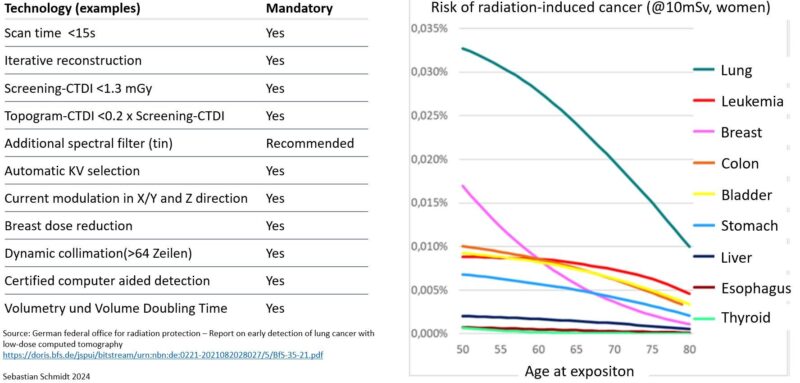
– Gender-specific risk: Screened women have higher risk, due to breast dose (right side of the chart, purple). As a consequence, BfS recommends angular dose modulation (lower tube current in anterior (ap) projections, higher in pa), which significantly reduces breast dose. This is extremely important as women profit strongly from screening, and the number of women at risk is growing (see CASCADE, REVEL Marie-pierre)
– Organs at risk are in upper abdomen: Colon, stomach. Dynamic collimation should be used in scanners >64 slices to limit the dose to adjacent body regions.
– We don’t need much low-energy photons, so selective filtering (tin, silver) is very helpful to eliminate these before the patient.
– Automatisms help to reduce user errors – KV, tube current modulation etc, should be set automatically, according to patient anatomy.
– AI may help to improve detection of smaller nodules, even at low-dose images
As a summary: The new study confirms that radiation-risk is absolutely acceptable in lung cancer screening. Still we owe it to the participants to keep the dose as low as reasonable, this applies to caregivers and regulators.”
View the article.
Source: Sebastian Schmidt/LinkedIn