PROSCA 2024, the final part of the RENALC-BLADDR-PROSCA 2024 forum, took place on November 29 (full day) and November 30 (AM), 2024.
For 2024, the focus remained on translating new data into clinical practice. The program featured state-of-the-art lectures, case discussions, and panel debates. The faculty consisted of carefully selected international and multidisciplinary experts who discussed the key topics of 2024 in renal, prostate, and bladder cancer. To maximize interaction, no parallel sessions were held.
The journey took participants to Vienna and beyond. Prior to the meetings, case challenges were sent out, allowing attendees to compare their opinions with peers and experts. These cases were incorporated into the RENALC-BLADDR-PROSCA program during the meetings (26 November for RENALC, 27 & 28 November for BLADDR, and 29 & 30 November for PROSCA).
María Natalia Gandur Quiroga is a Medical Oncologist and Chief of the Division of Genitourinary Medical Oncology at the Ángel H. Roffo Oncology Institute in Buenos Aires, Argentina. She is a Professor of Medicine at the University of Buenos Aires at the Oncologists Post Graduates Studies.
Her research focuses on clinical trials with aims to improve the treatment of patients with urologic tumors. She is an active member of the European Association for Cancer Research, Argentinian Medical Association and American Society of Clinical Oncology.
María Natalia Gandur Quiroga shared her insights from PROSCA 2024:
Regional Lymph Node Staging by PSMA-PET:
“Regional Lymph Node Staging by PSMA-PET: How to Optimize Interpretation?
Presented by: Ken Herrmann
Moderators: Verane Achard, Johan Stranne
Panel: Bertrand Tombal, Thomas Zilli, and team
Key Insights
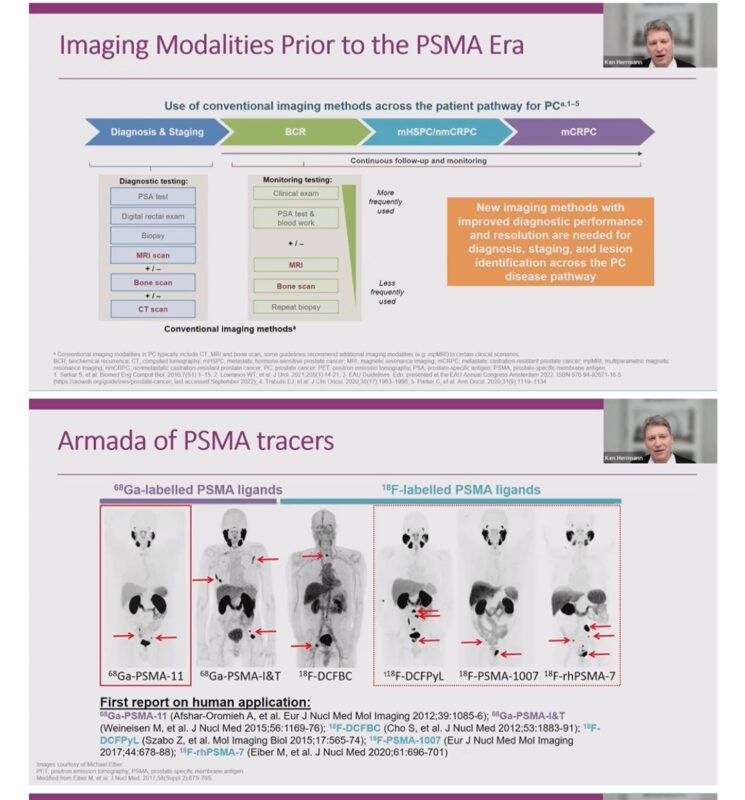
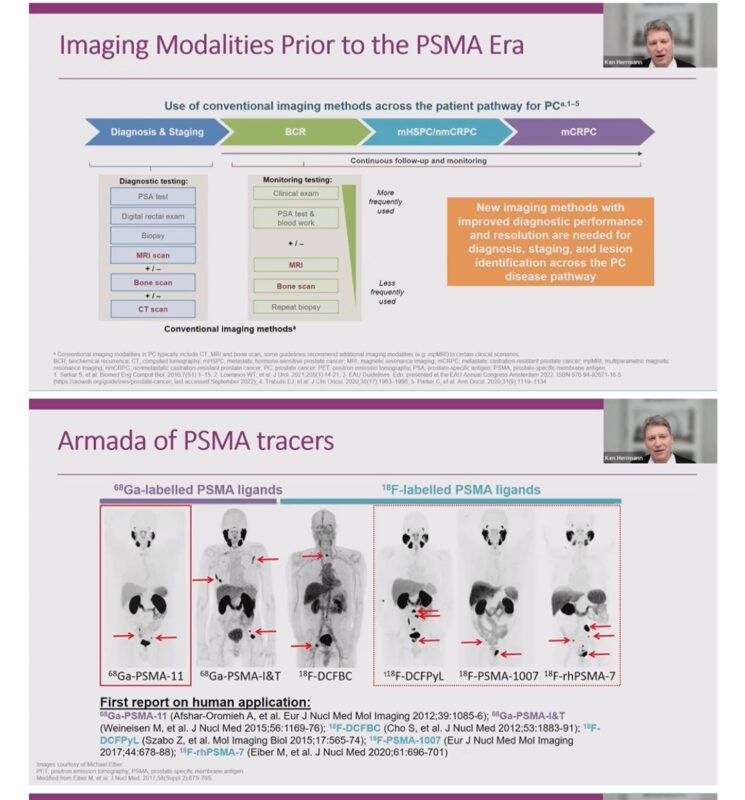
Pre-PSMA Era: Imaging relied on CT, MRI, bone scans; limited precision.
PSMA Tracers: 68Ga-PSMA-11 & 18F-DCFPyL dominate, with FDA/EMA approvals.
Guidelines 2024: Strong recommendation for PSMA-PET in high-risk & locally advanced prostate cancer cases.
PROMISE Standard: Unified reporting ensures better lesion localization & staging.
Clinical Impact: PSMA-PET outperforms conventional imaging in nodal staging with superior specificity (>95%).
Data Spotlight
– ProPSMA: Accuracy 92% (PSMA) vs 65% (conventional).
– Sensitivity challenges (40%), but unmatched clarity for treatment decisions!
