Authors: Alan Celik,Tobias Berg, Maj-Britt Jensen, Erik Jakobsen, Hanne Melgaard Nielsen, Iben Kümler, Vesna Glavicic, Jeanette Dupont Jensen, and Ann Knoop.

Published in Breast Cancer: Basic and Clinical Research, Sage Journals on October 4, 2023
Introduction
Metastatic triple-negative breast cancer (mTNBC) is a highly aggressive subtype of breast cancer with a poor prognosis and limited treatment options. New treatment strategies have emerged, but real-world data on treatment outcomes remain scarce. This study aimed to evaluate overall survival (OS) and progression-free survival (PFS) across first to third-line therapies in advanced mTNBC patients, utilizing nationwide real-world data from Denmark.
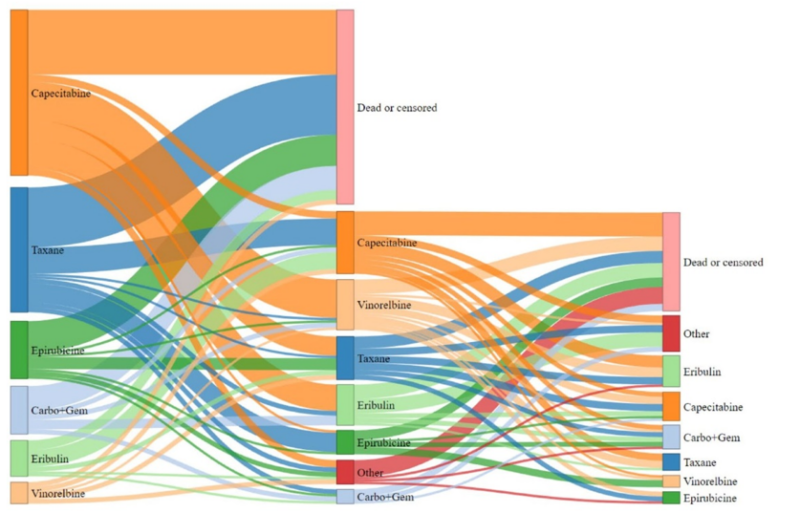
Above is shown a Sankey diagram representing patients’ treatment progression from the first to the third line, with box sizes proportional to the number of patients at each stage.
Design and Methods
This retrospective, non-interventional, multi-site observational study included 243 women diagnosed with metastatic or locally recurrent TNBC between January 1, 2017, and December 31, 2019, from the Danish Breast Cancer Group (DBCG) national database. Patients were followed until death or the last clinical follow-up. Treatment patterns, OS, and PFS were assessed for first-, second-, and third-line treatments using the Kaplan-Meier method.
Results
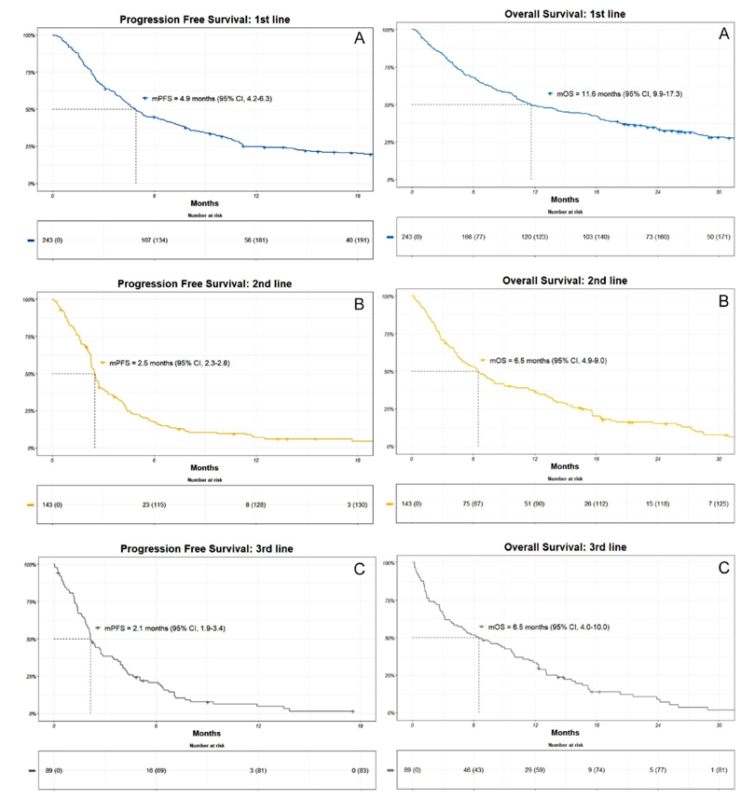
- The median overall survival (mOS) was 11.6 months in the first line, 6.5 months in the second line, and 6.5 months in the third line.
