Sebastian Schmidt, Head of Medical Affairs Computed Tomography at Siemens Healthineers, shared a post on LinkedIn:
“Lung cancer screening and overdiagnosis (2 of 2).
As promised, the second part of my comments on the recent BMJ article.
One more misunderstanding is that they mix up screening and commercial “body checkups”. Writing about screening, they don’t show any data from screening programs. Data for Korea ends in 2019, the year when Korea started screening. As a result, none (zero) none of the data is actually from quality-controlled screening programs.
Why does it matter?
For the ones not familiar with the Asian “body checkups: Commercial entities offer self-paid CT scans – you pay a fee, e.g. about 20-30 Dollar in China, and get a chest CT. In several countries, this is a significant business. Frequently also part of company health benefits.
However, this is not screening. This is not an organized and quality-controlled program – guideline adherence is low, there are no inclusion and exclusion criteria, no radiation dose control, little quality control, and in case of a finding, the patient is simply sent to the next hospital.
What the authors do, is presenting data from these unstructured body checkups and talk about screening. This is mixing up different things.
They also mix it up in the other direction: They come to the conclusion that screening should not be done in non-smokers unless randomized clinical trials exist. This won’t have an effect, as, again, we are talking about different things: There are almost no screening programs for non-smokers (with only one small exception in Taiwan for non-smokers with family history). But this has no (zero) influence on “body checkups”. Two different things. RCTs and scientific papers will not change the current practice in these checkups.
What’s the background?
The challenge are cancers formerly known as BACs (Brochoalveolar Carcinoma – an old term, currenty known as LPA, IAS, MIA). These are slow-growing cancers, and as I wrote previously, slow growing cancers always carry the risk that the patient dies from something else before (called “overdiagnosis”). These should be watched for a longer time to avoid overtreatment (“watchful waiting”, we call it in prostate cancer, which is another slow-growing cancer). These cancers typically present as ground-glass opacities (GGOs) in CT. That is why current guidelines handle these carefully – e.g. in LungRads, a GGO is LungRads 3 and only gets follow-up CT, until it shows growing solid parts. A LungRads 3 will not be diagnosed as cancer – it will be followed up.
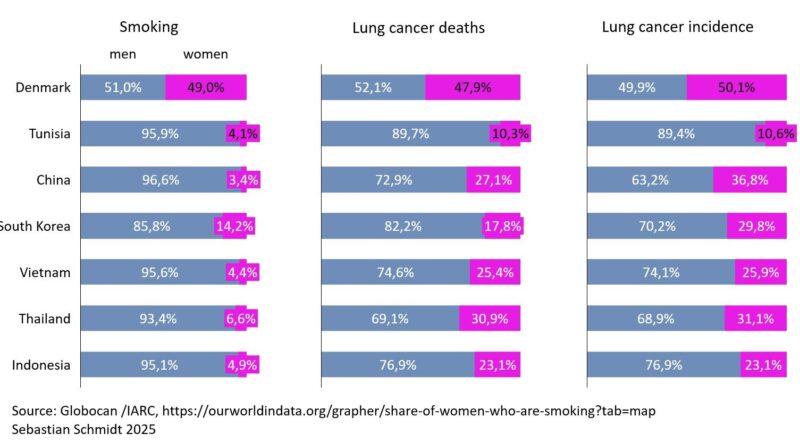
BACs are rare in smokers (8% or less of lung cancers), but common in Asian never smokers (30% or more). If you take invasive actions on them too quickly, you create harm. A large portion of this is mitigated, however, if you follow current guidelines, which greatly improved in the 25 years since NLST.
Let’s address what we can improve: Avoidance of overtreatment through guideline adherence.”