Take-Home: No PSMA uptake ≠ no nodal metastases. Interpretation needs expertise.
Access full resources.”
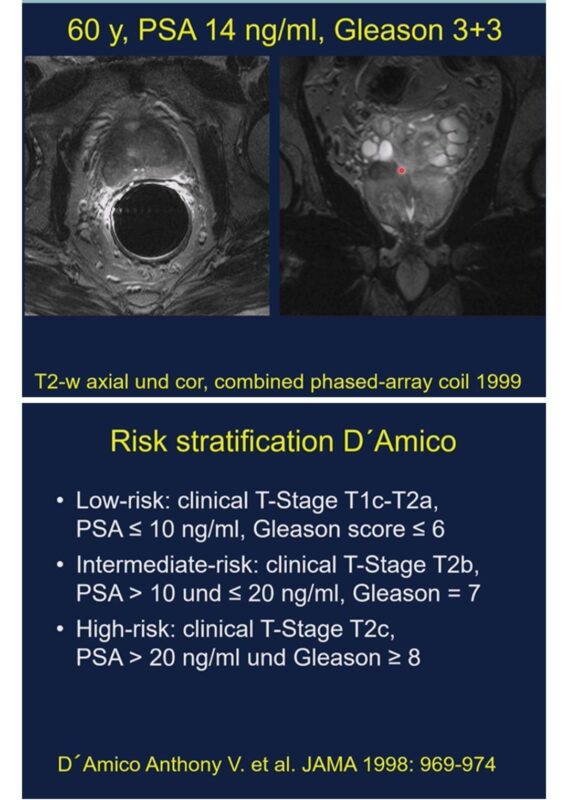
Active Surveillance for Low-Risk PCa: A Modern Approach at PROSCA24:
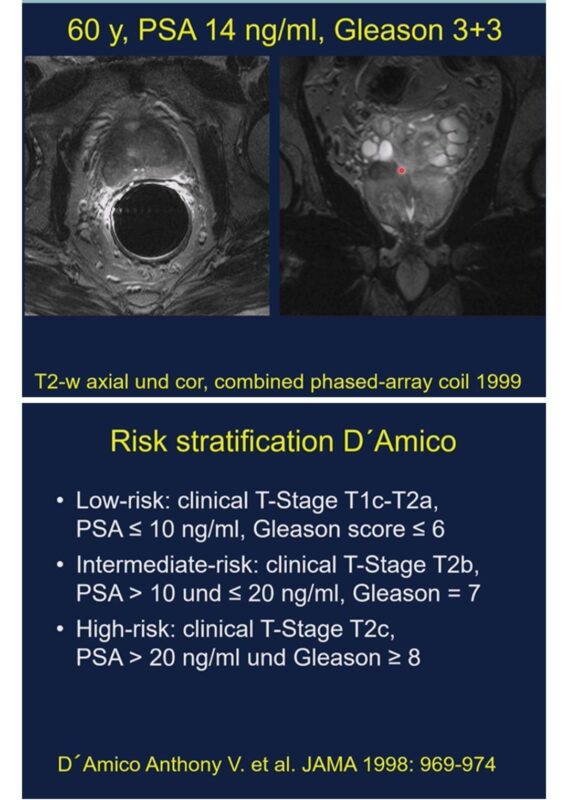
“Active Surveillance for Low-Risk PCa: A Modern Approach at PROSCA24
Presenter: Dirk Beyersdorff
Key Takeaways:
– MRI fusion biopsies outperform systematic biopsies for precision in detection.
– German S3 Guideline 2024: Active surveillance for ISUP 1 PCa is strongly recommended!
– Gleason 6 cancers: Minimal metastatic risk, excellent long-term outcomes.
– Life expectancy matters – customized care is crucial.
– PI-RADS V2: A reliable tool to predict clinically significant prostate cancer.
– Clinical Pearl: Surveillance isn’t passive—it’s an active, personalized journey ensuring optimal outcomes!
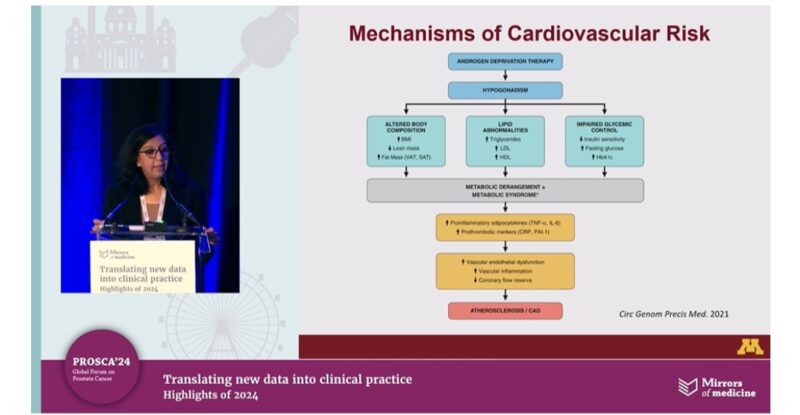
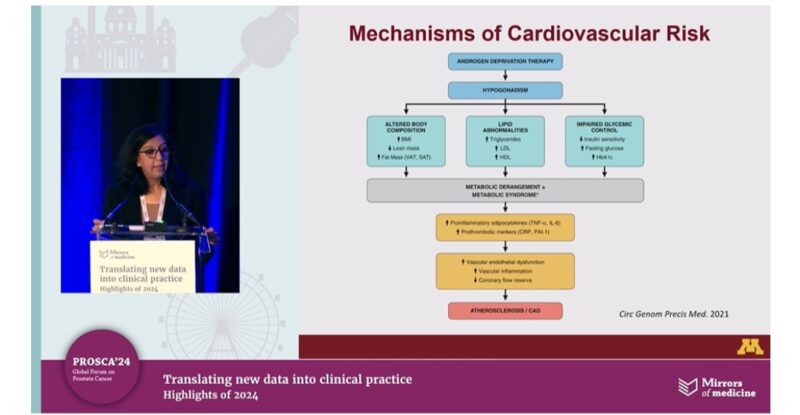
Cardiovascular complications related to hormonal therapy:
“Update lecture: Cardiovascular complications related to hormonal therapy: identification, assessment, and management
Moderator: Athanasios Papatsoris | Presenter: Suma Konety
– PCa & CVD intersection: Shared risk factors and ADT’s cardiovascular implications.
