Imagine climbing a Himalayan peak. The air gets thinner, and your body has to work harder just to get enough oxygen. Over generations, some populations—like Tibetans and Sherpas—have developed special genetic tweaks to survive in these extreme conditions. Interestingly, tumors can hijack some of these same genetic adaptations to help them thrive in low-oxygen environments, like those found deep within the body.
Now, imagine a tumor trying to do the same thing.
Surprisingly, that’s not just a metaphor—it’s the focus of a groundbreaking new study that reveals a deep, almost poetic connection between how our bodies adapt to low oxygen in nature and how cancers evolve under similar stress.
Photo from VHIO/X
The Star of the Show: EPAS1
At the center of this story is a gene called EPAS1, famously dubbed the “super-athlete gene” because of its role in helping high-altitude populations cope with hypoxia (low oxygen). It helps regulate how cells respond when oxygen is scarce.
The researchers behind this study discovered that EPAS1 doesn’t just help climbers—it helps cancer cells, too.
In certain tumors, particularly pheochromocytomas and paragangliomas (PPGLs)—rare cancers that arise from nerve tissue—EPAS1 mutations are shockingly common, especially in people with a lifelong history of low oxygen, such as those born with congenital heart defects.
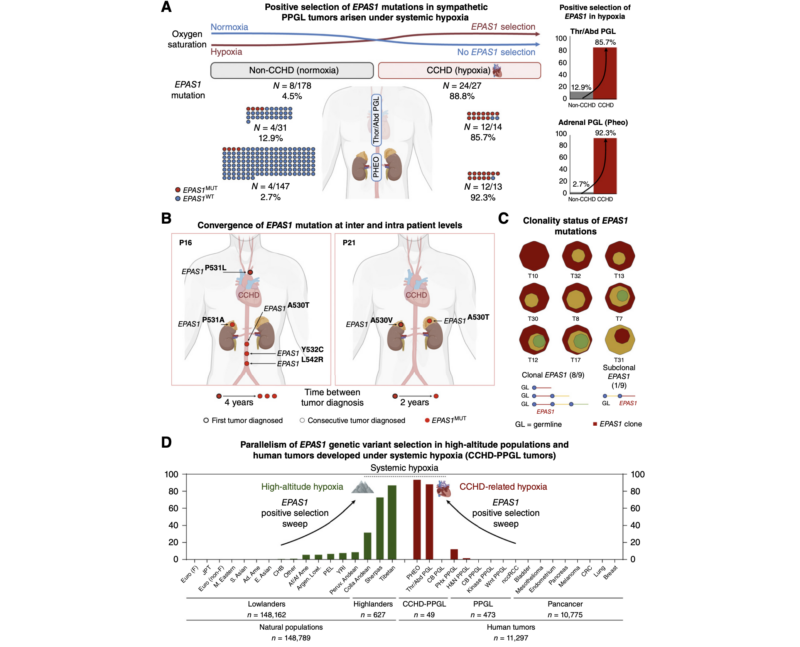
Photo from silverchair.com
When the Body is Born Into Thin Air
People with congenital cyanotic heart disease (CCHD) have hearts that don’t oxygenate blood efficiently. That means their entire body lives in a kind of permanent high-altitude simulation. The study looked at nearly 2,600 such patients and found a striking trend: those who developed PPGL tumors almost always had mutations in EPAS1—nearly 89%, compared to just 4.5% of people without chronic hypoxia.
And these mutations aren’t just random. They seem to be the very first events that start the cancer process, acting like a spark that lights the fuse.
What Happens When Oxygen Is Scarce
Under low oxygen conditions, EPAS1 becomes hyperactive. This leads to the activation of genes like COX4I2, which help cells survive by using oxygen more efficiently—not to make energy, but just to get by. It’s a smart but sneaky trick, one that tumors have co-opted to thrive in otherwise lethal environments.
The study found that this isn’t just a one-off mutation—it’s an evolutionary strategy. In both high-altitude humans and cancer cells, EPAS1 is shaped by powerful natural selection, helping the organism—or tumor—adapt and grow under stress.
But There’s a Price to Pay
While helpful in the short term, this adaptation has downsides. In tumor cells, chronic hypoxia disrupts DNA repair, allowing more mutations to pile up. In fact, EPAS1-mutated tumors showed high genetic instability, with defects in key repair proteins like MLH1 and PMS2.
This leads to faster tumor evolution, more aggressive behavior, and greater resistance to treatment.
Not All Tumors Are Equal
Interestingly, EPAS1 mutations were found only in sympathetic PPGLs, which come from adrenal tissue, and not in parasympathetic tumors, like those in the neck (carotid body tumors). Even in people with the same chronic hypoxia, the timing and type of tissue mattered—a key clue that tumor risk depends on both when and where the oxygen shortage hits.
The Altitude Connection: A Shared Blueprint
Here’s where the story becomes truly extraordinary.
The exact same EPAS1 gene variations that help Tibetans and Sherpas live high above sea level are echoed in the mutations seen in these tumors. It’s as if cancer cells are borrowing a page from humanity’s high-altitude survival playbook. This suggests that our evolutionary history may also shape how diseases like cancer arise—and perhaps how we can treat them.
Hope on the Horizon: New Treatments
There’s more good news. The study points to Belzutifan, a drug that blocks EPAS1 activity, as a promising treatment for these tumors. In early case reports, it has already shown success in shrinking tumors and easing symptoms.
Even more exciting? This research opens doors to other potential therapies—like PARP1 inhibitors—that target the weak spots left behind by this adaptation strategy.
A New Way to Think About Cancer
This study is a powerful reminder that cancer isn’t just chaos—it’s evolution in action. Tumors adapt to their environment just like any living thing does. And if we can understand the rules of that game, we might find new ways to beat it.
By studying how humans adapted to the sky-high peaks of Earth, scientists are uncovering clues to how tumors survive in the low-oxygen niches of our bodies.
Sometimes, nature’s toughest environments teach us the most about life—and disease.
Information primarily sourced from the article “Convergent Genetic Adaptation in Human Tumors Developed Under Systemic Hypoxia and in Populations Living at High Altitudes” published in Cancer Discovery journal.
What are your thoughts on this advancement?
We’d love to hear how this could impact your practice, research, or advocacy work.
For more insights into the latest in oncology—from breakthrough therapies to expert interviews—follow OncoDaily and stay connected to the pulse of global cancer care.
By: Md Foorquan Hashmi, MD, Sr. Editor, OncoDaily: India Bueura