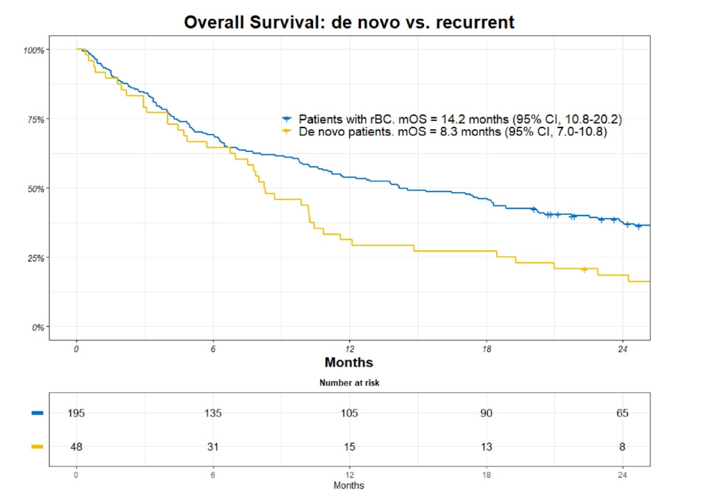
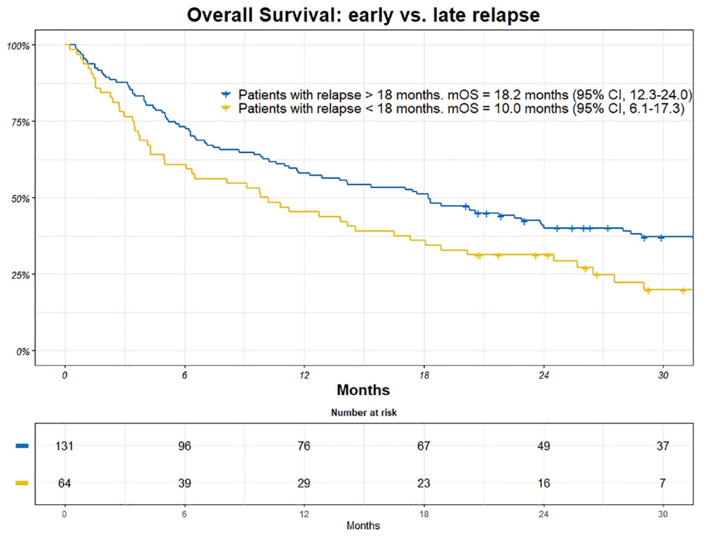
- Patients with de novo mTNBC had shorter OS compared to those with recurrent disease (8.3 vs. 14.2 months). Additionally, patients with early relapse (within 18 months of primary treatment) had worse OS (10.0 vs. 18.2 months).
- Taxane was the most common first-line treatment for de novo mTNBC, while capecitabine was preferred in recurrent cases. Capecitabine remained the most common second-line therapy, and eribulin was the preferred third-line treatment.
- The median progression-free survival (mPFS) was 4.9 months in the first line, 2.5 months in the second line, and 2.1 months in the third line.
What We Learned
- Efficacy: OS was significantly worse for patients with de novo mTNBC and for those who relapsed within 18 months of primary treatment. Treatment efficacy diminished with each successive line of therapy, with shorter PFS and OS in the second and third lines.
- Treatment Patterns: There was substantial variability in first-line treatment, with about half of patients receiving a taxane or anthracycline, and a considerable number receiving capecitabine or other chemotherapies.
Key Highlights
- mOS was significantly worse in de novo mTNBC patients compared to those with recurrent disease, reflecting the aggressive nature of TNBC.
- Patients who experienced early relapse had significantly shorter survival than those with late recurrence.
- The study showed diminishing efficacy of treatments across successive lines, with significantly reduced PFS and OS in second- and third-line therapies.
Below are presented the Kaplan-Meier (KM) estimates for both progression-free survival (PFS) and overall survival (OS). Figure 2 illustrates PFS in the (A) first, (B) second, and (C) third lines, while Figure 3 shows OS estimates for the same treatment lines. Both figures include the number of patients at risk and corresponding median estimates for PFS (mPFS) and OS (mOS) at each stage.
Key Takeaway Messages
- Real-world data indicate poor survival outcomes for advanced TNBC patients, particularly those with de novo disease and early relapse.
- More effective first-line treatments may be needed, and treatment choices should consider the rapid progression of the disease.
- Patients and clinicians should weigh the benefits of additional treatment lines given the diminishing efficacy observed with each successive therapy.
Limitations and Future Directions
- The retrospective design limits the ability to assess causality or patient-reported outcomes like quality of life.
- Future studies should explore the integration of newer therapies (e.g., immunotherapy) and assess long-term outcomes, including real-world quality of life.
Conclusion
This study highlights the poor prognosis for patients with metastatic or recurrent TNBC, particularly those with de novo mTNBC or early relapse. The findings underscore the need for more effective first-line therapies and comprehensive, real-world evidence to inform treatment strategies for this aggressive disease.