– ADT’s impact: Essential for prostate cancer, but increases CV risk via metabolic syndrome & QT prolongation.
Key interventions:
– Regular CVD risk assessment (duration, therapy type).
– Continuous monitoring of BP, lipids, BMI, HbA1c every 3 months with ≥2 risk factors.
– Multi-disciplinary management: cardio-oncology, endocrinology, mental health.
Conclusions: Implementing CV risk management can improve overall survival.
Future outlook: Research safer ADT alternatives and optimized monitoring strategies.
Clinical takeaways to minimize CV risks and optimize PCa outcomes!
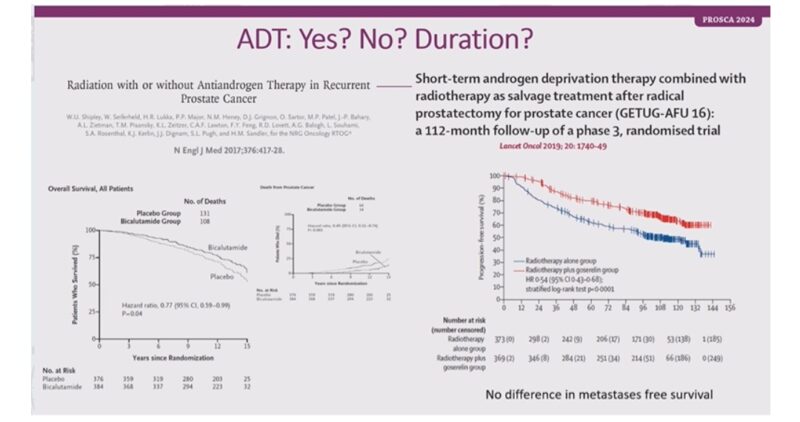
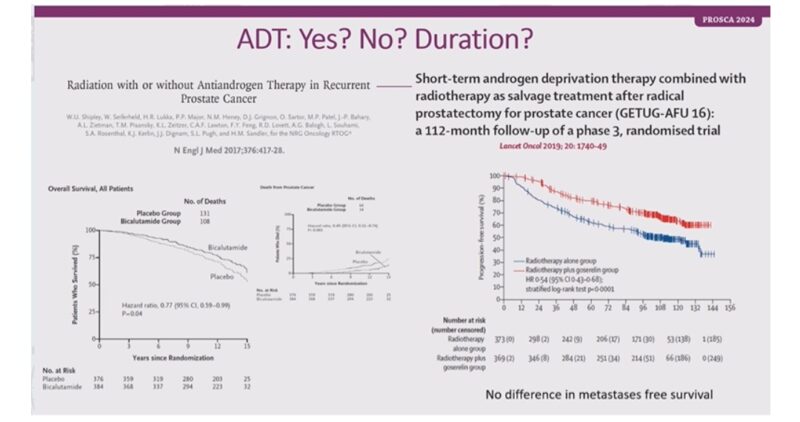
Tailoring salvage therapies for BCR post-RP:
“Second chances: tailoring salvage therapies for BCR post-RP
Presenter: Peter Hoskin
Key Takeaways:
– Early salvage RT improves outcomes; PSA <0.2 μg/L is critical for timing.
– Adjuvant vs. early salvage RT? Meta-analysis shows non-significant survival differences but personalized approaches matter.
– Dose-intensified salvage RT offers no clear survival benefit over conventional doses.
– Short-term ADT with salvage RT enhances survival; duration optimization remains debated.
– PSMA PET/CT identifies treatment targets—crucial for staging before RT.
Future considerations:
– Stage all patients with PSMA PET?
– Can ADT duration be reduced to 4–6 months?
– Salvage therapies require personalization based on PSA levels, imaging, and patient factors.”
