Shravan Nadkarni: Post-hepatectomy Liver failure (PHLF) – Lets dive right in!
Shravan Nadkarni, Consultant Surgical Oncologist at Karnataka Cancer Therapy and Research Institute Hubli-Dharwad, made the following post on Twitter:
“Post-hepatectomy Liver failure (PHLF) – Dreaded complication of a difficult surgery
Is there a unifying definition of PHLF?
What are the preventive strategies?
How best can it be managed?
Lets dive right in!
Leading cause of post-hepatectomy mortality
Rx Challenges?
Heterogeneity- Lack of uniform diagnostic Cx despite ISGLS Defn(2001)- variations prevalent
Predictability- Accurate preop predictions difficult
Therapy- No effective Rx once PHLF occurs
Prevention:
Applies to patients with Ⓝ and abⓃ preop liver func (provided other causes ruled out Eg. biliary Obs)
In preop INR/Bili- PHLF def INCREASING Sr Bil/INR on/after POD5 / need of FFP, clotting factors to maintain INR
Y POD5? (Reissfelder 2011)- median levels return to Ⓝ by
Severity –
Grade A – Non-clinically relevant postop deterioration of LFT – no deviation from expected course, no need of additional evaluation, managed in ward
Grade B – deviation frm usual postop course; managed without invasive Rx (FFP, albumin, NIV) transfer to intermediate care/ICU; Might need imaging & goal directed Rx
Grade C – Critical condition; Need Invasive Rx (drainage, hemodialysis, intubation, pressors)
Periop Mortality (Reissfelder 2011) – PHLF Gr A, B, C : 0%, 12%, 54%
“50-50” Criteria (Balzan et al, 2005) – combination of prothrombin time index <50% & Sr bilirubin >50 mmol/L (2.9 mg/dL) on POD 5
Sensitivity & Specificity in predicting PHLF – 50% & 97%
Peak Sr Bilirubin > 7 mg/dL – Sen/Spe : 93% & 94%)
ISGLS PHLF def does not provide general cut-off levels nor uses strict preop values to define INR & Bil
Levels are in reference to Ⓝ range acc to local labs & helps eliminate confounding fac & holds true regardless of d extent of resection/underlying disease status
Other scores – CTP- preop use to predict postop Px established. But, postop use confounded by bil obst, use of FFP/alb, bile leak MELD- designed for risk assessment for cirrhotics scheduled for TIPSS & to prioritize for LTx- but as a postop measure of func is controversial
Pitfalls of ISGLS Defn-
Clinical relevance of Gr A?
No distinction b/w 1° & 2° liver failure
Time point of applicability – POD 5 limited possibilities left to substantially influence & potentially Rx postop liver dysfunc since regeneration starts almost immediately
Therefore there seems to be an urgent need to develop predictive models for the 1st 48 postop hrs – guiding better Rx decisions to prevent PHLF than Rx it since Rx options are limited & most measures are at best ‘supportive’
Preop models to predict/stratify risk for PHLF ?
Combination of aspartate aminotransferase/platelet ratio index (APRI) & albumin–bilirubin grade (ALBI) score – Good preop risk assessment of postop outcomes
French Risk calculator for PHLF in cirrhotics
Need validation
Risk factors for PHLF – click here to view details.
FLR & PHLF – Functional liver remnant estimated by preop CT 3D recon correlates well with postop liver weight
Expressed as a % of liver minus d tumour –
Cut-off –
Healthy Liver – 20-30% FLR (0-6% PHLF)
Pre-existing liver disease (cirrhotics/cholestasis)- 40%
FLR is quantitative; presumes remnant liver to b optimally functional
ChemoRx effects/Liver dis – not accounted for
∴ Func assessment (quality) + FLR (quantity)
Post-PVE augmentation of FLR function is heterogenous
∴ total liver function & its distribution in FLR
Augmentation of FLR –
Portal V Embolization (PVE) -> compensatory growth of the FLR
ALPPS – accelerated 2-stage Sx combining PV occlusion + parenchymal transection induces rapid growth of FLR
PVE + HVE – of the specimen to be resected FLR hypertrophy
Management –
Goal – support organ function for spontaneous recovery
Symptom Mx – all aspects of modern intensive organ & patient support
Medical – Supportive measures
Surgical – Liver Tx
ECLS – details here.
Medical –
Antibiotics – prophylactic Abx – No benefit; if PHLF develops, aggressive Abx Rx infectious complications
Source control – imaging drainage of septic foci, ERAS, early drain removal, culture-directed Abx Rx
Lactulose – for hep enceph
Surgical – LTx The only definitive Rx in PHLF
Issues – Optimal time point of Tx? Justified in light of donor organ shortages?
∴ Rescue Rx, tertiary centres, for benign pathology
ECLS – bridging impaired function
Molecular adsorbent circulating system (MARS) – improved detoxification in acute/acute-on-chr liver failure – No survival benefit in RCT
Modified fractionated plasma separation & adsorption (Prometheus)
Single-pass albumin dialysis
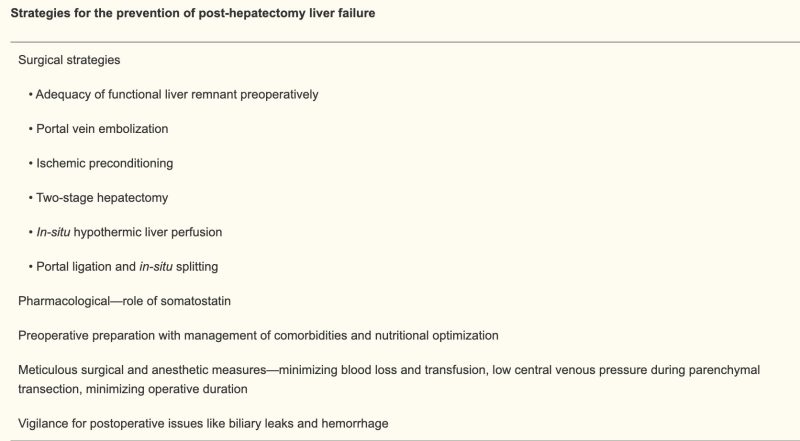
Prevention strategies for PHLF:”
Source: Shravan Nadkarni/Twitter