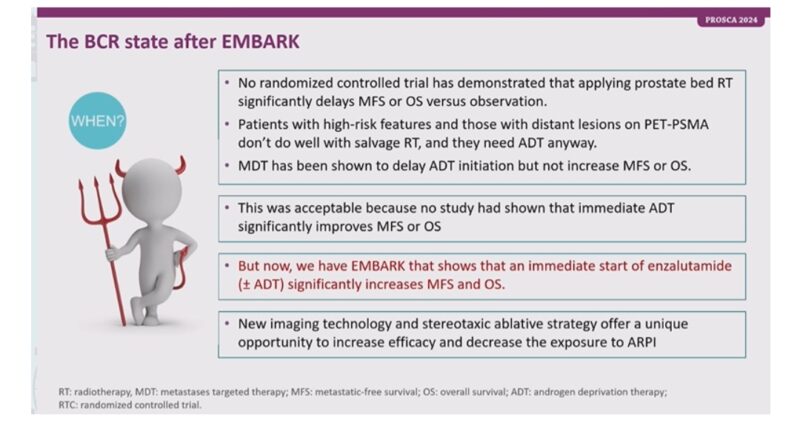
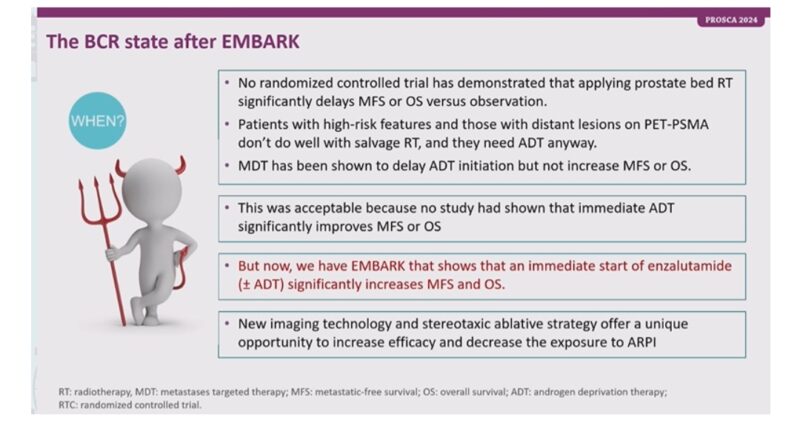
Key takeaways from EMBARK by Bertrand Tombal:
“Amazing session!! by Bertrand TOMBAL at PROSCA24!
Key takeaways from EMBARK:
– EMBARK redefines BCR: Adding enzalutamide + ADT significantly improves metastasis-free survival (MFS) and overall survival (OS).
– Patient benefits: Enzalutamide monotherapy shows significant MFS improvement over ADT alone, paving the way for its role as systemic therapy.
– AE Profile: Combination of enzalutamide and ADT increases grade ≥3 adverse events (31.3%) but remains manageable.
– High-risk outcomes: Patients with PSA doubling ≤9 months benefit most.
– Post hoc insights: Sexual activity-related quality of life remains comparable with delayed TTCD in enzalutamide monotherapy.
– ‘Is it still acceptable to delay enzalutamide initiation in EMBARK patients?'”
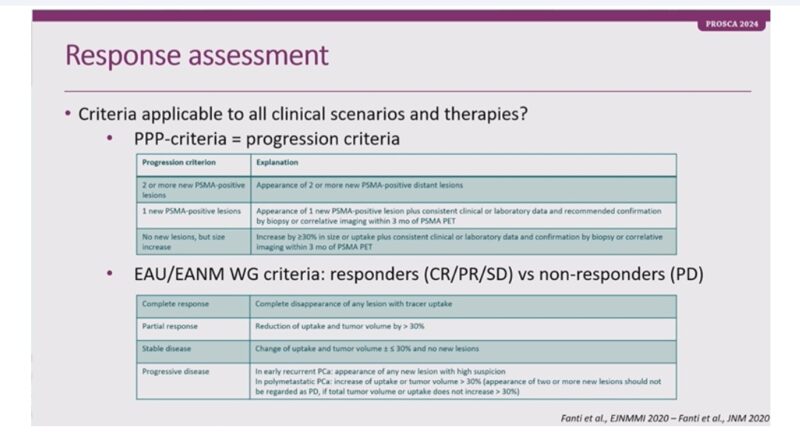
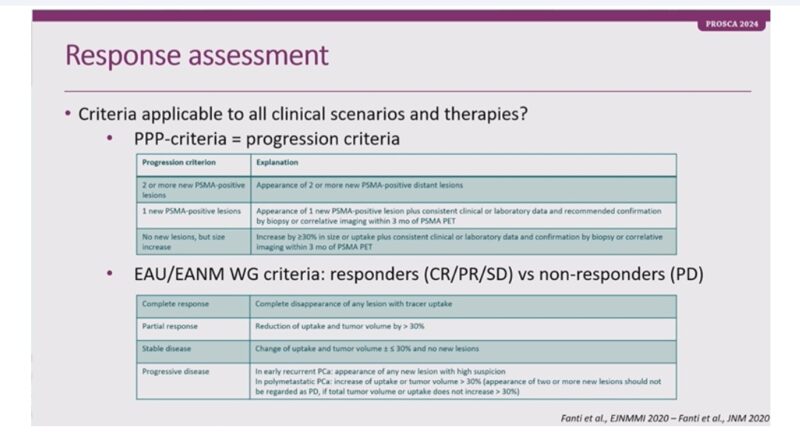
Next generation Imaging in the Metastatic Setting:
“Next generation Imaging in the Metastatic Setting Presented by Karolien Goffin
Moderator: Petros Grivas
PSMA PET: A game-changer!
– Identifies biochemical recurrence early
– Guides therapy selection in oligoprogressive disease
– Monitors response to RLT & predicts survival
Response Evaluation Criteria (RECIP)
– PSMA imaging correlates with Overall Survival (OS)
– Validates new response criteria for mCRPC patients
PSMA PET vs Conventional Imaging
– Superior in detecting micrometastases
– Supports precision oncology approaches
Future directions:
– Standardize imaging for treatment adaptation
– Explore applications in diverse treatment lines
– Transforming metastatic prostate cancer care!”
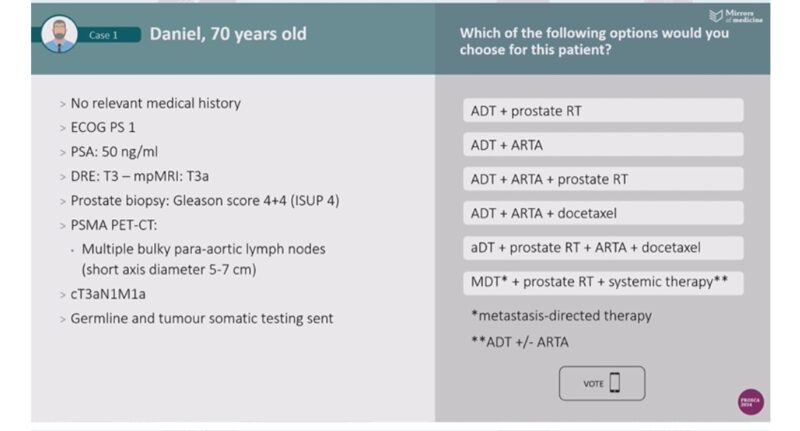
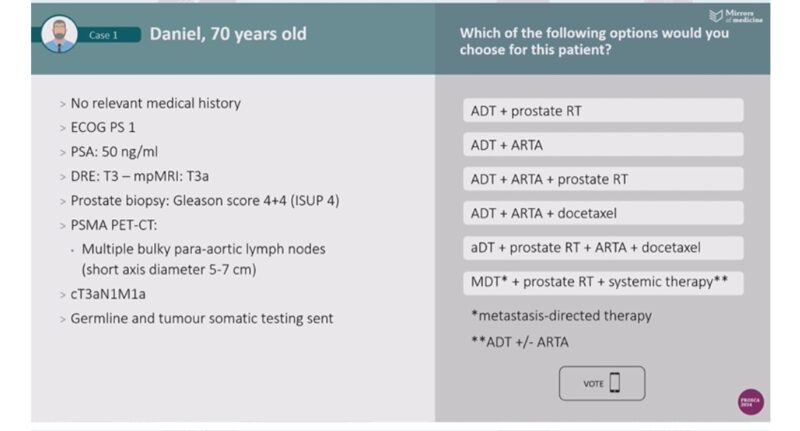
Case Presentation: Managing M1a Disease:
“Case Presentation: Managing M1a Disease
Presented by Amit Bahl, Karolien Goffin | Moderator: Petros Grivas
Daniel, 70 years old
– No comorbidities, ECOG PS 1
– PSA: 50 ng/ml, Gleason 4+4 (ISUP 4)
– PSMA PET-CT: Bulky para-aortic LN (5–7 cm) cT3aN1M1a
Treatment Votes
– ADT + ARTA + Prostate RT led the poll with 44%
– Other options included systemic therapy with docetaxel or MDT.
Panel Discussion Highlights
– MDT + systemic therapy emerges as a promising strategy
– Importance of precision oncology in metastatic prostate cancer.”
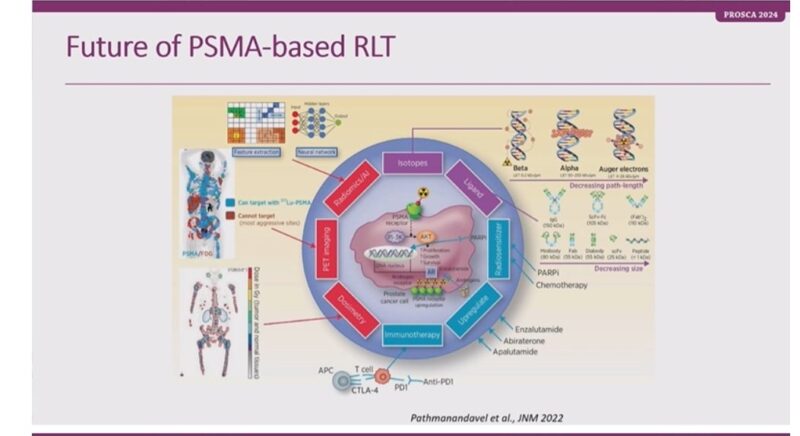
Prostate Cancer (PCa) management in 2025:
“Looking ahead: Prostate Cancer (PCa) management in 2025
Moderator: Amit Bahl | Nuclear Medicine Insights by Karolien Goffin
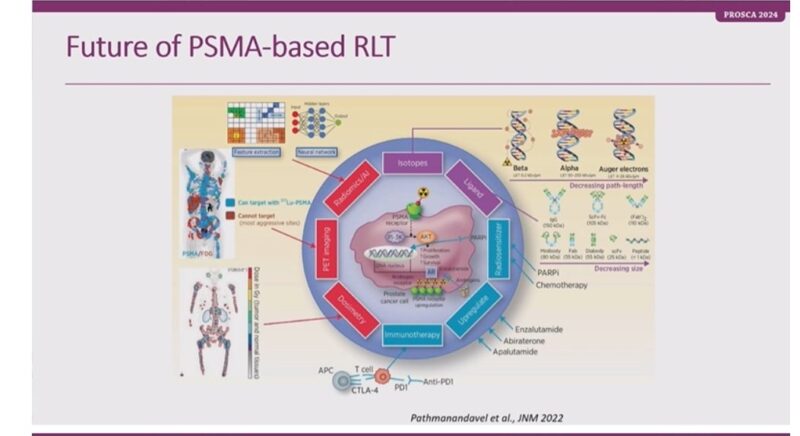
PSMA-based Radioligand Therapy (RLT)
– PSMAfore: 12.0 vs 5.6 months (PFS benefit)
– SPLASH: 9.5 vs 6.0 months (PFS benefit)
– ECLIPSE: Promising outcomes!
Future of RLT
– Integrates isotopes, PET imaging, and immunotherapy
– Exploring alpha therapy: Actinium-225 shows remarkable efficacy!
Innovative Trials in 2025
– Expanding RLT applications globally
– Enhancing targeted treatments with PSMA-based approaches
Beyond Beta
– Lu-PSMA achieves great outcomes-
Alpha therapies (Actinium-225) show groundbreaking potential
Radiation Oncology Evolution. From clinical trials to future standards. Revolutionizing Nuclear Medicine & PCa Treatment!”
Further Reading:
Highlights from RENALC 2024 by María Natalia Gandur Quiroga
Highlights from BLADDR 2024 by María Natalia Gandur Quiroga